Oct 25 CAPHC Concurrent Symposium - Mental Health - Dr. Sharon Clark and Dr. Kathleen Pajer
- 1. The Choice and Partnership Approach (CAPA): Improving the Delivery of Mental Health Care Sharon Clark, Ph.D. Registered Psychologist Advanced Practice Leader: CAPA Kathleen Pajer, M.D., M.P.H. Chief of Psychiatry, Children’s Hospital of Eastern Ontario (CHEO) Professor of Psychiatry University of Ottawa FOM
- 2. Collaborators • Debbie Emberly, Ph.D., IWK • Susan McWilliam, Ph.D., IWK • Emily DeLong, B.S., IWK • Alexa Bagnell, M.D., F.R.C.P.C. • Barb Casey, M.B.A., IWK • William Gardner, Ph.D., CHEO RI • Dave Murphy, CHEO • Marjorie Robb, M.D., CHEO • Karen Tataryn, M.S.W., CHEO • Laura MacLaurin, M.S.W. , The Royal • Christine Slepanki, M.B.A.,The Royal • Gail Beck, M.D., The Royal • Dr. Judy Makinen, Ph.D., C. Psych, The Royal • Rebekah Ranger, BSoc.Sc., BA, The Royal
- 3. Doing the right thing, at the right time, with the right people.
- 4. Overview • What is CAPA? • How is CAPA different from other service delivery systems? • How does CAPA work? • CAPA at three Canadian sites. • Lessons learned. • Questions/Discussion.
- 6. • “You do not have to have a waiting list. It can be eliminated. We need to stop talking about assessment and treatment—things we do to people— and talk instead about partnership and collaboration.” Dr. Ann York, Psychiatrist, CAPA Developer
- 7. • CAPA is innovative method to deliver Child and Adolescent Mental Health Services. • It improves patient flow and quality of care. • Widely used across the UK, New Zealand, Australia. • CAPA makes child and adolescent mental health services: – user-friendly – client/family focused – accessible – safe – effective.
- 9. How is CAPA different from other service delivery systems?
- 11. Fundamental change in philosophy of clinical care. Challenges all assumptions and asks the “system” hard questions: • What is the role of the family in care? • What is the role of the clinician/physician in care? • What is our “core business”? • What is value-added?
- 13. Shared decision making. A consultative process where a clinician and client jointly participate in making a health decision, having discussed the options and their benefits and harms, and having considered the patient’s values, preferences and circumstances. Involves the professional and the service user bringing together their individual sources of expertise
- 14. Shift in responsibility. Family bus ride has already started. • The bus ride doesn’t start start at MH care facility. • The bus ride destination is not the MH care facility. • So, how do we get on the bus with family?
- 15. Value-added care. • Value is anything that improves health, well-being or care experience of patient/family. • Value is defined by patient or family. • We identify the ‘value stream’ or key set of actions required to deliver value. • The trick is to maximize actions that add value and eliminate waste.
- 16. Importance of letting go. “CAPA is all about empowering people and helping them access their own resources – and those in their communities – to move their lives forward. Part of this is not to assume they need services….” CAPA Manual, 2013, p. 81 “Release people back into the wild”
- 17. Mechanics: CAPA uses quantitative approach to service delivery. • Demand and Capacity Theory • Queue Theory • Lean Principles
- 18. Capacity and resources. • A key lever for improving patient flow. • How do we measure capacity? – What is the capacity of a 20 seat restaurant? – A 16 bed ward? • Capacity is a RATE – Customers/hour – Patients/day • We can view a 16 bed ward as a queuing system with 16 servers – What is the capacity of a bed? • A delivery system comprises resources with capacities. – Resources and capacity are not interchangeable; one is a function of the other – Capacity may fluctuate Puterman, Martin, 2012, BHAC 510 Coursework
- 19. Demand and capacity. • Too much capacity or too many resources = idleness • Not enough capacity = waits • Resource manager must trade these off taking into account system objectives and available resources • Should we set capacity equal to demand? – This is called a balanced system – It works perfectly when there is no variation in the system – It works terribly when there is variation! Why? • Once behind, you never can catch up. – Queuing theory quantifies these tradeoffs in terms of performance measures. Puterman, Martin, 2012, BHAC 510 Coursework
- 20. Queuing models. • (Mathematical) queuing models help set capacity (or determine the number of resources needed) to meet: – Service level targets – Average wait time targets – Average queue length targets • Queuing models provide more precise alternative to simulation • They provide insights into how to plan, operate and manage a system Puterman, Martin, 2012, BHAC 510 Coursework
- 21. Push-Pull: the milkman. • Push – the milkman delivers every day • The delivery rate come from the milkman • Pull – the family puts out a bottle when they need milk • The rate comes from the family across continuum ofSlide taken from
- 22. CAPA: Putting it all together. • Demand – Each referral is a request for a clinical service; demand is the number of clinical hours needed • Capacity – Skills bank and resources required to deliver those skills – Skill bank built with targeted recruitment and clinician education – Capacity is not number of clinical staff, but number of clinical hours available to meet demand • Queue estimates used to create job planning. • Lean principles to map out efficient care with least waste.
- 23. How does CAPA work?
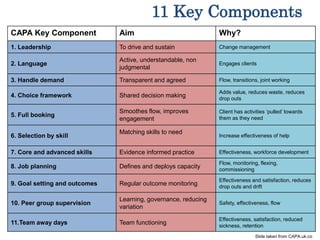
- 24. Slide taken from CAPA.uk.co 11 Key Components CAPA Key Component Aim Why? 1. Leadership To drive and sustain Change management 2. Language Active, understandable, non judgmental Engages clients 3. Handle demand Transparent and agreed Flow, transitions, joint working 4. Choice framework Shared decision making Adds value, reduces waste, reduces drop outs 5. Full booking Smoothes flow, improves engagement Client has activities ‘pulled’ towards them as they need 6. Selection by skill Matching skills to need Increase effectiveness of help 7. Core and advanced skills Evidence informed practice Effectiveness, workforce development 8. Job planning Defines and deploys capacity Flow, monitoring, flexing, commissioning 9. Goal setting and outcomes Regular outcome monitoring Effectiveness and satisfaction, reduces drop outs and drift 10. Peer group supervision Learning, governance, reducing variation Safety, effectiveness, flow 11.Team away days Team functioning Effectiveness, satisfaction, reduced sickness, retention
- 25. 5 BIG ideas. 1. Choice 2. Core and Specific Partnership Work 3. Selecting Core Partnership clinician 4. Job Planning 5. Peer group discussion
- 26. #1 What is Choice? • Choice appointment = first face to face contact • Find out what child, youth and family wants • Use clinical knowledge to collaboratively formulate problem • Choice is single session intervention • Clinician and family design plan to help with problem: – Choice is enough and they can exit or – Return to clinic for treatment matching problem or – Refer to another agency or care provider for better match Slide content taken from CAPA.co.uk
- 27. Choice: menu of treatments. • Establish treatment goals with clients • Match goals with menu of treatments – Methods: group, 1:1, in-home, family, school – Intensity: outpatient, inpatient, acute care, day treatment Intensive services • Consider patient/family’s capacity for change
- 28. #2 Core and Specific Partnership Work Slide content from capa.co.uk
- 29. What is core partnership? • If patient/family will stay at clinic after Choice appointment, then go to Core Partnership – treatment matched to Choice-defined problem and goals, i.e., family “pulls” care in – assigned by reviewing who on team has skills best suited – evidence-based treatments effective across wide range of problems, e.g. CBT – Can be individual or group care – CAPA model suggests average of 7.5 sessions
- 30. Specific Partnership Specific: • When a particular technique, assessment, or skills is needed for specific symptoms or problems as a complement to Core work • Treatment duration is shorter or longer Specific Time examples: – Diagnostic Assessments – Cognitive Assessments Specific Clinics: - OCD - Eating Disorders - Psychosis - PDD
- 31. # 4 Job Planning: Pooling Our Time on Teams.
- 32. Goals to Methods • Better match the treatment options to the goals identified by the client.
- 33. Monday Tuesday Wednesday Thursday Friday 8:30 9:00 10:00 11:00 12:00 1:00 2:00 3:00 4:00 5:00 6:00 7:00 Team Meetin g Discipline Meeting Specific: Cognitive Ax Choic e Partner ship Partner ship Partner ship Priority Ax Group Big Admin Carepat h # 4 Job planning.
- 34. #5: Peer group discussion.
- 35. Weekly peer group discussion. • Weekly meetings of all clinicians on team: – Discuss Choice appointment outcomes – Distribute workload – Do clinical peer supervision • Purpose – Builds trust within teams – Supports “letting go” – Specifies clear treatment goals and monitoring using outcome measures – Helps develop a learning culture – Reduces variability in responses to client’s needs – Increases safety and risk management
- 36. CAPA at three Canadian Sites.
- 37. IWK Health Centre • IWK Mental Health Program - Mandate for service delivery across continuum of care - total of 400 allied professionals and support staff providing care across multiple service areas and 17 psychiatrists - CAPA started April 2012 in outpatient teams 2015/16 Data:
- 38. 0 50 100 150 200 250 300 350 400 450 500 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 2011-2012 2012-2013 2013-2014 2014-2015 2015-2016 2016- 2017 Referral to Choice: Regular Overall CMHA # of New Patients Average wait Source: IWK Community Wide Scheduling
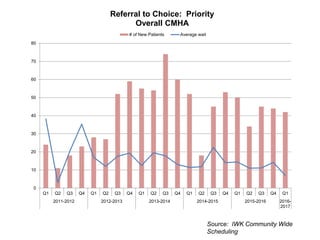
- 39. Source: IWK Community Wide Scheduling 0 10 20 30 40 50 60 70 80 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 2011-2012 2012-2013 2013-2014 2014-2015 2015-2016 2016- 2017 Referral to Choice: Priority Overall CMHA # of New Patients Average wait
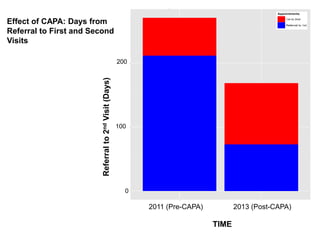
- 40. Effect of CAPA: Days from Referral to First and Second Visits TIME 2011 (Pre-CAPA) 2013 (Post-CAPA) 0 100 200 Referralto2ndVisit(Days)
- 42. CHEO • CHEO Mental Health Program, Outpatient Service: – Psychiatry Dept. (3.4 FTE) provides all psychiatric care – 12.5 total FTE allied health professionals and support staff – 15/16: 1479 referrals to Outpatient; 8715 visits; all off site; Outpatient Eating Disorders is separate – In care partnership with the Youth Program at The Royal Ottawa Hospital: Young Minds Partnership
- 43. Progress to date • Pre-CAPA: wait time to first appointment = average 200 days • Current wait time: 4.5 weeks • Current wait time for Partnership (excluding groups) = 8 weeks • Skills and competencies assessment identified following gaps: – Trauma care, brief interventions, some group therapies, family therapy
- 44. The Royal Ottawa Hospital • The Royal is specialized mental health centre to treat people with complex, serious mental illness in Eastern Ontario. • The Youth Program provides intensive, specialized mental health services to 16-18 year-old youth with early onset major psychiatric disorders or complex psychiatric illnesses resistant to treatment. • Number of clinicians and psychiatrists = 15 • Waitlist blitz – early 2015; CAPA March 2016
- 45. Progress to date • Wait times: – January 2015 ~ 18 months (blitz) – March 2016 ~ 2 months – Currently ~ 4 weeks
- 46. Progress to date • Parent Choice experience (N = 16) “Overall, the help I had here was good.” All true 84.6% Partly true 7.7% Don’t know 7.7% “Did you feel that people here listened to your concerns?” Very much 92.3% Pretty much 7.7% “Was today’s session helpful for you?” Very much 69.2% Pretty much 15.4% A little 15.4%
- 47. Client & Clinician Ratings/Choice (N = 23) Q1 – “How much were they/you curious about their/your view point…?” RESPONSE CLIENT CLINICIAN None 0% 0% A little 0% 0% Some 8.7% 0% A fair bit 8.7% 9.5% A lot 39.1% 47.6% Loads 43.5% 42.9%
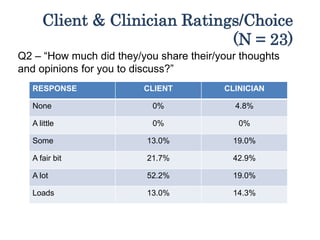
- 48. Client & Clinician Ratings/Choice (N = 23) Q2 – “How much did they/you share their/your thoughts and opinions for you to discuss?” RESPONSE CLIENT CLINICIAN None 0% 4.8% A little 0% 0% Some 13.0% 19.0% A fair bit 21.7% 42.9% A lot 52.2% 19.0% Loads 13.0% 14.3%
- 49. Client and Clinician Ratings/Choice (N = 23) Q3 – “How much did they/you come to a share view as the nature of their/your problems?” RESPONSE CLIENT CLINICIAN None 0% 0% A little 0% 0% Some 8.7% 0% A fair bit 8.7% 9.5% A lot 39.1% 47.6% Loads 43.5% 42.9%
- 50. Lessons learned.
- 51. Key CAPA elements • Systematic evaluation of progress: use data to inform decision-making. • Fidelity is critical. • Mechanics done without philosophy change is “doing to” our clients, not “engaging with” them. • Need to build continuous skill development: – Choice Clinic = pushing out the private practice model and building trust. – Team Peer Supervision = creating an environment where clinicians can ask for help. – Developing clinical capacity in specific clinics to strengthen core skills.
- 53. Lessons learned. • Program administration needs to be actively supporting CAPA • Achieving flow of patients means radically new thinking. • Change will come in waves. • People may accept CAPA and then drift back to old ways. • The power of families as collaborators is freeing. • Stick with it. • Share what you’ve learned. • Find mentors and stay in close communication. • Fidelity to model is critical.
- 54. Resources • All the CAPA ideas and concepts presented today were developed by Drs. Steve Kingsbury and Ann York. • Please see the http://www.capa.co.uk/ website for more information or refer to their publication: The Choice and Partnership Approach: A Service Transformation Model (2013)