Nephrotic syndrome
- 1. APPROACH TO NEPHROTIC SYNDROME IN ADULTS
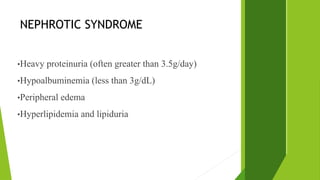
- 2. NEPHROTIC SYNDROME •Heavy proteinuria (often greater than 3.5g/day) •Hypoalbuminemia (less than 3g/dL) •Peripheral edema •Hyperlipidemia and lipiduria
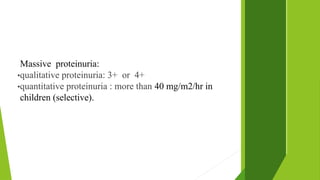
- 3. Massive proteinuria: •qualitative proteinuria: 3+ or 4+ •quantitative proteinuria : more than 40 mg/m2/hr in children (selective).
- 4. Causes of Nephrotic syndrome Primary causes 1.Membranous glomerulopathy (30% in adults) 2.Focal segmental glomerulosclerosis (15% in adult) 3.Minimal change disease (10-15% in adults and 70-90% in children)
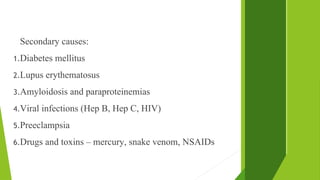
- 5. Secondary causes: 1.Diabetes mellitus 2.Lupus erythematosus 3.Amyloidosis and paraproteinemias 4.Viral infections (Hep B, Hep C, HIV) 5.Preeclampsia 6.Drugs and toxins – mercury, snake venom, NSAIDs
- 6. NEPHROTIC SYNDROME 1. MINIMAL CHANGE DISEASE •nil lesion •70-90% of nephrotic syndrome in childhood •10-15% of nephrotic syndrome in adults •On renal biopsy- No obvious glomerular lesion by light microscopy •Immunofluorescence - no evidence of immune complex deposition •diffuse effacement of epithelial cell foot processes on
- 7. •Selective proteinuria: principally contains albumin with minimal amounts of higher-molecular-weight proteins •30% children have spontaneous remission •All children treated with steroids •Non-responders are biopsied
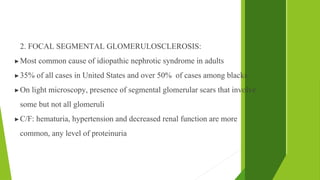
- 8. 2. FOCAL SEGMENTAL GLOMERULOSCLEROSIS: ▶Most common cause of idiopathic nephrotic syndrome in adults ▶35% of all cases in United States and over 50% of cases among blacks ▶On light microscopy, presence of segmental glomerular scars that involve some but not all glomeruli ▶C/F: hematuria, hypertension and decreased renal function are more common, any level of proteinuria
- 9. 3. MEMBRANOUS NEPHROPATHY: ▶Most common cause of primary nephrotic syndrome in adults ▶Most often secondary disorder in children ▶Uniform thickening of basement membrane along the peripheral capillary loops in light microscopy ▶Diffuse granular deposits of IgG and C3 ▶Electron dense sub-epithelial deposits ▶Autoantibodies against Phopholipase A2 Receptors (PLA2R) may be present in most adults in idiopathic nephropathies
- 10. Work-up •CBC •Serum albumin •Renal function test •Urinalysis and urine sediment examination •Urine protein measurement (24-hr)
- 11. Work-up •Lipid profile •Serologic studies for infection and immune abnormalities •Renal ultrasonography •Renal biopsy
- 12. Indications of renal biopsy in nephrotic syndrome •Features s/o diagnosis other than MCD •NS presenting in 1st year of life •NS presenting after 6 years •Failure to respond to adequate dose of steroid therapy in 28 days •Relapsing Nephrotic Syndrome •Development of steroid resistance •Change in clinical course •Patient with renal insufficiency and nephrotic syndrome •Before starting immunosuppressive therapy
- 14. COMPLICATIONS IN NEPHROTIC SYNDROME •Thromboembolism •Acute Renal Failure •Hypovolemic crisis •Infections •Cardiovascular complication •Anemia
- 15. THROMBOEMBOLISM •Nephrotic syndrome is associated with increased risk of thromboembolic complications •Incidence of arterial and venous thrombosis(10-40%) •Risk is particularly increased with lower serum albumin levels Ref: Barbano B, Gigante A, Amoroso A, Cianci R. Thrombosis in nephrotic syndrome. Semin Thromb Hemost. 2013;39(5):469–76.
- 16. Why patients are at increased risk? •Loss of antithrombotic factors in the urine •Increase in plasma procoagulant cofactors, as factor V, factor VIII, and fibrinogen •Lack of balance between procoagulant/anticoagulant factors •Abnormalities in platelet activation that promote in situ thrombosis
- 17. •Fibrinogen, factor V, and factor VIII synthesis are increased out of proportion to urinary losses •Increased von Willebrand factor levels are associated with increased platelet adhesion
- 21. Clinical Predictors of Thrombotic Risk 1. Histologic diagnosis of NS is of paramount importance in assessing the risk of thrombosis- Prevelance high in Membranous Nephropathy (10-40%) 2. Low albumin level •<2.8g/L in MN •<2g/L in other nephrotic syndrome 3. Age- Adults have 7 to 8 fold increased risk of thombotic events
- 22. Renal vein thrombosis RVT has been reported in approximately 25 to 30% of nephrotic patients ↖membranous glomerulonephritis (37%), ↖membranoproliferative glomerulonephritis (26%), ↖minimal-change disease (24%)
- 23. DVT in Nephrotic Syndrome •Most common thrombotic complication •Risk stratification to be done by Wells score • Wells score ≥1, Doppler ultrasound of lower extremities must be performed to exclude DVT •Confirmed DVT, anticoagulation therapy is warranted •IVC filters in contraindicated patients
- 24. Pulmonary Thromboembolism •DVT is major risk factor for PTE •The origin of pulmonary embolus from renal vein has also been reported •Management of PTE depends on cardiovascular instability and presence of right ventricular disfunction
- 25. Prophylaxis against Increased Thrombotic Risk in Patients with NS •Because of lack of randomised clinical trials optimal approach to prophylactic anticoagulation is not well defined •Decision is based on serum albumin level and bleeding risk with anticoagulation
- 26. Prophylactic anticoagulation 1.Incidence of thrombotic events 2.Bleeding risk Choice of anticoagulants: ▶Aspirin ▶Heparin ▶Warfarin ▶Not recommended in asymptomatic RVT
- 27. Prophylaxis is given in membranous nephropathy – ▶Low bleeding risk and albumin <3 ▶Intermediate bleeding risk and Sr.albumin <2g/dl •Regardless of the cause of nephrotic syndrome if patient has potential indications for anticoagulation and low bleeding risk prophylaxis is given •Ref: Primary Nephrotic Syndrome in Adults as risk factor for pulmonary embolism (Aibek Et al)
- 28. Treatment of hypercoagulability in NS •Anticoagulation to prevent thromboembolic events •Anticoagulation for dissolution or removal of thrombus
- 29. Symptomatic RVT, DVT and PTE ↖Treatment consists of anticoagulation, initially with heparin and then with warfarin Nephrotic patients resistant to heparin ↖Direct thrombin inhibitors ↖Ref: Glassock RJ, Prophylactic anticoagulation in nephrotic syndromes: a clinical corrundrum (2007)
- 30. Platelet abnormalities in nephrotic syndrome •Increased platelet counts and platelet hyperactivity have been observed in nephrotic patients •Walter et al reported for the first time a statistically significant increase in mean platelet count in adult patients with nephrotic syndrome •There is controversy concerning the need of prophylactic treatment in the prevention of thromboembolic events in Nephrotic syndrome •REF: Benedicte et al .Platelet abnormalities in Nephrotic Syndrome
- 31. Pathogenesis of quantitative platelet changes in NS •Hypoalbuminemia is suggested to play a role in increased platelet counts •Hypercholesterolemia •Urinary loss of PACAP (Pituitary Adenylate Cyclase Activating Polypeptide), inhibitor of megakaryopoiesis
- 32. Infection •Children are mainly susceptible to infection •Infections in patients with NS have been described as a hallmark of idiopathic nephrotic syndrome •Most common infections – URTI, Peritonitis, UTI •Increased risk of developing serious bacterial infections especially with encapsulated bacteria
- 33. Factors contributing for infections •Reduced serum concentrations of immunoglobulin G •Decreased levels of the alternative complement pathway factors B and D •Impaired ability to make specific antibodies REF: Emilia et al, Influence of Nephrotic state on the infectious profile in childhood idiopathic nephrotic syndrome (2004)
- 34. Acute kidney injury •Acute onset nephrotic syndrome does not typically present with AKI •In Minimal Change Disease and FSGS, AKI may be present at the time of presentation •In 25-30% of adults with MCD, AKI had been reported
- 35. •AKI in adults with MCD ▶Acute tubular necrosis ▶Use of NSAIDs ▶Excessive diuresis ▶Contrast induced nephropathy ▶Severe renal interstitial edema ▶Increased urinary viscosity
- 36. •AKI in other forms of Nephrotic Syndrome ▶Due to glomerular and concurrent tubular injury ▶RVT ▶Drugs Ref: Waldman et al, Adult – minimal change disease (2007)
- 37. Anemia in nephrotic syndrome •Increased urinary losses of iron and transferrin •Urinary losses of erythropoietin •Losses of transcobalamin and vitamin B12 in the urine •The role of metals and drugs -Urinary losses of ceruloplasmin, can lead to copper deficiency and consequent anemia in patients with nephrotic syndrome. Ref: Franca Iorember, Diego Aviles, Anemia in Nephrotic Syndrome: approach to evaluation and treatment
- 38. Protein malnutrition •Marked proteinuria •Loss in lean body mass with negative nitrogen balance •Anorexia and vomiting secondary to edema of the GI tract
- 39. Cardiovascular complications •As a result of dyslipidemia, cardiovascular complications may occur
- 40. Hypovolemia •Symptomatic hypovolemia may occur •As a result of over diuresis in those with serum albumin level of less than 1.5g/dl •Volume depletion due to severe hypoalbuminemia causing fluid movement into interstitium