Penicillium
- 1. Name: Purshotam Kumar Sah Kanu Roll No.: MB 1318/075 Level: M.Sc Microbiology (3rd Sem) Central Department of Microbiology Tribhuvan University, Kirtipur Kathmandu, Nepal MB 609 Systemic and Diagnostic Mycology
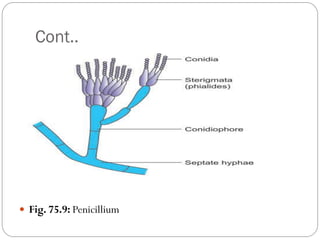
- 2. Penicilliosis Penicillium species rarely cause opportunistic infections in humans. The Penicillium species are identified by their typical morphology (Fig. 74-6), culture characteristics on the SDA medium (Color Photo 69), and microscopy (Color Photo 70). P. marneffei is the only dimorphic fungus in the genus Penicillium known to cause opportunistic infection. There are more than 150 known species of the genus Penicillium.
- 3. Cont.. Fig. 75.9: Penicillium
- 4. Cont.. P.marneffei causes disseminated infection in immunocompromised hosts, such as patients with HIV. It develops a necrotizing reaction and involves the skin, lung, and intestine. It causes disseminated infections of reticuloendothelial system, and also allergic diseases and mycotoxicoses. The disseminated infection is more common in adults than in children. P.marneffei is widely distributed in the nature. Its natural habitat is soil.
- 5. Cont.. The fungus infects no mammals other than humans and bamboo rat. Fungus is found in feces of rats and also in burrows made by the rats in the soil. The infection is transmitted by inhalation of conidia, direct inoculation of the skin, and rarely, by ingestion of infected rats. The condition is more common in rainy season, in rural areas.
- 6. Physiology The fungus, which is a dimorphic fungus, grows rapidly on SDA. At 25°C, it grows as a mold and produces greenish yellow colonies with dark green edge and pink or red center. It exhibits brick red pigment on the reverse. At 37°C, it grows as small yeast, producing cream-colored mucoid colonies resembling Histoplasma capsulatum.
- 7. Pathogenesis Incubation period is variable from few weeks to years. P.marneffei causes asymptomatic infections in immunocompetent hosts. It causes granulomatous or suppurative reaction, Bronchopneumonia with or without adenopathy, and cavitary lung lesion. It produces chronic cervical lymphadenitis resembling tuberculosis. Disseminated infections occur rarely in immunocompetent hosts.
- 8. P.marneffei causes disseminated infection in immunocompromised hosts, such as patients with HIV. It develops a necrotizing reaction and involves the skin, lung, and intestine. It causes disseminated infections of reticuloendothelial system, and also allergic diseases and mycotoxicoses. The disseminated infection is more common in adults than in children.
- 9. Epidemiology P.marneffei is widely distributed in the nature. Its natural habitat is soil. The fungus infects no mammals other than humans and bamboo rat. Fungus is found in feces of rats and also in burrows made by the rats in the soil. The infection is transmitted by inhalation of conidia, direct inoculation of the skin, and rarely, by ingestion of infected rats. The condition is more common in rainy season, in rural areas.
- 10. Immunity Cell-mediated immunodeficiency, steroid treatment, and HIV infection are predisposing factors.
- 11. Laboratory Diagnosis 1.Microscopy: Demonstration of P.marneffei in the skin and mucosal scrapings, sputum, stool, blood, urine, lymph node, bone marrow, lung and liver biopsy specimens. 2.Staining: Staining of skin, lymph node, and bone marrow aspirate by hematoxylin and eosin, PAS (periodic acid-Schiff),Wright’s, and calcofluor white stain demonstrates yeast cells with transverse septa.
- 12. Cont.. 3.Histological test: Immunohistochemical assay using monoclonal antibody against an external wall epitope is used to identify P.marneffei in tissues. Demonstration of fungal antigen in affected tissue by using direct immunofluorescence antibody also helps in diagnosis of the condition. Peripheral blood smear shows P.marneffei in patients with AIDS.
- 13. Cont.. 4.Culture: Culture is the gold standard. P.marneffei is a highly infectious fungus, hence culture should be done in a laboratory with a biohazard safety level-2 precautions. The fungus on SDA without cycloheximide and at 25°C produces mycelial grayish white colonies, green center, white periphery, and bright rose pigmented reverse (Color Photo 71). Microscopy of the colony shows septate hyaline hyphae, branched conidiophores, and three to five medullae which produce phialides that bear conidia in chains. The fungus on SDA at 37°C produces yeast-like colonies and cream- colored mucoid with brown red pigment. Microscopy of the colony shows pleomorphic ellipsoidal to rectangular yeast cells with transverse septum
- 14. COLOR PHOTO 71. SDA medium showing colonies of Penicillium marneffei. COLOR PHOTO 70. LPCB wet mount showing Penicillium (×100).
- 15. Cont… 5.Serological test: Indirect immunofluorescent antibody test, immunoblot assay, and immunodiffusion method using mycelial phase culture antigen are used to demonstrate serum IgG antibodies. Immunodiffusion and latex agglutination tests are used to detect P.marneffei antigen in serum and urine.