Male reproductive organs
- 1. Review of Male Reproductive Organ By- Isha Thapa Magar Master in Nursing (WHD) TU, IOM
- 2. Male Reproductive System • External Male Reproductive system • Internal male reproductive organs
- 3. Male Reproductive Organs External Male Reproductive Organs 1. Scrotum 2. Penis Internal male reproductive organs 1. Testis 2. Epididymis 3. Vas Deferens 4. Accessory Glands a. Seminal Vesicles b. Prostate Gland c. Bulbourethral Glands
- 4. Scrotum • A pouch of skin formed from lower part of abdominal wall. • Scrotum forms a pouch in which testes are suspended outside body. • Scrotum keeps testes at a temperature slightly cooler than body temperature.
- 5. Penis • Penis is male external genital organ for passage of urine and semen to exterior. • It is about 10 cm long, 4 cm breath flaccid muscular cylindrical organs. • Composed mainly of three cylindrical columns of erectile tissue.
- 6. Testis
- 7. Testis • Testis are oval-shaped male reproductive organs located in scrotum, just behind penis. • Testis are 4.5 cm in length, 2.5 cm breath, 3 cm in thicken and weight about 10-14 gm. • In embryo, testis develop within upper abdominal cavity and during 7th month of fetal life they migrate into scrotum.
- 8. • Each testis consists of 200 to 300 lobules. • Each testis is made of tightly coiled structures called seminiferous tubules.
- 9. • Testes contain 3 types of cells: 1. Germ cells 2. Sertoli cells, and 3. Leydig (interstitial) cells
- 11. • Germ cells undergoing progressive differentiation and development into mature spermatozoa. • Sertoli cells are supporting cells • Ledyig (interstitial) cells are testosterone producing cells
- 12. Epididymis • Epididymis is a tightly coiled tubes against testicles. • Is comma shaped structure which consists of head, body and tail, that is continuous with vas deferens. • It acts as maturation and storage place for sperm.
- 14. Vas deferens • Vas deferens is a thin tube and continuation of epididymis to urethra in penis. • They transport sperm from the epididymis in anticipation of ejaculation.
- 16. Accessory glands • Accessory glands are – Seminal Vesicles – Prostate Gland – Bulbourethral gland • These glands produce nourishing fluids for sperms that enter urethra.
- 17. Seminal Vesicles • Seminal Vesicles are sac-like structures attached to vas deferens at one side of bladder. • They produce a sticky yellowish fluid that contains fructose.
- 19. Prostate Gland • Prostate Gland surrounds ejaculatory ducts at base of urethra, just below the bladder. • Is responsible for making production of semen, a liquid mixture of sperm cells, prostate fluid and seminal fluid.
- 21. Bulbourethral Glands - Bulbourethral Glands are two small glands located on sides of urethra just below prostate gland. - These glands produce a clear, slippery fluid that empties directly into urethra.
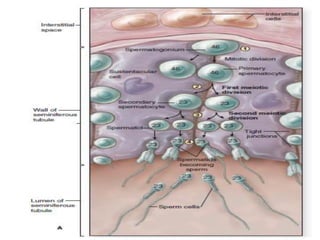
- 23. Spermatogenesis Introduction • Spermatogenesis is the process by which primitive male gametes become mature sperm. • Spermatogenesis takes place in the seminiferous tubules under influence of Follicle stimulating hormone (FHS) and testosterone.
- 24. • Pituitary gland secretes luteinizing hormone (LH), which stimulates synthesis and secretion of testosterone by Leydig cells, and follicle- stimulating hormone (FSH), which acts with testosterone on Sertoli cells to stimulate spermatogenesis
- 25. • Germinal epithelial cells lining seminiferous tubules are called spermatogonia. • They are present at birth but do not produce spermatozoa until puberty. • At puberty, spermatozoa begin to actively divide under influence (FSH) and continues throughout adult life. • Spermatogonia enter maturation process every 16 days, and development from spermatogonia stem cells to mature sperm cells takes about 75 days.
- 27. Process of Spermatogenesis 1. Shortly before puberty, primordial gremial cells develop into spermatogonia and remains in wall of seminiferous tubules. 2. Mitosis cell division occurs resulting differentiation of Spermatogonia into primary spermatocytes. 3. Each primary spermatocytes contains 22 pairs of autosomes and one pair of sex chromosomes.
- 28. 3. Through First meiotic division, secondary spermatocytes are formed having haploid number of chromosomes either 23,X or 23, Y from primary oocytes. 4. Immediately follows, second meiotic division with formation of four spermatids, each containing haploid number of chromosomes, two with 23, X and two with 23, Y.
- 29. • After formation of spermatids , extensive morphological differentiation of spermatids occurs without further cell division to convert them into spermatozoa/sperm. This process is called Spermiogenesis.
- 33. Sperm
- 34. Introduction • Spermatozoon is a motile cell gamete and shaped liked a tadpole. • Structure: 1. Head: head region of sperm that contains DNA. 2. Mid piece: narrow middle part of cell contains mitochondria. 3. Tail: wavelike motion of flagellum propels sperm forward.
- 36. Contd.. • At each ejaculation, 2-4ml of semen is released. • Seminal fluid contains about 100 million sperm per milliliter, of which 20-25% are likely to be abnormal. • Survival time of spermatozoa is approximately 72 hours. • Only one spermatozoon is necessary to fertilize ovum.
- 37. Sperm Transport • During ejaculation, mature spermatozoa are released from vas deferens along with fluid from prostate, seminal vesicles, and bulbourethral glands. • Following ejaculation, released spermatozoa must undergo capacitation to become competent to fertilize oocyte. • Capacitation occurs within cervical mucus and involves removal of inhibitory mediators such as cholesterol from sperm surface, tyrosine phosphorylation, and calcium ion influx.
- 38. • When sperm reach tubal isthmus they are slowly released into ampulla, further reducing number of sperm that reach oocyte. • Sperm transport from posterior vaginal fornix to fallopian tubes occurs within 2 minutes during follicular phase of menstrual cycle
- 39. Fertilization • As capacitated sperm near and pass through cumulus cells surrounding oocyte, hydrolytic enzymes are released from acrosome via exocytosis in a process called acrosome reaction. • Following acrosome reaction, sperm binds to and penetrates zona pellucida. • Resulting sperm to fuse with plasma membrane of oocyte, an event that promotes changes in oocyte and prevent entry by additional sperm.
- 40. • As first sperm penetrates zona pellucida, cortical granules are released ( cortical reaction) from oocyte. • This stops oocyte’s zona pellucida from binding new sperm and inhibits penetration by previously bound sperm, further reducing possibility of polyspermy.