General Practice Transformation Champions: Lessons from the front line
- 1. Dr. Paul Deffley Lessons from the front line. What we have learnt about at scale working whilst building GP hubs
- 2. Intentions For The Session • To understand what is happening across the country • To reflect on the key learning points from our work • To have an opportunity to discuss with colleagues • To consider what your next steps are and where to find support
- 3. About Here Formerly known as Brighton and Hove Integrated Care Services Not-for-profit social enterprise Membership organisation (our members are local GPs, Practice Managers, Practice Nurses and our own staff) Annual turnover of £50 million Partnered with local practices Delivering a broad range of NHS Services Supporting primary care since 2008 and testing new ways of working
- 4. Working at Scale • Working at scale in collaborative arrangements is widely accepted as the future of general practice • Collaboration in General Practice survey 2017 • 81% GP practices part of collaboration (up from 73% 2015) • 45% federations • 53% covering >100,000 people
- 5. Working at Scale • But…. • Over half of GPs and a third of CCG staff felt practices and collaborations had not been at all influential in shaping STP strategy • Only 1/5 of GPs thought STPs would deliver change in primary care • 53% (very) unwilling to give up GMS/APMS • Complicated picture: - • Many work in multiple collaborations • One size does not fit all
- 6. Working at Scale • What is happening across the country? • One third collaborations reported achieving their goal to improve access • One in ten had fully achieved goal of improved sustainability
- 7. Conversation point Imagine a successful, connected group of practices, sharing resources and service delivery… What are the benefits of this? What’s stopping you?
- 8. Challenges to GPs Working at Scale • Trust • Engagement • Time and work pressures ‘No corporation or practice can thrive in the absence of creativity, innovation and learning and the greatest threat to all three of these is disengagement’.
- 9. Our Journey – Workflow and Understanding Scale
- 10. Case Study – Sackville Medical Centre, Hove
- 12. Our Journey – Hub development
- 13. Our Journey – Hub development Engagement Protocol design Data Safety Business governance Learning Implement Sustain
- 14. Invest in time together
- 16. Identify local leaders and delegate swiftly
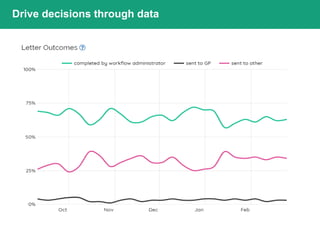
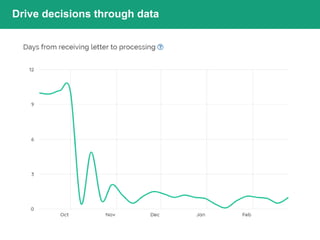
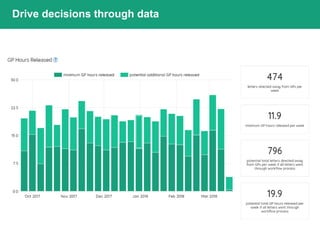
- 17. Drive decisions through data
- 18. Drive decisions through data
- 19. Drive decisions through data
- 20. Drive decisions through data
- 21. Supporting GP at scale (CCG, Fed, PCH View)
- 22. Safety
- 25. What we are seeing in the system • Keeping people connected whilst they learn • Clear over time what the solutions are • This is the transformation space
- 26. Resources/further reading • https://gpatscale.rcgp.org.uk/ • https://www.nuffieldtrust.org.uk/ news-item/general-practice-at- scale-is-it-working-for-front- line-gps • https://www.nuffieldtrust.org.uk/ our-priorities/new-models-of- health-care-delivery/
- 27. Discussion – about the why Thank you for your participation… Any questions, thoughts or reflections on the information and conversation about General Practice at scale?
- 28. Fourth Floor, 177 Preston Rd, Brighton, BN1 6AG +44 (0)1273 560 243 pauldeffley@nhs.net
Editor's Notes
- Simple slide to ensure people have a sense of purpose for the session
- https://www.nuffieldtrust.org.uk/research/is-bigger-better-lessons-for-large-scale-general-practice What is happening across the country? This agenda is well underway across the country, with almost three-quarters of general practices already in some form of collaboration with others, almost half of which formed during 2014/15. The major reasons for forming were to ‘achieve efficiencies’ and ‘offer extended services in primary care’. Larger scale has the potential to sustain general practice through operational efficiency and standardised processes, maximising income, strengthening the workforce and deploying technology. However, scaling up will take a lot of hard work and cannot just be left to a few heroic leaders. All GPs will need to play a part in making these new organisations successful.
- https://www.nuffieldtrust.org.uk/research/is-bigger-better-lessons-for-large-scale-general-practice
- Larger scale has the potential to sustain general practice through operational efficiency and standardised processes maximising income strengthening the workforce deploying technology. No single model that can be implemented throughout the country Each organisation must evolve to meet the needs of its local population Data can be used to improve the care patients receive without increasing the burden on primary care professionals
- Larger scale has the potential to sustain general practice through operational efficiency and standardised processes maximising income strengthening the workforce deploying technology. No single model that can be implemented throughout the country Each organisation must evolve to meet the needs of its local population Data can be used to improve the care patients receive without increasing the burden on primary care professionals
- https://gpatscale.rcgp.org.uk/discussions/culture-eats-strategy-breakfast/#.WjkyU9Jl-M8 GPs and CCGs agree that collaborations are likely to be ready to hold budgets for selected community services in the near future. Collaborations will need to think carefully, but positively, about their governance arrangements to enable this. GP engagement with their STPs may need to be re-examined quickly to develop better buy in. Further discussions about options for contractual models may also be needed, as a majority of GPs said they would be unwilling to change to a new contract.
- Introduction to workflow Design principles Approach to learning Confirmation practices through data
- The current reality with documents Are we really doing the best job for the people we serve?
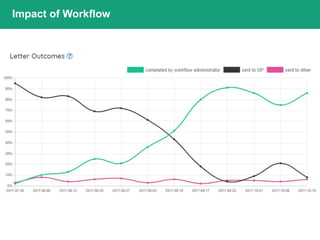
- How will you know it’s working? Data from a typical practice we trained We know some practices where the cross over happened much sooner – depending on skill, they may already doing workflow to an extent already. Describe the layout so everyone knows it represents Letters / Timeframes / Person Black line - letters sent to GP Green line – letters completed by Administrator Pink line - letters sent to others , for example, Pharmacist or Nurse As you can see, as this practice hit 8 weeks post training, they had passed over 50% of their clinical correspondence to their administration team. Following an implementation plan which follows letter types that are a combination of high frequency and ease of completion A&E 111s Screenings Implementation slows down as administrators move onto more complex letter types
- Engagement GP protocol design Data to create demand and capacity Code sign local governance structures Shared decisions Conflict resolution Empowering teams and understanding when to seek advice Implementation plan using data E-learning and physics go live Support Data to demonstrate impact and understand what is the next question to answer Communication and learning
- I’m showing this so you get a sense of just how much information the Dashboard can give you and what it allows you to do Appreciate its difficult to read – see Handout The Dashboard is useful as it… As primary care physicians we know our own communities well and live daily with the tension between providing continuity of care and meeting the accessibility they need, whilst working in practices stretched by workforce challenges and rising demand. It seems essential therefore that for GP at Scale to develop in any area, organisations will need good data on the health needs of their local population upon which to base any new care models, as the Nuffield Trust projects are demonstrating – including in the Valentine medical group. This will mean that working at scale can improve the care patients receive without increasing the burden on primary care professionals Allows the auditing process to happen, and provides your PM / GP Lead insight on Workflow Administrators training needs. Track implementation of workflow for your practice, including percentage of letters being completed by a clinician vs. administrator Help measure the impact of Workflow across the practice including the workload of clinicians and administrators Support you to identify which letter types to tackle next Provide clear data on the types, shapes and volume of demand of clinical correspondence, allowing engagement with your hospitals and providers to influence change in the future Will pick out a few graphs to introduce you to……
- I’m showing this so you get a sense of just how much information the Dashboard can give you and what it allows you to do Appreciate its difficult to read – see Handout The Dashboard is useful as it… As primary care physicians we know our own communities well and live daily with the tension between providing continuity of care and meeting the accessibility they need, whilst working in practices stretched by workforce challenges and rising demand. It seems essential therefore that for GP at Scale to develop in any area, organisations will need good data on the health needs of their local population upon which to base any new care models, as the Nuffield Trust projects are demonstrating – including in the Valentine medical group. This will mean that working at scale can improve the care patients receive without increasing the burden on primary care professionals Allows the auditing process to happen, and provides your PM / GP Lead insight on Workflow Administrators training needs. Track implementation of workflow for your practice, including percentage of letters being completed by a clinician vs. administrator Help measure the impact of Workflow across the practice including the workload of clinicians and administrators Support you to identify which letter types to tackle next Provide clear data on the types, shapes and volume of demand of clinical correspondence, allowing engagement with your hospitals and providers to influence change in the future Will pick out a few graphs to introduce you to……
- I’m showing this so you get a sense of just how much information the Dashboard can give you and what it allows you to do Appreciate its difficult to read – see Handout The Dashboard is useful as it… As primary care physicians we know our own communities well and live daily with the tension between providing continuity of care and meeting the accessibility they need, whilst working in practices stretched by workforce challenges and rising demand. It seems essential therefore that for GP at Scale to develop in any area, organisations will need good data on the health needs of their local population upon which to base any new care models, as the Nuffield Trust projects are demonstrating – including in the Valentine medical group. This will mean that working at scale can improve the care patients receive without increasing the burden on primary care professionals Allows the auditing process to happen, and provides your PM / GP Lead insight on Workflow Administrators training needs. Track implementation of workflow for your practice, including percentage of letters being completed by a clinician vs. administrator Help measure the impact of Workflow across the practice including the workload of clinicians and administrators Support you to identify which letter types to tackle next Provide clear data on the types, shapes and volume of demand of clinical correspondence, allowing engagement with your hospitals and providers to influence change in the future Will pick out a few graphs to introduce you to……
- I’m showing this so you get a sense of just how much information the Dashboard can give you and what it allows you to do Appreciate its difficult to read – see Handout The Dashboard is useful as it… As primary care physicians we know our own communities well and live daily with the tension between providing continuity of care and meeting the accessibility they need, whilst working in practices stretched by workforce challenges and rising demand. It seems essential therefore that for GP at Scale to develop in any area, organisations will need good data on the health needs of their local population upon which to base any new care models, as the Nuffield Trust projects are demonstrating – including in the Valentine medical group. This will mean that working at scale can improve the care patients receive without increasing the burden on primary care professionals Allows the auditing process to happen, and provides your PM / GP Lead insight on Workflow Administrators training needs. Track implementation of workflow for your practice, including percentage of letters being completed by a clinician vs. administrator Help measure the impact of Workflow across the practice including the workload of clinicians and administrators Support you to identify which letter types to tackle next Provide clear data on the types, shapes and volume of demand of clinical correspondence, allowing engagement with your hospitals and providers to influence change in the future Will pick out a few graphs to introduce you to……
- How to use working at scale as a way to improve quality? • What are the key challenges that you face when working at scale? How do different new different models of care compare? • How do we release clinical leadership time? • How can we build trust and relationships in primary care? • How can working at scale address workforce issues?