REPRODUCTIVE DISORDERS-FENWICK, FILAMER
- 1. Reproductive System ( Disorders ) Group 5 BSN III Fenwick
- 2. P himosis A state in which the male foreskin is unable to retract properly from the head of the penis (or glans). This is due to an unusually tight foreskin
- 3. Types of Phimosis A. Infantile or congenital phimosis (in infants) Infants are born with Phimosis B. Acquired phimosis (adult men) Phimosis is the result of repeated foreskin infections such as balanitis. Also linked with neglected hygiene A B
- 4. Schematic Diagram Uncleaned Preputial Normal Secretion Balanitis Secretions Thickened Adhesion Encrusted with urinary salts and calcify Fibrosis Forming calculi in prepuce Interfere with urinary elimination and intercourse Malignant changes of the penis
- 5. Diagnosis Physical examination Check pubic and axillary hair distribution. Palpate the penis, scrotum, prostate gland, and rectum. Inspect the penis for lesions, swelling, inflammation, scars, or discharge. In the uncircumcised male, retract the foreskin to visualize the glans. Examine the scrotum for size, shape, and abnormalities, such as nodules or inflammation. Check for the presence of both testes
- 6. Complications Problems urinating Problems and pain during intercourse Infections under the foreskin Frequent and recurrent infections under the foreskin, which can be avoided by cleaning regularly under the foreskin with lukewarm water At erection, a contracted foreskin may cause trouble by hurting when an attempt is made to pull the foreskin back A small chance of malignant growth in a long-standing foreskin contraction.
- 7. Nursing Assessment Pain Penile swelling Penile inflammation Penile discharge Penile bleeding Swelling of penis on urination Urination difficulties Pain on urination Red, swollen, and tender foreskin Inability to retract foreskin Straining during urination Thin stream of urine Recurrent urinary infections
- 8. Surgical Intervention Circumcision Medical Intervention Stretching (stretching of the foreskin can be acheived by a metal calliper or a balloon device) Steriod Cream (Betamethasone has been proven to assist with making the foreskin stretch and should be used more often especially in combination with the balloon or calliper technique of stretching)
- 9. Stretch Plus Steriod Cream (This combination should be used as often as clinically indicated and will give the best non surgical outcomes and results should be long term) Levels of Care Proper hygiene Proper Diet (more on vegetables) Taking of vitamins Promotive
- 10. Keep the penis and foreskin clean. Avoid sexually transmitted disease: Do not have sex with multiple sexual partners. Do not have with anyone who has oral or genital sores. Do not have sex with anyone who has a penile discharge or vaginal discharge. Do not have sex with a partner who has intercourse with others. Practice safe sex: Preventive
- 11. Circumcision Stretching (stretching of the foreskin can be acheived by a metal calliper or a balloon device) Steriod Cream (Betamethasone has been proven to assist with making the foreskin stretch and should be used more often especially in combination with the balloon or calliper technique of stretching) Stretch Plus Steriod Cream (This combination should be used as often as clinically indicated and will give the best non surgical outcomes and results should be long term) Curative Rehabilitative Maintain good personal hygiene Follow up check-up with your urologist
- 12. H ypospadia Hypospadias is a male birth defect in which the opening of the tube that carries urine from the body ( urethra ) develops abnormally, usually on the underside of the penis. The opening can occur anywhere from just below the end of the penis to the scrotum.
- 13. One distinguishes various anatomic variants Hypospadia of the glans penis is characterized by a urinary meatus on the underside of the glans. With a hypospadia of the penile shaft , the urinary meatus is in the middle of the penis. hypospadia of the scrotum the fusion of the genital swellings is absent and a urethral opening at the level of the scrotum remains.
- 14. Etiology Genetic factors A genetic predisposition has been suggested by the 8-fold increase in incidence of hypospadias among monozygotic twins compared with singletons. Familial trend with hypospadias Endocrine factors A decrease in available androgen or an inability to use available androgen. Endocrinopathies or fetal endocrine abnormalities. Environmental factors Environmental substances with significant estrogenic activity are ubiquitous in industrialized society and are ingested as pesticides on fruits and vegetables, endogenous plant estrogens, in milk from lactating pregnant dairy cows, from plastic linings in metal cans, and in pharmaceuticals. An increase in estradiol concentration in placental basal syncytiotrophoblasts of boys with undescended testes compared with a control population
- 15. Assessment Mild hypospadias usually does not cause symptoms, especially in newborns and young children. If not surgically corrected, older children and adults may complain of difficulty directing their urinary stream and spraying urine. More severe cases of hypospadias make it impossible to urinate while standing. Boys with hypospadias are also more likely to have an undescended testicle .
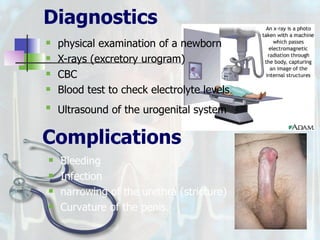
- 16. Diagnostics physical examination of a newborn X-rays (excretory urogram) CBC Blood test to check electrolyte levels Ultrasound of the urogenital system Complications Bleeding Infection narrowing of the urethra (stricture) Curvature of the penis.
- 17. Nursing diagnoses Risk for impaired skin integrity related to problems in managing the urine collection appliance Acute pain related to surgical incision Potential for sexual dysfunction related to structural and physiologic alterations Deficient knowledge about management of urinary functins
- 18. Interventions Surgical repositioning of the urethra correcting the placement of the urethral opening in the head of the penis reconstructing the skin of the area around the urethral opening Note: a baby with hypospadias should not be circumcised . Surgical Complications General Anesthetic side effects Post-operative bleeding following repair hypospadias Post operative bladder spasm following repair hypospadias Infection following repair hypospadias Post operative urethral stenosis following repair hypospadias Post operative fistula following repair hypospadias
- 19. Curative Surgery repositioning of the urethra correcting the placement of the urethral opening in the head of the penis reconstructing the skin of the area around the urethral opening Thiersch-Duplay repair For the more distal defects that have openings closer to the normal position at the end of the penis, a new tube can be created from the surrounding skin Levels of Care
- 20. Rehabilitative Always do aseptic technique after post operation especially if the child has a tube to prevent infection. Child will be allowed to have sponge baths until dressing is removed. Tub baths may begin when the dressing falls off or two days after the surgery Avoid applying powder or ointments to the childs genital area. Encourage fluids to keep your son's urine clean.
- 21. E pispadias A birth defect due to malformation of the URETHRA in which the urethral opening is above its normal location. In the male, the malformed urethra generally opens on the top or the side of the PENIS, but the urethra can also be open the entire length of the penis. In the female, the malformed urethral opening is often between the CLITORIS and the labia, or in the ABDOMEN." Overview The deformity manifests in males. The normal urethra is replaced by a broad mucosal strip lying on the dorsum of the corpora cavernosa; the meatus is divided dorsally between the tip of the glans and the pubis, the penile shaft is curved dorsally with the absence of the preputial apron, and a cleft is present on the upper surface of the penis.
- 22. 3 types of Epispadias A. Glandular Type Affects the distal part of the urethra. B. Penile type Entire penile urethra is affected, with an external meatus on the dorsal shaft of the penis C. The complete or Penopubic type A total deficiency of the dorsal wall of the urethra and the anterior wall of the bladder is present A B C
- 23. Etiology Epispadias are unknown at this time. Related to improper development of the pubic Associated with bladder exstrophy, Epispadias can also occur alone or with defects. Assessment In males: Abnormal opening from the joint between the pubic bones to the area above the tip of the penis Backward flow of urine into the kidney (reflux nephropathy) Short, widened penis with an abnormal curvature Urinary tract infections Widened pubic bone
- 24. In females: Abnormal clitoris and labia Abnormal opening where the from the bladder neck to the area above the normal urethral opening Backward flow of urine into the kidney (reflux nephropathy) Widened pubic bone Urinary incontinence Urinary tract infections Diagnostics Blood test to check electrolyte levels Intravenous pyelogram (IVP), a special x-ray of the kidneys, bladder, and ureters Pelvic x-ray Ultrasound of the urogenital system chest radiograph (if indicated based on examination findings or the patient's history) CBC Pelvic x-ray Intravenous pyelogram (IVP)
- 25. Complications Bleeding Infection wound separation Flap necrosis Edema. Urethrocutaneous fistula with urinary leakage Persistent urinary incontinence Upper urinary tract (ureter and kidney) damage Infertility Nursing diagnoses Risk for impaired skin integrity related to problems in managing the urine collection appliance Acute pain related to surgical incision Potential for sexual dysfunction related to structural and physiologic alterations Deficient knowledge about management of urinary functions
- 26. Medical Interventions No medical treatment corrects epispadias Surgical Surgical repair of epispadias is recommended in patients with more than a mild case. Leakage of urine (incontinence) is not uncommon and may require a second operation.
- 27. 1.Distal penile epispadias 2. Wide diastasis of the pubic bone and external displacement of the hips in epispadias. 3. Distal epispadias. Outlining of local flaps from the glans to reconstruct the distal urethra. 4.Vertical island flap drawn on the ventral aspect of the penis 5. Island flap transferred dorsally and anastomosed to the urethra. 6. Island flap sutured into a tube to reconstruct the missing portion of the urethra 7. Urethral reconstruction is completed 8. Drawing of the final appearance at the end of the operation. 9. Final Apperance
- 28. Promotive Engage in activity such as genetic counseling Immunization against infectious diseases Good nutrition Careful genital hygiene Healthy sexual practices Nursing Intervention Preventive Screening Self examination Curative Surgical repair Rehabilitative Don't apply powder or ointments to the genital area. If your child has loose bowel movements and soils his surgical dressing, clean it gently with soapy water and a washcloth, away from his penis.
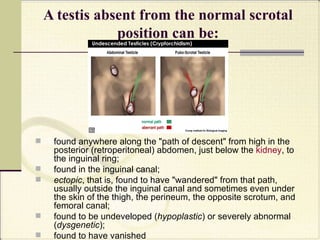
- 29. C ryptorchidism It is the absence of one or both testes from the scrotum . This usually represents failure of the testis to move, or "descend," during fetal development from an abdominal position, through the inguinal canal , into the ipsilateral scrotum.
- 30. A testis absent from the normal scrotal position can be: found anywhere along the "path of descent" from high in the posterior (retroperitoneal) abdomen, just below the kidney , to the inguinal ring; found in the inguinal canal; ectopic , that is, found to have "wandered" from that path, usually outside the inguinal canal and sometimes even under the skin of the thigh, the perineum, the opposite scrotum, and femoral canal; found to be undeveloped ( hypoplastic ) or severely abnormal ( dysgenetic ); found to have vanished
- 31. Etiology Severely premature infants Hormonal abnormalities(deficiency or insensitivity to androgens or anti-müllerian hormone) Regular alcohol consumption during pregnancy (5 or more drinks per week) Exposure to pesticides (mother during pregnany) Low birth weight Gestational diabetes Multiple pregnancy Diagnostic Tests Pelvic ultrasound Magnetic Resonance Imaging Karyotyping
- 32. Complications Reduced fertility Lower sperm counts Testicular cancer ( Seminoma ) Surgical Procedures Orchiopexy Auto-transplantation of testis into the scrotum Complications after Surgery Ischemic Atrophy of the testis Fibrosis of the testis Loss of blood supply to the testis Medical Intervention hCG injections (10 injections over 5 weeks) GnRH analogs such as nafarelin or buserelin
- 33. Assessment Palpation of the testis Assess patients family history regarding testicular cancer Assess weight Assess the position of the testis absent from the normal scrotal position. Assess mother from alcohol consumption during pregnancy Alteration in comfort due to pain Fear related to diagnosis Risk for infection due to bacterial invasion of wound or bladder Powerlessness due to physical condition Ineffective individual and family coping related to infertlity and family relationship Nursing Diagnoses
- 34. Promotive Proper diet during pregnancy to avoid gestational diabetes. Follow prenatal check-up as scheduled. Knowledge about the occurrence of the disease Knowledge of family health history regarding specifically the occurrence of Cryptorchidism to minimize risk factors and add awareness (genetic counseling) Nursing Intervention Preventive Pregnant mother should avoid exposure to pesticides Mothers should avoid alcohol consumption throughout pregnancy. Pregnant mothers should minimize or avoid caffeine consumption if possible. Curative Orchiopexy Auto-transplantation of testis into the scrotum hCG injections (10 injections over 5 weeks) GnRH analogs such as nafarelin or buserelin Rehabilitative Wear of scrotal support Avoid tight clothing
- 35. H ydrocele Hydroceles are fluid collections within the tunica vaginalis of the scrotum or along the spermatic cord. These fluid collections may represent persistent developmental connections along the spermatic cord or an imbalance of fluid production versus absorption. Rarely, similar fluid collections can occur along the canal of Nuck in females
- 36. Structurally, Hydroceles are classified into 3 principal types In a communicating (congenital) hydrocele, a patent processus vaginalis permits flow of peritoneal fluid into the scrotum. Indirect inguinal hernias are associated with this type of hydrocele. In a noncommunicating hydrocele, a patent processus vaginalis is present, but no communication with the peritoneal cavity occurs. In a hydrocele of the cord, the closure of the tunica vaginalis is defective. The distal end of the processus vaginalis closes correctly, but the mid portion of the processus remains patent. The proximal end may be open or closed in this type of hydrocele.
- 37. Etiology Most pediatric hydroceles are congenital; however, consider malignancy, infection, and circulatory compromise. Hydrocele of the cord is associated with pathologic closure of the distal processus vaginalis, Communicating hydrocele is caused by failed closure of the processus vaginalis Noncommunicating hydrocele results from pathologic closure of the processus vaginalis and trapping of peritoneal fluid. Adult-onset hydrocele may be secondary to orchitis or epididymitis .
- 38. Can be caused by tuberculosis and by tropical infections such as filariasis. Testicular torsion may cause a reactive hydrocele Tumor, or tumors of the testicular adnexa may cause hydrocele. Traumatic (ie, hemorrhagic) hydroceles are common. Ipsilateral hydrocele occurs after renal transplantation. Radiation therapy is associated with cases of hydrocele. Exstrophy of the bladder may lead to hydrocele. Hydrocele may arise from Ehlers- Danlos syndrome . Hydrocele may result from a change in the type or volume of peritoneal fluid
- 39. Diagnostic Tests CBC Urinalysis Inguinal-scrotal imaging ultrasound Doppler ultrasound flow study Testicular scintigraphy Abdominal x-ray Testicular Scintigraphy Surgical procedures Transillumination Hydrocele aspiration Inguinal incisions with high ligation of the patent processus vaginalis and excision of the distal sac.
- 40. Complications An extremely large hydrocele may impinge on the testicular blood supply. The resulting ischemia can cause testicular atrophy and subsequent impairment of fertility. Hemorrhage into the hydrocele can result from testicular trauma. Incarceration or strangulation of an associated hernia may occur. Surgical Complications Accidental injury to the vas deferens Postoperative wound infections Postoperative hemorrhagic hydrocele Direct injury to the spermatic vessels
- 41. Nursing Assessment Most hydroceles are asymptomatic or subclinical. Evaluate the onset, duration, and severity of signs and symptoms. Identify any relevant genitourinary (GU) history, sexual history, recent trauma, exercise, or systemic illnesses. The usual presentation is a painless enlarged scrotum. The patient may report a sensation of heaviness, fullness, or dragging. Patients occasionally report mild discomfort radiating along the inguinal area to the mid portion of the back. Hydrocele usually is not painful; pain may be an indication of an accompanying acute epididymal infection. The size may decrease with recumbency or increase in the upright position. Chronically formed hydroceles appear to be larger in size than acutely formed ones. Systemic symptoms such as fever, chills, nausea, or vomiting are absent in uncomplicated hydrocele. GU symptoms are absent in uncomplicated hydrocele.
- 42. Hydrocele usually is not painful; pain may be an indication of an accompanying acute epididymal infection. The size may decrease with recumbency or increase in the upright position. Chronically formed hydroceles appear to be larger in size than acutely formed ones. Systemic symptoms such as fever, chills, nausea, or vomiting are absent in uncomplicated hydrocele. GU symptoms are absent in uncomplicated hydrocele. Nursing Diagnoses Body image disturbance related to size of Hydrocele Alteration in comfort due to pain Fear related to diagnosis Risk for infection due to bacterial invasion of wound or bladder Powerlessness due to physical condition
- 43. Preventive Screening Self examination Curative Surgical procedure Transillumination Hydrocele aspiration Inguinal incisions with high ligation of the patent processus vaginalis and excision of the distal sac. Wear of scrotal support Avoid tight clothing Rehabilitative Nursing Intervention Promotive In adults with Hydrocele and for Mothers Proper Diet Engage in activity such as genetic counseling Immunization against infectious diseases Good nutrition Careful genital hygiene Healthy sexual practices
- 44. V aricocele Varicocele is an abnormal enlargement of the veins in the scrotum draining the testicles . The testicular blood vessels originate in the abdomen and course down through the inguinal canal as part of the spermatic cord on their way to the testis . Up-ward flow of blood in the veins is ensured by small one-way valves that prevent backflow. Defective valves, or compression of the vein by a nearby structure, can cause dilatation of the veins near the testis, leading to the formation of a varicocele.
- 45. Idiopathic varicocele Occurs when the valves within the veins along the spermatic cord don't work properly. This results in backflow of blood into the pampiniform plexus and causes increased pressures, ultimately leading to damage to the testicular tissue. Secondary varicocele Is due to compression of the venous drainage of the testicle. One non-malignant cause of a secondary varicocele is the so-called " SMA " ( superior mesenteric artery ), a condition in which the superior mesenteric artery compresses the left renal vein, causing increased pressures there to be transmitted retrograde into the left pampiniform plexus.
- 46. Diagnostic tests Physical Examination Ultrasound Doppler ultrasound Complications Infertility Testicular Atrophy Medical Intervention Scrotal support (e.g. jockstrap , briefs ) Vasotonic drugs Surgical Intervention Varicocelectomy The three most common approaches: inguinal (groin), retroperitoneal (abdominal) infrainguinal/subinguinal (below the groin) Embolization Surgical ligation A 2- to 3-inch incision is made in the groin or lower abdomen, the affected veins are located visually, and the surgeon cuts the veins and ties them off above the varicocele to reroute the blood through unaffected veins
- 47. Complications after Surgery Hematoma Injury to the scrotal tissue or structures Infection Nursing assessment Dragging-like or aching pain within scrotum . Feeling of heaviness in the testicle(s) Infertility Atrophy (shrinking) of the testicle(s) Visible or palpable (able to be felt) enlarged vein Body image disturbance related to size of varicocele Alteration in comfort due to pain Fear related to diagnosis Risk for infection due to bacterial invasion of wound or bladder Powerlessness due to physical condition Nursing Diagnoses
- 48. Preventive Scrotal support (e.g. jockstrap , briefs ) Vasotonic drugs Promotive Proper Diet Engage in activity such as genetic counseling Immunization against infectious diseases Good nutrition Careful genital hygiene Healthy sexual practices
- 49. Curative Varicocelectomy The three most common approaches: inguinal (groin), retroperitoneal (abdominal) infrainguinal/subinguinal (below the groin) Embolization Surgical ligation Laparoscopy Rehabilitative Wear of scrotal support Avoid tight clothing
- 50. P ROSTATE CANCER Prostate cancer is a disease in which cancerous cells develop in the prostate, one of the male sex glands. Cancer of the prostate is one of the most commonly occurring cancers in men in the United States. Although the cause of the disease is not known, we do know that the growth of cancer cells (like normal cells) is stimulated by male hormones, particularly testosterone.
- 51. The Prostate Gland The prostate is about the size of a walnut and is located just below the bladder. It functions as part of the male reproductive system by secreting a slightly alkaline fluid that forms part of the seminal fluid.
- 52. ETIOLOGY Although the etiology is unknown, this condition is hormone dependent. Prostate cancer is the second most common cancer in man Incidence is extraordinarily rare in men under the age of 40. However, most prostate cancer is occult; only 1% to 2% of men in the ninth decade of life annually manifest clinical evidence of new prostate cancer . ASSESSMENT Weak or interrupted flow of urine Frequent urination (especially at night) Difficulty urinating or holding back urine Inability to urinate Pain or burning when urinating or ejaculation Blood in the urine or semen Nagging pain in the back, hips, or pelvis
- 53. Loss of mobility adenoncarcinoma Normal semen-secreting prostate gland cells mutate into cancer develop in peripheral zones of the prostate gland Begin to multiply Tumor enlarges metastasis This location increases the risk of local spread to the prostatic capsule Compress urethra Lymph/venous circulation Seminal vesicle/bladder Compression fracture Obstruct the urinary flow bone Blood upon ejaculation hematuria Joint and back pain Migratory pain hematuria dysuria nocturia
- 54. DIAGNOSTICS (pre-intra-post) 1. Routine prostate screening annual physical examination digital rectal examination (DRE) an examination performed in a physician's office in which the doctor inserts a gloved, lubricated finger into the rectum in order to feel the prostate. a prostate-specific antigen (PSA) test is a blood test in which the blood is examined to look for PSA, a substance that often increases in a man who has prostate cancer or another prostate disease. If a man's PSA levels are high compared to others in his age group, there is a higher chance that he may have prostate cancer.
- 55. 2. Prostate Biopsy 3. Endorectal magnetic resonance imaging 4. Molecular Staging 5. Axial imaging (CT, MRI) 6. Bone scan
- 56. COMPLICATIONS Spread of cancer Pain Difficulty urinating (urinary incontinence) Erectile dysfunction (ED) or impotence . Depression NURSING DIAGNOSES Anxiety related to concern and lack of knowledge about the diagnosis, treatment plan, and prognosis Urinary retention related to urethral obstruction secondary to prostatic enlargement or tumor and loss of bladder tone to prolonged distension/retention Sexual dysfunction related to effects of therapy, chemotherapy, hormonal therapy, radiation therapy, surgery Pain related to progression of disease and treatment modalities Impaired physical mobility and activity intolerance related to tissue hypoxia, malnutrition and exhaustion and to spinal cord or nerve compression from metastases
- 57. INTERVENTIONS Medical It is based on the stage of the disease and the patient’s age and symptoms. A nomogram (PSA level combined with clinical stage and pathologic grade of the tumor) can be useful in making treatment decisions and predicting treatment outcomes Radiation therapy External beam therapy Brachytherapy Estrogen Therapy LHRH Analog Therapy Antiandrogen Therapy Chemotherapy Watchful waiting
- 58. B. Surgical Prostatectomy Transurethral Resection of the Prostate Cryosurgery Orchiectomy (Surgical Removal of the Testicles) Nursing Intervention Promotive Eat well Get regular exercise Ask your doctor about taking an NSAID Preventive No specific measures are known to prevent the development of prostate cancer. At present, therefore, we can hope only to prevent progression of the cancer by making early diagnoses and then attempting to cure the disease.
- 59. Curative Radiation therapy External beam therapy Brachytherapy Estrogen Therapy LHRH Analog Therapy Antiandrogen Therapy Chemotherapy Watchful waiting Prostatectomy Transurethral Resection of the Prostate (TURP) Cryosurgery Orchiectomy (Surgical Removal of the Testicles) Rehabilitative Continuous follow-up is essential for all ovarian cancer patients.. Most patients are examined by their physicians every 3 months for the first 2 years. During each visit, the physician will check the CA125 level in the patient's blood. Sexual Concerns -the surgery that is performed to treat ovarian cancer will result in sexual changes Menopausal symptoms can be treated hormonally psychological and/or sexual counseling.
- 60. O varian Cancer Cancer begin in cells. Normally, cells grow and divide to form new cells as the body needs them. When cells grow old and die, and new cells tale their place. Sometimes, this orderly process goes wrong. New cells form when the body does not need them, and old cells do not die when they should. These extra cells can form a mass of tissue called a growth or tumor. Pathophysiology Predisposing Factors Family history of any cancer Personal of breast cancer Age: Postmenopausal (<40) Early menarche Late menopause Genetic predisposition Race: white Precipitating Factors Prolonged use fertility drugs with achieving pregnancies First child after 30 years old Multipara Use of talc powder in genital area. High fat diet Obese Diet: low in fruits and vegetables
- 61. Mutation inactivates tumor suppressor gene Cell proliferate Mutation inactivates DNA repair gene Mutation of proto-oncogene creates an oncogene Mutation inactivates more suppressor genes Ovarian surface epithelium tumor grow Invades organs next to ovaries such as fallopian tubes and uterus Cancer cells shed into abdomen New tumor develop Spread Lymphatic System Blood stream Affects lymph nodes Affects liver and lungs Blocks lymphatic drainage in the abdomen Ascites
- 62. Diagnostic tests Blood tests CBC Serum electrolyte test Serum BHCG level Serum alpha – letoprotein Lactate dehydrogenase CA-125 Pelvic examinations CT Scan Transvaginal Ultrasound Physical Exam MRI Paparoscopy Pap Smear X-ray Complications Spread of the cancer to other organs Progressive function loss of various organs Ascites Intestinal obstruction
- 63. Medical Intervention Hysterectomy TAHBSO with Omentectomy Surgical Debulking Chemotherapy Cyclophophamide Cisplatin Paclitaxel (Taxol) and Carhoplatin (paraplatin) – IV Immunotherapy Bavacizumab (Avastin) Liposmal Therapy Hormonal therapy with Tamoxifen (Tamofen) Gene Therapy Radiation a. Intraoperative Radiation Therapy b. Internal (intractivity) Irradiation c. External Beam Radiation Therapy (EBCT) Surgical Intervention Complications after Surgery Hemorrhage Deep vein thrombosis Bladder Dysfunction Nursing Intervention Health Teaching
- 64. Assessment Obtain history of irregular menses, pain, postmenopausal bleeding. Ask about vague gastrointestinal-related complaint. Ask about history of other malignancy and family history of breast or ovarian cancer. Assess patient’s general health status in terms of tolerating surgical and adjuvant therapy. Nursing Diagnoses Health seeking behaviour related to altered health status. Deficient knowledge related to new condition, procedure, treatment. Deficient knowledge related to emotional state affecting learning. Anticipatory grieving due to perceived potential loss of physiopsycosocial possession. Ineffective coping related to recent change in health status and diagnosis of serious illness Ineffective sexuality patterns due to recent surgery. Fear related to treatment and invasive procedures and threat of death.
- 65. Promotive Avoid eating foods with carcinogenic substances that can alter their metabolism. Eat balanced diet. Pursuing a lifestyle that modifies cancer-causing factors. Nursing Intervention Preventive The prevention of ovarian cancer is still under investigation Chemoprevention with a retinoid Oral Contraceptives Dietary Modification and Exercise Pregnancy and Breast Feeding Tubal Ligation Ovary Removal
- 66. Hormone Therapy Progestins Estrogens Combination estrogen/progestin therapy Antiestrogens Androgens Gonadotropin-releasing hormone (GnRH) Curative Rehabilitative Continuous follow-up is essential for all ovarian cancer patients.. Most patients are examined by their physicians every 3 months for the first 2 years. During each visit, the physician will check the CA125 level in the patient's blood. Sexual Concerns -the surgery that is performed to treat ovarian cancer will result in sexual changes Menopausal symptoms can be treated hormonally psychological and/or sexual counseling.
- 67. L eiomyomas Also called uterine fibroids, uterine leiomyomas or uterine leiomyomata. They are many times denser than normal myometrium. Uterine fibroids are usually round or semi-round in shape Locations Intramural fibroid tumors Subserous fibroid tumors Submucous fibroid tumors Ultrasound Transvaginal ultrasound Hysterosalphingography Hysteroscopy CT scan MRI CBC Diagnostic Tests
- 68. More estrogen and progesterone promote the growth of fibroids Develop in smooth muscle tissue in the uterus Single cell reproduces repeatedly Creating a pale, firm, rubbery mass distinct from neighboring tissue Fibroid enlarges in the uterus Uterus expand Vaginal bleeding
- 69. Complications Anemia-from heavy blood loss sudden, sharp, severe pain in lower abdomen distort or block your fallopian tubes interfere with the passage of sperm from cervix to fallopian tubes may prevent implantation and growth of an embryo slightly increased risk of miscarriage premature labor and delivery abnormal fetal position separation of the placenta from the uterine wall Medical Intervention Gonadotropin-releasing hormone (Gn-RH) aganists. Androgens Danzol Oral contraceptives/ progestines Surgical Intervention Hysterectomy Myomectomy – Removal of fibroids Abdominal Myomectomy Laparoscopy Hysteroscopy Myolysis Cryomyolysis Endometrial Alblation Uterine Artery Embolization
- 70. Nursing Assessment Heavy menstrual bleeding Prolonged menstrual periods or bleeding between periods Pelvic pressure or pain Urinary incontinence or frequent urination Constipation Backache or leg pains Pelvic pain that doesn't go away Overly heavy or painful periods Spotting or bleeding between periods Pain with intercourse Difficulty emptying your bladder Difficulty moving your bowels
- 71. NURSING DIAGNOSES Acute pain resulting from medical problem Constipation related to tumor. Deficient knowledge related to new condition Urinary retention due to disease process Disturbed body image related to permanent alteration in function of a body part Nursing Intervention Promotive Avoid eating foods with carcinogenic substances that can alter their metabolism. Eat balanced diet. Pursuing a lifestyle that modifies cancer-causing factors Preventive Chemoprevention with a retinoid Dietary Modification and Exercise Pregnancy and Breast Feeding Tubal Ligation Ovary Removal
- 72. Curative Hysterectomy Myomectomy – Removal of fibroids Abdominal Myomectomy Laparoscopy Hysteroscopy Myolysis Cryomyolysis Endometrial Alblation Uterine Artery Embolization Gonadotropin-releasing hormone (Gn-RH) aganists. Androgens Danzol Oral contraceptives/ progestines Rehabilitative Continuous follow-up is essential for all ovarian cancer patients.. Most patients are examined by their physicians every 3 months for the first 2 years. During each visit, the physician will check the CA125 level in the patient's blood. Sexual Concerns -the surgery that is performed to treat ovarian cancer will result in sexual changes Menopausal symptoms can be treated hormonally psychological and/or sexual counseling.
- 73. Huether, Mc Cance Understanding Pathophysiology 2004 3 rd ed pp. 850-922 Gulanick & Meyer Nursing Care Plans 2007 3 rd ed pp. 15, 21, 51, 116, 126 136 Lemone & Burke Medical Surgical Nursing 2004 3 rd ed Vol. 2 pp. 1531-1532, 1543-1549 References: http:// en.wikipedia.org/wiki/Cryptorchidism http:// emedicine.medscape.com/article/hydrocele http:// children.webmd.com/tc/hypospadias -topic-overview wiki.bmezine.com/index.php/Hypospadia http://www.mayoclinic.com/health/prostate-cancer/DS00043 http:// www.mayoclinic.com /health/uterine-fibroids http:// en.wikipedia.org/wiki/Varicocele Luckmann & Sorensen Medical Surgical Nursing 3 rd ed Vol. 2 pp. 1720-1722, 1745, 1801-1803, Smeltzer & Bare Medical Surgical Nursing 9 th ed Vol. 2 pp. 1241-1308 Smeltzer, Bare, Cheever Textbook of Medical-Surgical Nursing pp. 1996 1679, 1689-1696
- 74. P repared by: Allado, Molena Benemile, Diane Claire Datiles, Kris Angela Mosquera, Ruby Jane Pagdilao, Adonis Jess Tentativa, Jaritza Yosefa GROUP 5 BSN III-Fenwick
- 76. Female
- 77. Male