First aid
- 1. FIRST AID
- 2. Introduction • Aperson who gives treatment for the one suffering from a disease or an accident, to improve his condition is called an” aides” and the medical treatment given as aid is called “ first aid”. • If an accident happens in the workplace, you cannot be a helpless witness, since simply standing by can potentially worsens the situation. This is why it’s important to have at least a basic knowledge of first aid. • At its most basic, first aid is the initial assistance given to a victim of injury or illness. Comprised of relatively simple techniques that can be performed with rudimentary equipment, first aid is usually carried out by a layperson until professional medical assistance arrives.
- 3. Definition of first aid • First aid is the provision of immediate care to a victim with an injury or illness, usually effected by a lay person, and performed within a limited skill range. • First aid is normally performed until the injury or illness is satisfactorily dealt with (such as in the case of small cuts, minor bruises, and blisters) or until the next level of care, such as a paramedic or doctor, arrives. • First aid is an emergency aid or treatment given to someone injured, suddenly ill, etc., before regular medical services arrive or can be reached.
- 4. Objectives of first aid/guiding principle The key guiding principles and purpose of first aid, Prevent further injury Preserve life Promote recovery To help to ensure safe transportation to the nearest healthcare facility.
- 5. Philosophy of First Aid • In the pre-hospital setting, the key contributors to survival and recovery from illness and injury are prompt and effective maintenance of the body’s primary functions: 1. Airway 2. Breathing 3. Circulation 4. Bleeding control (life threatening)
- 6. Importance of first aid The importance of first aid is hard to overestimate. Among the major benefits of first aid are the following: • Providing quick medical treatment until professional assistance arrive. • First aid helps ensure that the right methods of administering medical assistance are provided. • Knowledge in first aid also benefits the individuals themselves. • It affords people with the ability to provide help during various emergency situations.
- 7. Principles of emergency care • Collect the detailed history of accident either from the victim or from anyone who has witnessed the accident. • The victim’s injury should be examined thoroughly, taking note of every symptom, to know the correct diagnosis. • By the help of the diagnosis, treat the victim until the doctor arrives or shift the victim to the hospital and aid the patient during transport. • Call the doctors or shift the victim to the hospital as soon as possible, so that the patience can recover soon from doctor’s treatment instead of prolonging the first aid.
- 8. Golden rule’s of first aid. Do first things first quickly, quietly and without fuss or panic. Give artificial respiration if breathing has stopped-every second counts. Stop any bleeding. Guard against or treat for shock by moving the casualty as little as possible and handling him gently. Do not attempt too much-do the minimum that is essential to save life and prevent the condition from worsening. Reassure the casualty and those around and so help to lessen anxiety. Do not allow people to crows round as fresh air is essential. Do not remove clothes unnecessarily. Arrange for the removal of the casualty to the care of a Doctor or hospitals soon as possible.
- 9. Content of the first aid kit
- 10. FIRST AID IN EMERGENCIES
- 11. Shock What causes shock to occur? Anything that affects the flow of blood through your body can cause shock. Some causes of shock include: Severe Allergic Reaction Significant Blood Loss Heart Failure Blood Infections Dehydration Poisoning Burns Sepsis Shock is a life-threatening medical condition as a result of insufficient blood flow throughout the body. Shock often accompanies severe injury or illness.
- 12. Signs/Symptoms: Unusual behavior (e.g. Very calm or very anxious), Lack of pain to an injury Rapid breathing Rapid but weak pulse Bluish skin (cyanosis) Unconsciousness. Management: Activate the ambulance right away. Assist the person to lie on their side to improve circulation, treat any injuries help them take any medication for an illness.
- 13. Burns Definition:A burn is damage to the skin or underlying tissue caused by heat. There are 3 levels of severity; 1st (Superficial), 2nd (Partial thickness), 3rd (Full thickness). Causes: There are 5 main sources of burns; Electricity, Radiation (sun), Thermal (something hot), Chemical, Friction Prevention: Use safety rules. Use safety equipment when working with chemicals. Hire professionals for work dealing with e.g. electricity. Avoid sun exposure. Keep hot objects away from children.
- 14. DEGREE OF BURNS 1st Degree The skin is red and painful with some minor damage, but no blisters; think sunburn. 2nd Degree The skin is red, blistered, swollen, and painful. The burn area might also look wet and shiny or be white/discolored in an irregular pattern. There is no nerve damage in 2nd degree burns. 3rd Degree The skin has been burned all the way through. It may be dry and leathery to touch and change color to black, white, brown, or yellow. The burn will feel numb because nerve endings have been destroyed. Skin will not regrow because the cells responsible for regrowth have been destroyed.
- 16. 3rd Degree
- 17. Management • For 1st and 2nd degree burns you should cool the area immediately with gently running cold water for about 10-15 minutes, or until it has cooled off. Do not break any blisters as this will make the wound worse. • For 3rd degree burns do not put anything on the burn, seek medical help immediately and treat for shock. 3rd degree is extremely life threatening even when a small body part is affected. • If there is clothing on the burn do not remove it as this may also remove skin. • There is a very high risk of infection from this kind of burn.
- 19. Snake-bite
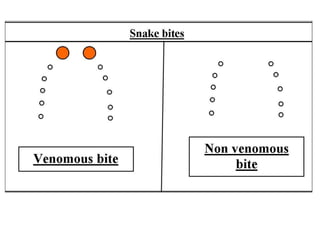
- 20. Snake Bites Definition A physical puncturing wound caused by the fangs of a venomous/non-venomous snake leading to a bunch of symptoms like pain and vomiting, paralysis and sometimes death, qualifies as a snake bite. Snake Bites Symptoms Two fang marks look punctured Bleeding from the wound Localized Inflammation Burning and redness around the bite Tremendous pain around the bite Change in skin color Diarrhoea and fever Difficulty in breathing Nausea and vomiting Shock and Convulsions Allergic reactions Vision going blurry Paralysis Rapid pulse Tiredness and muscle weakness Numbness and tingling in the limbs and the face, and drooping eyelids Thirst Low Blood pressure
- 23. Snake Bites Risk Factors The major risk factors associated with snake bites are the following – a) Lack of immediate and scientific first aid in the form of anti-venom. b) Too much movement of the victim can cause the venom to spread faster in the body. c) Tight and fitted clothing and jewellery around the bite. d) Outdated first aid techniques like cutting the wound open and exposing to infection and complication, using tourniquets or cold compress, manually sucking the venom out or using pump suction device, pain killers without the doctor. e) Children run the risk of death and serious complications because of their smaller body size.
- 24. a) Note the snake's appearance. b) Be ready to describe the snake to emergency staff while waiting for medical help. c) Move the person beyond striking distance of the snake. d) Have the person lie down with wound below the heart. e) Keep the person calm and at rest, remaining as still as possible to keep venom from spreading. f) Cover the wound with loose, sterile bandage. g) Remove any jewelry from the area that was bitten. h) Remove shoes if the leg or foot was bitten. a) Cut a bite wound b) Attempt to suck out venom c) Apply tourniquet, ice, or water d) Give the person alcohol or caffeinated drinks or any other medications. Do not: Snake Bites Treatment and First Aid
- 27. Broken bones and fractures Definition: A break or crack in a bone is called a fracture. In most cases the damage to the bone will be under the skin, which is called a closed fracture. But sometimes bits of the bone can puncture through the skin to become an open fracture. In both cases you'll need to treat the casualty for shock. Even if you can't see any blood, the break might have caused some internal bleeding. To break a fully grown bone, a huge amount of force is needed But bones that are still growing are supple and can split, crack or bend quite easily, a bit like a twig.
- 28. Fracture Signs: The seven things to look for are: Swelling Difficulty moving Movement in an unnatural direction A limb that looks shorter, twisted or bent A grating noise or feeling Loss of strength Shock
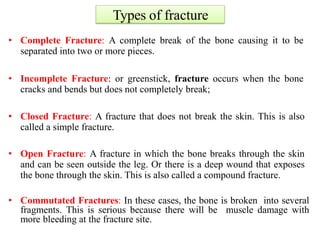
- 29. Types of fracture • Complete Fracture: A complete break of the bone causing it to be separated into two or more pieces. • Incomplete Fracture: or greenstick, fracture occurs when the bone cracks and bends but does not completely break; • Closed Fracture: A fracture that does not break the skin. This is also called a simple fracture. • Open Fracture: A fracture in which the bone breaks through the skin and can be seen outside the leg. Or there is a deep wound that exposes the bone through the skin. This is also called a compound fracture. • Commutated Fractures: In these cases, the bone is broken into several fragments. This is serious because there will be muscle damage with more bleeding at the fracture site.
- 30. Open Fracture
- 31. Types of fracture • Impacted Fractures:After a heavy fall, the fracture may be impacted by the force, (eg.) Spinal injury falling from tree. • Pathological Fractures: These occur when the bone is weakened by loss of calcium, infection or cancer. Minimal cause a break in such cases. In old age the bones are more brittle, and may break spontaneously due to calcium loss which is part of the ageing process. • Stress Fractures: Stress caused by repeated minor trauma as in athletic training. Involved in strenuous training, such as jogging or marathon running.
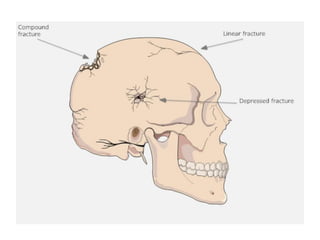
- 36. linear skull fractures Depressed fracture of skull compound skull Fracture
- 37. Management a) If it is an open fracture, cover the wound with a sterile dressing and secure it with a bandage. Apply pressure around the wound to control any bleeding. b) Support the injured body part to stop it from moving. This should ease any pain and prevent any further damage. c) Once you’ve done this, call medical help. While waiting for help to arrive, don’t move them unless they’re in immediate danger. d) Protect the injured area by using bandages to secure it to an uninjured part of the body to stop it from moving. For example, fractures on the arm can be secured with a sling, and a leg with a fracture can be tied to the uninjured leg. e) Keep checking the casualty for signs of shock. This does not mean emotional shock, but is a life-threatening condition, often caused by losing blood. f) If they lose responsiveness at any point, open their airway, check their breathing and prepare to treat someone who’s become unresponsive.
- 39. •
- 40. Poisoning • Definition: A poison is a substance which enters the body and can cause illness or death. • It may act within a matter of seconds (e.g. carbon monoxide) or a matter of years (e.g. car pollution). • There are four basic ways in which poison can enter the body;- by swallowing, breathing, injecting, or absorbing. Any of these methods can be life threatening. • Many times children are the innocent casualties.
- 43. Breathed/Inhaled Poisons: This can include fumes from household cleaners, industrial products, smoke, etc. Fresh air is the immediate first aid treatment. But first make sure you are not putting yourself in danger. Seek medical help for the person immediately. Never use chemicals in poorly ventilated areas. Be aware of carbon monoxide as it can not be smelled, has no taste, and can not be seen. It can be produced by any engine (e.g. house furnace, car), or even a fireplace with poor ventilation. Every home should have a carbon monoxide detector. If the detector begins to sound you need to leave the house immediately and call the fire department from the neighbor’s house. Carbon monoxide poisoning makes you feel sleepy and drowsy and can have an effect in a matter of minutes so you aren’t aware of what is happening.
- 44. Ingested Poisons
- 45. Ingested Poisons- Examples can include bad food, household cleaners, perfumes, nail polish remover, etc. If the person is having trouble breathing, is convulsing, is unconscious, or is in pain, call the ambulance immediately. If the person appears to be fine but you want to make sure call your doctor or local hospital. Make sure you do not induce vomiting unless you are told to do so by a physician as some substances are corrosive and may burn on the way up. Also, do not give anything to drink unless instructed by a physician as some substances may react more with liquids. Always keep cleaners and chemicals high up so children can not access them.
- 46. Injected Poisons: Some examples include needles, broken glass, mosquitoes, spider bites, bee stings, etc. As soon as possible remove the object from the skin. Clean the area thoroughly with soap and water. If an allergic reaction occurs, or you believe there is a risk of infection, seek medical help.
- 47. Absorbed Poisons: These are poisons which enter the body through the skin, but do not cause a puncture. Some examples are household cleaners, industrial products, poisonous plants, etc. Remove the substance as soon as possible by using large amounts of running water. Do your best not to contaminate other body parts. There are some chemicals that will react more with water, but if you leave them on the skin they will react anyway with skin moisture. Seek medical help. If you work with chemicals make sure you know how to do the job safely and always use safety equipment.
- 48. Common household poisons that can harm babies and children: Nail polish and nail polish remover. Lipstick and lip gloss. Mascara. Medication including: Panadol, Tylenol, Aspirin. Vitamins or other supplements. Cleaning supplies: e.g. bleach. Aerosols and other insect repellents. Poisons used for insect and pest control. Soaps: dishes, hands, clothes, etc. Smoke from smoking.
- 49. Swollen mouth or throat Vomiting / diarrhea Irregular heartbeat Dilated pupils Difficulty breathing Pale gums Swollen abdomen Muscle tremors Hyperactivity / weakness Bloody / painful urination or defecation Bleeding from any orifice Confusion Restlessness / pacing Blindness Paralysis Seizures Coma Cardiac arrest. Here are typical symptoms of poisoning:-
- 50. Take the following actions until help arrives: Swallowed poison. Remove anything remaining in the person's mouth. If the suspected poison is a household cleaner or other chemical, read the container's label and follow instructions for accidental poisoning. Poison on the skin. Remove any contaminated clothing using gloves. Rinse the skin for 15 to 20 minutes in a shower or with a hose. Poison in the eye. Gently flush the eye with cool or lukewarm water for 20 minutes or until help arrives. Inhaled poison. Get the person into fresh air as soon as possible. If the person vomits, turn his or her head to the side to prevent choking. Begin CPR if the person shows no signs of life, such as moving, breathing or coughing. Have somebody gather pill bottles, packages or containers with labels, and any other information about the poison to send along with the ambulance team.
- 51. Heart Attack
- 52. Heart Attack Signs/Symptoms: Pain/tightness/numbness in the shoulders, arms, neck, back, chest. Bluish, pale skin. Rapid but weak pulse. Shallow rapid breathing. Nausea or vomiting. Unconsciousness. These warning signs may come and go, and maybe severe or mild. Even if the warning signs go away this person may still be having a heart attack and still needs immediate help. Definition: When something goes wrong with the heart’s electrical system, or when an artery in the heart muscle ruptures or becomes blocked. Regardless, the heart is no longer able to circulate blood effectively, including to its own tissues. As a result, the heart may stop working.
- 54. • Strict bed rest. • Help them get in a comfortable position, make sure they are resting. • Activate the ambulance, Reassure them that help is on the way. • Check for medical history of a similar problem, as they may have medication (but only assist, do not administer medication). • Do not give them anything to eat or drink. • Stay with them all the time and comfort them. • If oxygen is available it should be given. • It is extremely common for people to ignore the warning signs of a heart attack. Unfortunately, this is one reason why so many people die from this disease because they don’t get help soon enough. • As a first aider it is your job to activate the ambulance as soon as possible. Management
- 56. Angina Definition: • Angina is a serious medical condition, diagnosed by a cardiologist, where the coronary arteries are partially blocked. As a result, when under stress, the heart is not able to get enough blood and cannot work properly. Sign/Symptoms: Shortness Of Breath Nausea Fatigue Dizziness Profuse Sweating Anxiety Risk factors for stable angina include: Being Overweight Having A History Of Heart Disease Having High Cholesterol Having Diabetes Smoking Not Exercising
- 57. • Nitroglycerine comes in 4 forms: Pill: which they must place under their tongue for quick absorption. If they swallow the pill it will take much longer to be absorbed. Spray: like a puffer, which they spray into their mouth. Paste: which they put on their skin. Patch: which they wear all day. • The most they should take is 3 doses, 3 minutes apart each. If after 10 minutes they do not feel better, or they become worse at any time then it means the medication is not working and this person needs advance medical help immediately. Management
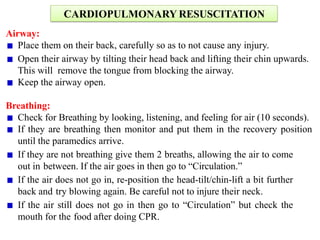
- 59. CARDIOPULMONARY RESUSCITATION Airway: Place them on their back, carefully so as to not cause any injury. Open their airway by tilting their head back and lifting their chin upwards. This will remove the tongue from blocking the airway. Keep the airway open. Breathing: Check for Breathing by looking, listening, and feeling for air (10 seconds). If they are breathing then monitor and put them in the recovery position until the paramedics arrive. If they are not breathing give them 2 breaths, allowing the air to come out in between. If the air goes in then go to “Circulation.” If the air does not go in, re-position the head-tilt/chin-lift a bit further back and try blowing again. Be careful not to injure their neck. If the air still does not go in then go to “Circulation” but check the mouth for the food after doing CPR.
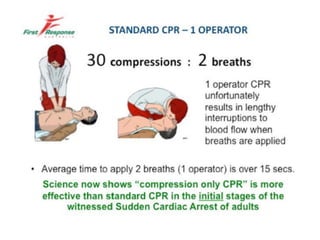
- 60. Circulation: Start CPR if needed (compressions and breaths). It is 30 compressions to 2 breaths. Continue until paramedics arrive or until something changes with the person (reassess at this point). If the air was not going in make sure you check the mouth, to see if the food came out, after each set of compressions. If you see the object in their mouth take it out and reassess breathing. Under this category, we are also concerned with shock and severe bleeding. About compressions: Adult: use both hands. Compress 4-5 cm deep. Child: use one hand. Compress almost half way down. Infant: use two fingers. Compress almost halfway down. Fast and smooth. Do not stop unless something changes. Ribs may break, keep going. If they vomit roll them onto their side, clean their mouth, continue.
- 62. Two-Rescuer CPR: In a situation where there are 2 trained first aiders, and they work well together, one rescuer can perform the compressions while the other rescuer gives the breaths. All the steps are the same, nothing changes. This is a bit more sufficient and less tiring for the rescuers. If the rescuer doing the compressions becomes tired they can switch positions.