NYU Langone Medical Center’s TJA BPCI Experience: Lessons in How to Maximize Value
- 1. NYULMC Hospital for Joint Diseases NYU Langone Medical Center’s TJA BPCI Experience: Lessons in How to Maximize Value Richard Iorio, MD Chief of Adult Reconstruction William and Susan Jaffe Professor of Orthopaedic Surgery Department of Orthopaedic Surgery NYU Langone Medical Center Hospital for Joint Diseases
- 2. Disclosures • Consultant for Medtronic and DJO Surgical • Product liability consultant for DePuy Orthopaedics • Co-founder Labrador Healthcare Consulting Services • Co-founder LIMA Project • Co-founder Responsive Risk Solutions • Advisory Board Member Pacira, Wellbe, Inc, ActiveCare MCS, Muvehealth • AAHKS, Knee Society and Hip Society Member • Consultant reviewer for JBJS, CORR, JOA, JAAOS • Editorial Board JBJS Reviews, Adult Reconstruction Section Editor • Institutional Research Support: Pacira, Orthofix, Vericel, Orthosensor, Bioventus, Ferring 2
- 3. The Future is Here Value Based Purchasing (VBP) •The goal of value based purchasing (VBP) is to transform Medicare from a passive payer of claims to an active purchaser of care. •In the past health care organizations were profitable as long as they processed patients. •For decades, health care systems have responded to incentives that rewarded volume regardless of quality. •VBP is an effort to change the focus of how care is paid for: in essence, the government wants value – not just quantity – for the money that it spends. •Episode of care delivery such as bundled payment offers a framework to measure the amount of value brought to a diagnosis 3
- 4. Bundled Payment Initiative Background •NYULMC HJD is a large, tertiary, academic medical center with a hybrid compensation system which implemented a Model 2 bundled payment initiative for Total Joint Replacement, Spinal Fusion and Cardiac Valve Surgery in January of 2013. •In April of 2016, CJR, a modification of Model 2 BPCI, was instituted in 67 MSA’s by CMS •In January of 2017, quality and financial metrics will begin collection for MIPS under MACRA which will regulate CMS reimbursement for the foreseeable future as a replacement for SGR adjustments •In January of 2018, voluntary participation in BPCI and CJR will be reopened to allow for advanced APM fulfillment of the requirements of MIPS and MACRA 4
- 5. The Future is Here Differences between BPCI and CJR •All episodes will be 90 days of care (Model 2 BPCI) •No third party purveyors or EI, hospitals only •Historical and Regional data is used to set target price in years 1-3 •Regional data only will be used for year 4 and 5 in CJR •Quality metric reporting and PRO measurement will be rewarded •Hospital Quality Standards will be used to determine eligibility for reconciliation: RSCR, HCAHPS, and PROMs •Reconciliation will be awarded with a composite score methodology of quality measures and financial performance •No physician risk throughout the program, No hospital risk in year 1 •Stop loss limits, 5% above target in year 2, 10% in 3, and 20% in years 4-5 •Gains limited to 20% above target price x number of episodes •Risk stratified episode threshold for hip fractures •Relief for difficult diagnoses like HCV, HIV and Hemophilia 5
- 6. CJR It’s good to be bad…until it’s not • CMS recognizes that hospitals may have limited ability to moderate spending for certain high cost cases. Therefore in setting target prices for both MS-DRGs, CMS proposes to set a high outlier limit at two standard deviations above the regional average episode cost. Individual episode costs that exceed the high outlier limit would be truncated to that limit so hospitals’ downside risk would be limited. • CMS does not propose to set target prices based solely on historical hospital- specific data but rather intends to use a blend of historical hospital-specific and regional-historical claim data. CMS proposes to transition to using regional only data to set targets by PY 4. CMS asserts this approach will afford early and continuing incentives for both efficient and less efficient hospitals to furnish high quality, efficient care in all years of the model. • CMS recognizes the need for more physician involvement and will rectify this in January 2018 with the ability of physicians to take more risk in both models 6
- 7. The Future is Here There will be winners and losers within the CJR demonstration project 7 Years 1 and 2 Year 3 Years 4 and 5 100% Regional2/3 Regional 1/3 Hospital 1/3 Regional 2/3 Hospital Target price based on hospital (historical) and regional pricing
- 8. Bundled Payment Initiative Background of BPCI •The episode of care included the inpatient and post-acute care and all costs through 90 days following discharge. The patient does not receive financial incentives. CMS requires quality measure reporting. A provider’s participation may be terminated by CMS if quality decreases or if CMS identifies a significant concern. •All unilateral, primary TKA and THA were included. Revisions and bilateral TJA were excluded. DRG’s 469 and 470 were included and payment was increased for DRG 469 due to the increased comorbidities. The reference years for cost comparison were 2009-12. •Clinical care coordination among all providers, evidence based clinical pathway implementation, and standardization of post discharge care were critical to the success of the program. 8
- 9. What is Included in the Target Price? Home Health Agencies Outpatient Therapy Services Skilled Nursing Facilities & LTACH Inpatient Rehab Hospital Surgeon Physician Visits (surgeon and other) Any services during the 90-Day Post-Acute Period such as… Consulting Physicians Readmissions (to NYU or others) DME 9 Part B Drugs Outpatient Services Lab Services Anesthesiologist Any services during the Acute Stay such as… Any services 72 hours prior to Admission such as… ED Visits Physician Visits (surgeon and other) PAT Days 91-120 CMS will be monitoring the period immediately following to ensure that services are not being shifted outside the bundle. NYULMC will be financially responsible if such behavior is observed and may be removed from the program.
- 10. Avg Medicare Payment1 DRG DRG Description Inpatient Only2 90D Bundle3 469 MAJOR JOINT REPLACEMENT W MCC $16,303 $54,233 470 MAJOR JOINT REPLACEMENT W/O MCC $12,446 $35,565 1Data is based on FY 2009-12 Medicare claims. CMS will be carrying rates forward to 2013 for the Episodes of Care Initiative. 2Inpatient payment includes patient deductible/coinsurance amounts, and excludes IME, DSH, Capital, and GDME payments. 390D Bundle includes Medicare readmissions exclusions and Part B services exclusions, updated as of January 9th, 2013 2009 Medicare Payments - Inpatient Stay and 90 Day Bundle Primary Joint Replacement (MS-DRGs 469-470) 10
- 11. Any patient having surgery at pilot hospital for one of the MS-DRGs is by default a part of the bundle; It is not physician-specific How Does Retrospective Bundling Work? Claim from hospital triggers a bundle Patient is flagged by CMS CMS pays all providers as normal All providers bill Medicare as normal Retrospectively the sum of claims is reconciled against the target price If it is LOWER than the target, the awardee will receive a check for the difference If it is HIGHER than the target, the awardee has to repay CMS 11
- 12. 12 All post-acute Medicare costs incurred within the 90d bundle are categorized by the initial post-acute setting (i.e., includes readmissions and other levels of care following the initial setting) Relative Cost of 90 day Episodes of Care by Post-Acute Setting 3-Yr Baseline Period
- 14. Reporting and Monitoring •Bundled Payment Weekly Dashboard – example of physician scorecard Confidential. Do Not Distribute. 14 Discharge Disposition 90-Day Readmission Rate - Closed Episodes Only1 # Patients Discharged ALOS Rehab Facility SNF Total Facility- Based Care HHA Home/ Self Care Total Home- Based Care # Readmissions # Patients 90-Day Readmission Rate Primary Joint of the Lower Extremity 865 3.51 6% 37% 43% 54% 3% 57% 42 338 12% HJD 813 3.41 6% 34% 40% 57% 3% 60% 35 317 11% DRG 469 - Primary Joint w MCC 19 6.84 21% 32% 53% 42% 5% 47% 1 2 50% Physician A 4 6.00 25% 50% 75% 25% 0% 25% 0 0 0% Physician B 4 8.75 25% 25% 50% 50% 0% 50% 0 0 0% Physician C 2 5.47 0% 50% 50% 0% 50% 50% 0 0 0% Physician D 2 4.50 0% 50% 50% 50% 0% 50% 0 0 0% Physician E 2 6.63 100% 0% 100% 0% 0% 0% 0 0 0% Physician F 2 9.35 0% 50% 50% 50% 0% 50% 0 1 0% Physician G 1 3.00 0% 0% 0% 100% 0% 100% 0 0 0% Physician H 1 13.00 0% 0% 0% 100% 0% 100% 0 0 0% Physician I 1 3.00 0% 0% 0% 100% 0% 100% 1 1 100%
- 15. 15 Episodes of Care Initiative Ways to Improve Quality and Efficiency • Reduce readmissions • Reduce LOS • Reduce implant, supply, or drug costs • Reduce OR time • Alter discharge patterns to more cost-efficient settings • Decrease excess utilization (e.g., consults ancillary tests) • Optimize patient health preoperatively • Optimize patient education, care management, pain management, blood management, VTED management and patient expectations Quality improvements and efficiencies will benefit all patients, regardless of payer.
- 16. Clinical Management Throughout the Pathway 16 The Importance of Care Coordination • Enforces best practices / standardization of pathways, workflows, and order sets • Improves communication between providers and to the patient • Ensures follow-up after care transitions • Optimizes Patient Education, Expectations and Outcomes
- 17. Bundled Payment Initiative BPCI Results Y1 • 721 patients were available for analysis at the time at the end of year one. • Average of length of stay was decreased to 3.58 days from 4.27 days (Median LOS 3 days). • Discharge to inpatient facilities has decreased on average from 63% to 44% on average, and 38% for the last month. • Readmissions occurred in 80 of 721 patients, 7% of patients at 30 days, 11% at 60 days and 13% at 90 days which is slightly less than prior to BCPI (17% in 2011, 15% in 2009). • The hospital realized significant cost reduction in the inpatient component year over year. We have achieved positive margins vs. CMS target price in the first three years without accounting for the costs of implementation. We have maintained these margins since the at risk period began in Oct. 2013. 17
- 18. Bundled Payment Initiative – September 2014 18
- 20. Bundled Payment Initiative 20 BPCI Y1 Results •DRG 470: Primary TJA of the Lower Extremity w/o MCC, 17% savings vs. target for Q1 and Q2 reconciliation •For DRG 469: Primary TJA of the Lower Extremity with MCC, 8.1% savings vs. target for Q1 and Q2 reconciliation
- 21. Bundled Payment Initiative Conclusions • We decreased length of stay • We decreased discharges to inpatient facilities • We decreased the cost of the episode of care • We had not significantly altered the readmission rates, but had begun to make inroads • We have implemented a surgeon directed risk factor stratification and modification program to delay surgery in those high risk patients which represent the most likely patients to have complications: 1. Morbid Obesity 2. Uncontrolled Diabetes and poor nutrition 3. Smoking cessation 4. Neurocognitive and Dependency issues 5. VTED 6. Physical deconditioning and Fall Risk 7. Infection prevention, Staph Colonization and Hepatitis C 8. Cardiovascular and Stroke complication prevention • In addition to patient optimization, the introduction of EBM based blood, pain and care management protocols were accomplished 21
- 22. Preventing Hospital Readmissions and Limiting the Complications Associated with Total Joint Arthroplasty Comorbidity Prevalence in NYULMC HJD TJA patients •Musculoskeletal comorbidities 73.8% •Hypertension 60.1% •Hyperlipidemia 55.3% •Tobacco use 22.0% •Diabetes 19.2% •Depressive disorders 14.5% •Ischemic Heart Disease 13.5% •Morbid Obesity 13.8% •Dysrhythmias 10.8% •Valve disease 7.8% •Cerebrovascular Disease 4.4% •CHF 2.8% 22
- 23. Preventing Hospital Readmissions and Limiting the Complications Associated with Total Joint Arthroplasty 23 Severity of Risk Factors Correlates with Financial Risk of Readmission
- 24. Preventing Readmissions Modifiable Risk Factors • MRSA Screening and Decolonization, weight based antibiotic dosing, and use of Vancomycin and Gentamycin in high risk patients, Hepatitis C screening and treatment • Smoking cessation (hard stop) • Cardiovascular Optimization and Stroke Prevention (using PT, High dose Statins, and ACE inhibitors perioperatively) • Aggressive weight control (hard stop at a BMI of 40) • Catastrophizing avoidance, interventions for depression • Drug and alcohol interventions • Fall education prevention • Physical deconditioning and frailty improvement interventions • Diabetes control and nutritional interventions for malnutrition (Hard Stop with glucose > 180) • Screening for high risk VTED patients with testing for thrombophyllia risk • Risk adjusted VTED prophylaxis, use ASA and SPCD’s with standard risk patients, avoid aggressive anticoagulation 24
- 25. Preventing Readmissions Perioperative Orthopaedic Surgical Home: POSH 25
- 26. Preventing Readmissions: The Role of Your Internist POSH Readmission Score and OR of Readmission 26 POSH 0 1 2 3 4 5 6 7 8 Readmitted (A) 21 36 37 45 49 43 24 9 5 None (B) 89 95 39 31 12 3 0 0 0 Ratio = A/B 0.24 0.38 0.95 1.45 4.08 14.33 - - - OR (Linear) 0.19 0.41 0.89 1.94 4.21 9.14 19.86 43.12 93.64 OR (Non-Linear) 0.24 0.38 0.95 1.45 4.08 14.33 - - - OR (Linear, Age) 0.18 0.40 0.90 1.91 4.56 10.23 20.20 44.68 104.24 OR (NL, Age) 0.23 0.37 0.95 1.48 4.26 15.21 - - -
- 27. MJR 90D Readmission Rates before and after POSH 27
- 28. BPCI Discharge Disposition Patterns Primary Joint Replacement 28 n= LOS: 507 5.62 680 4.27 673 3.84 819 3.49 Based on Medicare claims data Fiscal Year: Sept.1 – Aug. 31 869 3.20
- 29. 29 Bundled Payment Initiative - 2015
- 30. Five Pillars of Bundled Payment Success 30 Optimize patient selection and comorbidities Optimize care coordination/patient education/expectations Use a multimodal pain management protocol, minimize narcotics VTED risk standardization and optimized blood management Minimize postacute facility and resource utilization 1 2 3 4 5 VTED = venous thromboembolism disease.
- 31. BPCI Initiative: Clinical Management Throughout the Pathway The Importance of Care Coordination • Enforces best practices/ standardization of pathways, workflows, and order sets • Improves communication between providers and with the patient • Ensures follow-up after care transitions • Optimizes patient expectations and outcomes • Identifies patients who would benefit from preoperative health status optimization 31 Surgeon Preop Visit Preadmission Testing Preoperative Care Preoperative Pathway Skilled Nursing Facility Inpatient Rehab Home Health Agency Outpatient Physical Therapy Surgeon Follow-up Visits Primary Care Visits Postacute Care Shared Postacute Pathways Hospital Acute Care Inpatient Pathway Goal Develop a pathway with >80% use of all elements with exclusion determined by pathway criteria, not physician preference Hospital
- 32. BPCI Care Management/Coordination 32 Pre-hospital Inpatient Post-discharge • Call/meet with patient before surgery – complete preadmission assessment • Confirm contact information • Review preoperative office visits/ PAT results • Ensure Patient Engagement Form is completed and brought to PAT; reinforce Patient Engagement Form • Provide preadmission education and discuss hospital processes • Review expectations around surgical limitations, preparation for after hospital plan and discharge needs/options. • Provide patient with contact information and encourage patient to call back if questions arise • Home visit – high-risk patients - Monitor patient's progress status and readiness for discharge - Monitor the Social Worker and Case/Care Manager to ensure that post-discharge services are in place - Ensure the patient is on track for the expected discharge date and work with the in-hospital team if there are barriers, as needed -Respond to escalation of change in discharge disposition from home to a facility -Maintain communication with the surgeon, discharge planning team and other consults, as needed • Timely and ongoing contact with patients/coaches to monitor progress and identify any issues • Calls and electronic communication to PAC providers • Monitor SNF/IRF patient readiness for CHHA services or outpatient services and necessary follow-up appointments • Monitor CHHA patient readiness for self-care care and any necessary follow-up appointments, including outpatient PT • Alert surgeon and specialty consult(s) when changes have occurred during the postacute period • Follow guidance regarding patients who refuse contact and when not able to contact patients • Plan for and establish closure at the end of the 90-day period
- 33. Conclusions: What Does the Future Hold? Changing the anesthesia and pain management standard of care is needed to achieve desired outcomes Increasing number of same-day discharge total joint arthroplasty patients with continued multidisciplinary approach Discharging many of our total hip arthroplasty (THA) and unicondylar knee replacement patients same day Expanding same-day discharge to total knee arthroplasty (TKA), THA, and total shoulder replacements Training on appropriate injection techniques 33
- 34. Relative Cost of 90-Day Episodes of Bundled Care by Postacute Setting at NYULMC-HJD All postacute Medicare costs incurred within the 90-day bundle are categorized by the initial postacute setting (ie, includes readmissions and other levels of care following the initial setting) 34HHA = home health agency; IP = inpatient; NYULMC-HJD = New York University Langone Medical Center Hospital for Joint Diseases; SNF = skilled nursing facility.
- 35. Postacute Goal – Improved Outcomes and Patient Experience: NYULMC Postacute Partners •Developed in collaboration with partners standard postacute pathways •Focus on: •Bi-directional electronic exchange of information •Twice weekly updates on high- risk patients •Interdisciplinary weekly call •PAC report card •Quarterly PAC committee meeting 35 NYULMC clinicians and staff selected facilities based on a set of rigorous quality and care coordination criteria, taking into account existing clinical relationships, patient geography, and physician discharging preferences. NYULMC = New York University Langone Medical Center; PAC = postacute care.
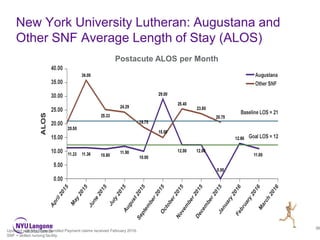
- 36. New York University Lutheran: Augustana and Other SNF Average Length of Stay (ALOS) 36 Updated with Medicare Bundled Payment claims received February 2016. SNF = skilled nursing facility. Postacute ALOS per Month
- 37. Five Pillars of Alternative Payment Methodology Success Conclusions 37 Optimize patient selection and comorbidities Optimize care management/patient education/expectations Use a multimodal pain management protocol, minimize narcotics Venous thromboembolism disease risk standardization and optimized blood management Minimize postacute facility and resource utilization 1 2 3 4 5 Data, transparent data, real-time data, believable data, accurate data…
- 38. Physician Resource Utilization and Quality Analysis 38 Department Average, Physician Discharge, Total Cost
- 39. Implementing Bundled Payment in Your Practice Summary • Care Management, Pain Management, Blood/VTED Management are critical to bringing value to the TJA episode • Optimizing the patient’s medical status and outcomes utilizing the integration of internal medicine, primary care, anesthesiology, physical therapy, bariatrics, nutritional services, endocrinology, cardiology, and psychiatry into the pre- admission and pre-operative preparation process is critical, POSH • Shared Decision making and patient buy-in • NYULMC is developing a risk stratification coordinator position to manage poorly optimized patients, currently this is surgeon driven • In today’s bundled payment and quality driven environment, it is no longer economically feasible to simply accept increased risk in poorly managed patients. We have chosen to take an active role in managing modifiable risk factors and will delay surgery until these risk factors are optimized 39
- 40. Nuances of BCPI 40 Conclusions •Evidence based, cost effectiveness analysis •Standardized protocol adoption •Careful Patient Selection, Preoperative Patient Optimization •Watch out for Prosthetic treatment of Hip Fx, conversion THA, TAA •Transparent data, Physician alignment and Gain sharing, Surgeon Champion •Alternative payment models are an opportunity for AR orthopaedic surgeons to control the episode of care and share in the value generated by high quality, cost effective care •Value based care is the best way to care for our patients
- 41. Thank you 41
- 42. 42 Streamlining Orthopedic Patient Pathways www.wellbe.me/CJR
- 43. 9/14/2016 Confidential ©2014 Wellbe, Inc. – All Rights Reserved. www.labradorhealthcareconsulting.com