Global issues 12.5.13
- 3. PQRS. Physical therapists, will be able to avoid the 2016 2.0% PQRS penalty by reporting at least 3 individual measures via claims or registry for 50% or more of eligible Medicare patients in the 2014 reporting period. increase the number of PQRS quality measures that providers must report either via claims or registry from 3 to 9 to qualify for the 0.5% bonus payment in 2014 eliminate the option to report on measures groups via claims. New measures
- 5. To identify, develop, endorse, implement, and advance quality measures in PT and the settings where PTs practice. To advance payment models that promote the value of PT. To identify, develop and implement public policy and payment initiatives that advance the role of the PT in disease management, prevention and wellness.
- 6. To improve access to PTs by the elimination of regulatory, legal and payment policy barriers. To eliminate referral for profit in PT To advance policy that ensure a qualified workforce in PT to meet the public need for health care services. Increase funding for rehabilitation research
- 8. Extended Scope of Practice Direct Access Quality Initiatives Inter-professional Collaboration Research
- 9. Full PT Scope of Practice Extended Scope/New Areas State Practice Act/Institutional policy Individual Scope –personal competence
- 10. Advanced Scope of Practice: A role that is within the currently recognized scope of practice for that profession, but that through custom and practice has been performed by other professions. The advanced role may require additional training as well as significant professional experience and competency development. ▪ Australian Physiotherapy Association Example
- 11. Extended Scope of Practice-:A role that is outside the currently recognized scope of practice and one that requires some method of credentialing following additional training, competency development and significant professional experience, as well as legislative change. Australian Physiotherapy Association Example
- 13. Objective The summit sought to share international experiences in developing and implementing policy direct access and advanced practice in physical therapy. A post Summit working group addressed key questions involving direct access and advanced scope of practice and strategies to move this international priority.
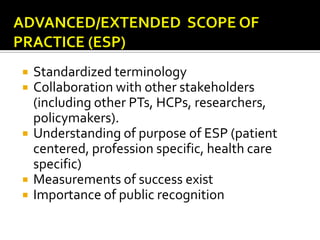
- 14. Standardized terminology Collaboration with other stakeholders (including other PTs, HCPs, researchers, policymakers). Understanding of purpose of ESP (patient centered, profession specific, health care specific) Measurements of success exist Importance of public recognition
- 15. Prescribing Rights for Physical Therapists
- 16. Rising health care costs, problems with access to care, and physician shortages leading to new models of care. Physiotherapy as key provider for services for MSK disorders Natural to move to advanced/extended SOP.
- 17. United Kingdom: 2005 : supplementary prescribers. ▪ “Voluntary partnership with medical practitioner and eligible supplementary prescriber to implement an agreed patient specific written clinical management plan with the patients agreement” ▪ Need counter signature August 2013: Independent prescribing by physiotherapists. ▪ “..independent prescribing is prescribing by a practitioner responsible and accountable for the assessment of patients with undiagnosed or diagnosed conditions and for decisions about the clinical management required, including prescribing.” * ▪ Eligible: Advanced practitioners and additional training ▪ Wide range of medicines *Department of Health (2006) Improving Patients’ Access to Medicines – A Guide to Implementing Nurse and Pharmacist Independent Prescribing within the NHS in England, London, DH
- 18. Australia Non Medical Prescribing Pathway. Identified large increases in demand for health care, equity of access, financial sustainability, workforce shortages and a fragmented health system as challenges facing Australia. PTs considered as primary contact practitioners. Recently approved by the Minster of Health
- 19. Desmeules, et al (2012) Systematic Review: Assess effectiveness of PT’s in APP Roles “The new roles include role enhancement and role substitution related to traditionally performed medical or controlled acts, such as: communicating a diagnosis, triaging potential surgical candidates, ordering diagnostic imaging or laboratory tests, and prescribing/injecting medication.” Conclusion: ▪ “emerging evidence suggests that physiotherapists in APP roles provide equal or better usual care in comparison to physicians in terms of diagnostic accuracy, treatment effectiveness, use of healthcare resources, economic costs and patient satisfaction. There is a need for more methodologically sound studies to evaluate the effectiveness APP care.” Desmeules F, Roy JS, MacDermid JC, Champagne F, Hinse O, Woodhouse LJ. Advanced practice physiotherapy in patients with musculoskeletal disorders: A systematic review. BMC Musculoskelet Disord. 2012;13:107-2474-13107. doi: 10.1186/1471-2474-13-107; 10.1186/1471-2474-13-107.
- 20. Is prescribing medication a direction we should (want) to take in the United States?
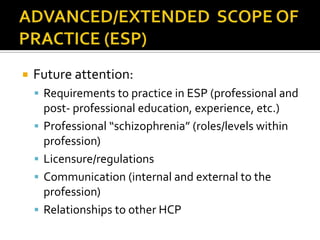
- 21. Future attention: Requirements to practice in ESP (professional and post- professional education, experience, etc.) Professional “schizophrenia” (roles/levels within profession) Licensure/regulations Communication (internal and external to the profession) Relationships to other HCP
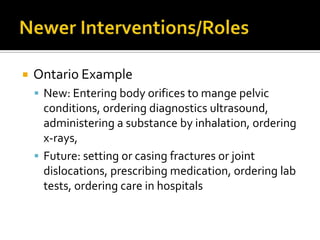
- 22. Ontario Example New: Entering body orifices to mange pelvic conditions, ordering diagnostics ultrasound, administering a substance by inhalation, ordering x-rays, Future: setting or casing fractures or joint dislocations, prescribing medication, ordering lab tests, ordering care in hospitals
- 23. One person’s advanced is another’s entry to practice Is it time to define PT around the world? What makes us US?
- 25. Data exists supporting direct access or patient self referral (cost, safety) Communicate and Consult
- 26. Purpose of direct access should be in terms of societal mission and be person centered.
- 27. Future attention: Need for standardized terminology (patient self referral vs. direct access) Global communciation of advances in DA Global consideration need to be adapted to regional and local jurisdictions. Setting specific variations in DA(public vs. private, variations in practice settings) Research requirements
- 28. Department of Practice driven survey with 1800 members from 9 selected chapters with varying degrees of direct access. Results: Although slightly more than half of the respondents report seeing patients without referral, the percentage of direct access patients in practice settings in these chapters is small. Physical therapists in private practice settings are much more likely to see patients via direct access than those in other settings. Employer requirements that all patients have a referral appear to impose a significant barrier to direct access. This requirement exists in all types of practice settings but is especially prevalent in both inpatient and outpatient hospital-based settings. A large percentage of respondents indicated a need for resources to help them remove hospital/institutional restrictions to direct access.
- 30. Importance of Value based research: Comparative effectiveness Efficiency and effectives of care Measures of quality
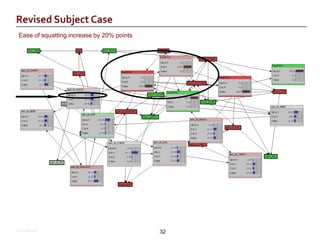
- 31. Boxes with black surrounds indicate actual case data inputs – other boxes are derived estimates Confidential 31
- 32. Ease of squatting increase by 20% points Confidential 32
- 33. The role of the PT in global healthcare challenges. International “standardization” for PT education, practice, and policy (regulation). EBP relation to policy development. PT role in health care policy development
- 35. Opportunities for advancement and innovation dependent upon unique environments that are influenced by national social and health care system, health care worker availability, and local facilities. Need to convince internal and external stakeholders of the role, value and effectiveness of physical therapy Collaborative and interprofessional models tended to be highly successful. Access to care was an important factor in all countries Practitioner malaise: resistance to change practice behaviors Data extremely important; so to are patient ‘stories’
- 36. Physicians working Map, accessed November 5, 2012 from World Mapper website: http://www.sasi.group.shef.ac.uk/worldmapper/textindex/text_health.html
- 37. HIV prevalence Map, accessed November 5, 2012 from World Mapper website: http://www.sasi.group.shef.ac.uk/worldmapper/display.php?selected=227
- 38. Diabetes prevalence: accessed November 5, 2012 from World Mapper website: http://www..sasi.group.shef.ac.uk/worldmapper/images/largepng/239.png
- 39. Addressing a need Singapore: PTs in ICU and critical care areas do not require physician referral for PT ▪ SARS outbreak was driver Political Push: Chartered Society regarding extended scope practitioner and prescription rights.
- 40. Improving access “New service models including self-referral to allied health professional services such as musculoskeletal physiotherapy, have improved patient outcomes and satisfaction and reduced demand elsewhere in the system. “
- 41. Various educational standards within member countries. Freedom of movement legislation: If there is a shortfall in the entry level education and attestations of competency of an applicant from another member state: ▪ A compensatory measure must be offered. ▪ Have we defined explicitly the educational requirements for direct access (first contact practitioners)?
- 43. PASS took place February 27-28, 2009, The PASS was designed as an invigorating experience and created a highly interactive environment that allowed rich, insightful discussion in five topic areas: education - professional preparation, health care access, systems and funding, practice models, research, technology.
- 44. Paradigm Shift to physical therapists as an integral part of a collaborative, multidisciplinary health care team that has the health care consumer as its focus. Technology: Information technology, integrated data systems, robotics, prosthetics tissue engineering, Imaging Value of PT to stakeholders (consumers) Prevention and Wellness Innovative practice models needed
- 45. Innovation
- 46. Providing secondary prevention services in a disease management model Improving physical therapy outcomes by incorporating evidence into practice in an integrated health care setting Providing consulting services in a primary prevention model Providing care in a hospital emergency department Providing outpatient services in a setting that incorporates evidence in practice to decrease costs and improve outcomes
- 47. Providing care to large numbers of patients in an HMO model Providing health promotion services to groups Providing services in an urban, academic medical center emergency department Providing direct access services in an academic medical center out-patient clinic Providing services to individuals in a military outpatient setting
- 48. Emergency Departments / Urgent Care Surgery Triage for musculoskeletal patients Public health role Technology
- 49. What needs changing? How will you lead your profession?
Editor's Notes
- Change behaviors