Metabolism 1
- 1. So far, 74 CYP gene families have been described, of which three main ones (CYP1, CYP2, CYP3) are involved in drug metabolism in human liver. CYP1A2 is one of the main enzyme. (Cytochrome P450 is called ‘super family’)
- 2. Drug oxidation by the monooxygenase P450 system requires drug , P450 enzymes, and in addition molecular O2 , NADPH and a flavoprotein (NADPH-P450 reductase)
- 3. Examples of common drugs that are substrate for P450 isoenzymes Isoenzyme P450 Drug CYP1A1 Theophyline CYP1A2 Caffeine, paracetamol CYP2A6 Methoxyflurane CYP2 Taxol CYP2C9 Ibuprofen, phenytoin, tolbutamide, warfarin
- 4. Cont’d……. CYP2C19 Omeprazole CYP2D6 Clozepine, codeine CYP2E1 Alcohol, halothane CYP3A4/ Losartan, nifedipine, terfenadine
- 5. P450 and biological variation Within the human populations there are major sources of interindividual variation in P450 enzymes that are of great importance in therapeutics. These include genetic polymorphisms: For example, one variant of the gene CYP2D6 leads to poor or extensive hydroxylation of debrisoquine, (an antihypertensive drug).
- 6. Cont’d….. Environmental factors: enzymes inducers and inhibitors are present in the diet and environment. For example, grapefruit and St John’s wort inhibit drug metabolism: cardiac dysrythmias. Cigarette smoke induce P450 enzymes
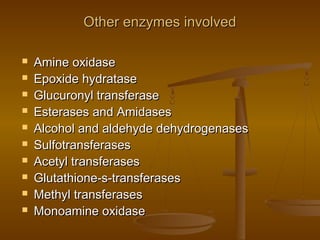
- 7. Other enzymes involved Amine oxidase Epoxide hydratase Glucuronyl transferase Esterases and Amidases Alcohol and aldehyde dehydrogenases Sulfotransferases Acetyl transferases Glutathione-s-transferases Methyl transferases Monoamine oxidase
- 8. Induction of microsomal enzyme activity Many drugs and chemicals 1. Anticonvulsants including phenobarbitone, rifampicin, glucocorticoids induce CYP3A isoenzymes 2. Phenobarbitone also induce CYP2B1 and rifampicin also induce CYP2D6 3. Isoniazid and chronic alcohol consumption induce CYP2E1
- 9. 4. Benzopyrine found in cigarette smoke and industrial pollutants induce CYP1A isoenzymes 5. Others: DDT(dichloro diphenyl trichloroethane), phenylbutazone, griseofulvin etc.
- 10. Inhibition of the microsomal enzyme activity Allopurinol Amiodarone Chloramphenicol Cimetidine Ciprofloxacine Diltiazem Metronidazole Ketokonazole Omeprazole MAO inhibitors Quinidine Sulfonamides
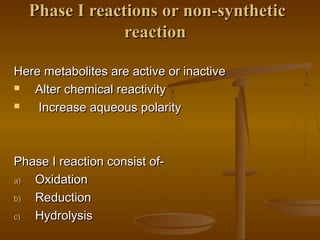
- 11. Phase I reactions or non-synthetic reaction Here metabolites are active or inactive Alter chemical reactivity Increase aqueous polarity Phase I reaction consist of- a) Oxidation b) Reduction c) Hydrolysis
- 12. In the phase I reaction, it may result in inactivation, change in the activity or inactivation of the parent drugs. In this phase, introducing the drug molecule to polar group such as -OH, -COOH, -NH2, and –SH. a) Oxidation This reaction involves addition of oxygen/negatively charged radical or removal of hydrogen /positively charged radical Two types- 1. Microsomal oxidation 2. Non- microsomal oxidation
- 13. a) Oxidation This reaction involves addition of oxygen/negatively charged radical or removal of hydrogen /positively charged radical Two types- 1. Microsomal oxidation 2. Non- microsomal oxidation
- 14. Microsomal oxidation 1. Aromatic hydroxylation 2. Aliphatic hydroxylation 3. N-, O-, or S-dealkylation 4. Epoxidation 5. Desulfuration 6. Deamination 7. Sulfoxidation 8. N—oxidation 9. N- hydroxylation 10. Dehalogenation
- 15. 1. Aromatic hydroxylation- Acitanilide ----------- p-hydroxyacetanilide (paracetamol or acetaminophen) 2. Aliphatic hydroxylation Phenobarbitone --------- phenobarbitone alcohol 3. Dealkylation: N-dealkylation- ex- diazepam -------desmethyldiazepam, here N- methyl group can be removed oxidatively
- 16. 4. O-deakylation- ex- phenacetin ----- paracetamol ( active metabolites) 5. Epoxidation- ex- Vitamin k -------- vitamin k epoxide benzene -------- benzene epoxide 6. Desulfuration- ex- Melathion -------Parathion ( more toxic than parent drug) 7. Deamination- ex- Amphetamine ------- phenylacetone ( inactive )
- 17. b) Reduction Drugs those contain- disulphide (s:s), azo (n:n), or nitro (no2) Azo- ex- Prontosil dye ---------- > Sulfanilamide Nitro- ex- chloramphenicol --------- > arylamine
- 18. c) Hydrolysis Ex- Acetylcholine -------- choline + acetate Procaine ------------- > p-aminobenzoic acid
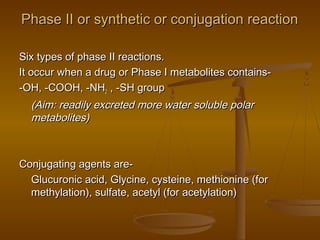
- 19. Phase II or synthetic or conjugation reaction Six types of phase II reactions. It occur when a drug or Phase I metabolites contains- -OH, -COOH, -NH2 , -SH group (Aim: readily excreted more water soluble polar metabolites) Conjugating agents are- Glucuronic acid, Glycine, cysteine, methionine (for methylation), sulfate, acetyl (for acetylation)
- 20. Species variation in conjugation reaction can depend on occurrence of the conjugating agent, ability of the body to form the necessary nucleotide or amount of transferring enzymes. Certain conjugation reaction are either defective or absent in particular species.
- 21. Cont’d….. Ex.- The cat synthesizes glucuronide conjugation at a slower rate, as this species is deficient in the transferring enzyme glucuronyl transferase The dog and fox are unable to acetylate aromatic amino groups
- 22. Glucuronide conjugation Drugs and some endogenous substances, steroid, thyroxine, bilirubin. First of all, glucuronic acid should be activated. The activated form of glucuronic acid is the nucleotide- uridinine diphosphate glucuronic acid (UDPGA) The drugs and endogenous substances that are excreted largely as glucuronides include-
- 23. The drugs and endogenous substances that are excreted largely as glucuronides include- Drugs: Morphine Salicylates Acetaminophen Chloramphenicol Phase I metabolites of diazepam (oxazepam), phenylbutazone (oxyphebylbutazone)
- 25. Requirement for the formation of glucuronide- UDPGA, drug or its metabolites and glucuronyl transferase Why more water soluble? Because, large hydrophilic carbohydrate moiety and more highly ionized at physiological pH values