Schizophrenia ppt
- 1. SCHIZOPHRENIAS A group of common major psychoses with a complex syndromal presentation, affecting young adults, showing chronic changes in behavior, perception, thoughts and emotions, causing a fundamental disorganization in personality and deterioration from previous levels of functioning
- 2. Epidemiology It is a universal disease found in all countries and all times with constant prevalence rates Incidence – 15-20/ 100,000/year Prevalence – 0.5 – 1% Normal risk (life time) – 0.7 – 1.3% (1%)
- 3. Exceptions to Universal Epidemiology Some communities have high incidence Northern Sweden, Western Ireland, Catholics in Canada, Tamils of South India and Sri Lanka In Northern Sri Lanka 34.6 / 100,000 / yr* Some communities have low incidence Hutterites, Anabaptist section of United States *Somasundaram D.J., Yoganathan S. & Ganeshvaran T. (1993) Schizophrenia in Northern Sri Lanka, Ceylon Medical Journal, 38, 131- 135.
- 4. Epidemiology ctd.. Age – 15 -45 years Sex – Male : Female 1 : 1 Onset is earlier in men
- 5. Aetiology- Multifactorial Variable Phenotypic Expression Hereditary 40% of the Pts have a family history In Jaffna – 63 % Relationship Likelihood of dev. Sch. Both parents 46% One parent 15% One sibling 10 – 14% MZ twin 42% DZ twin 10 – 14% 2nd degree relatives 2 -3 % Not related 1% Genetic Markers- Molecular Genetics: COMT gene
- 6. Environmental factors Family Disorders in relationship and communication Emotional family, Double bind messages, dominant mother High Expressed Emotion (EE) - hostility - critical - over involvement
- 7. Viral infection - In utero influenza like virus Birth trauma - hypoxia, cerebral injuries Endocrine Factors Postpartum psychosis Later onset in females Stress Psychological – life events, trauma, migration Physical – Viral encephalitis, Pyrexia, anti-malarials, surgery
- 8. Sensory loss / deprivation Head injury Epilepsy Drugs – amphetamines, L dopa, cannabis Multisystem CT disorders Socio – cultural low socioeconomic state, urban (homeless, prostitutes, prisons) single, unemployed ?cause or ‘drift’
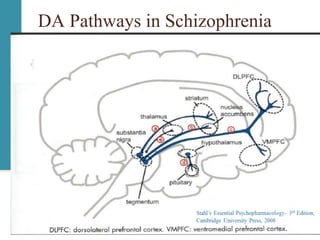
- 9. Neurotransmitters in Schizophrenia Dopamine Hypothesis Dopamine Hyperactivity in Mesolimbic pathways Hypofunction in Mesocortical pathways Glutamate Hypothesis NMDA hypofunction The role of Serotonin Dysfunction in DA release
- 10. DA Pathways in Schizophrenia
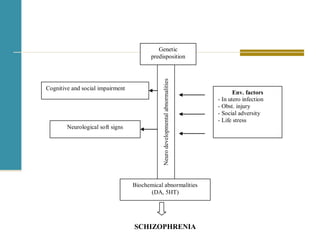
- 12. Neurodevelopmental theory Observations Neuro imaging Neurological soft signs Hypofrontality Neurocognitive and social cognitive impairments- poor functional outcome Hypothesis Pathological changes laid down in early life Non progressive damage
- 13. Cognitive and social impairment Genetic predisposition Neurodevelopmentalabnormalities Biochemical abnormalities (DA, 5HT) Env. factors - In utero infection - Obst. injury - Social adversity - Life stress Neurological soft signs SCHIZOPHRENIA
- 14. Symptoms of Schizophrnia Positive Symptoms Hallucinations Delusions Passivity Negative symptoms Apathy Amotivation / Avolition Asocialization Disorganization Thoughts Emotions
- 15. The Puzzle of Schizophrenia
- 20. Diagnosis of Schizophrenia Schneider's First rank symptoms Auditory Hallucinations –3rd person, thought echo, commenting voices Thought - insertion, withdrawal, broadcasting Delusional perception Passivity Somatic hallucinations ICD 10 DSM IV
- 21. Differential diagnosis Medical Epilepsy Cerebro vascular disorders Cerebral neoplasms Head injury Infections Encepalitis, AIDS, Systemic infections, Substances Amphetamines, Hallucinogens, alcohol Psychiatric Brief/Reactive psychosis Schiz. Affective dis. Affective disorder Delusional disorder Dissociative conditions Possession PD OCD
- 22. Co-morbidity Depression OCD Anxiety disorders Substance abuse
- 23. Management 1. Pharmacological management 2. Other physical management 3. Psychological management 4. Rehabilitation 5. Family work Biopsychosocial approach
- 24. Pharmacological management Antipsychotics 1. Typical antipsychotics – Chlorpromazine, Trifluoperazine, Haloperidol, Droperidol, Pimozide, 2. Atypical antipsychotics Olanzapine, Risperidone, Quetieapine, Amisulpiride, Ziprasidone, Aripiprazole, Clozapine
- 25. Selection of drugs depends on Availability Side effect profile Symptoms Specific contra indications Familiarity Cost
- 26. Management Initial tranquilization Control of acute psychotic symptoms Resistant Schizophrenia- Clozapine Long term maintenance treatment- depot
- 27. Mental Asylum
- 28. Psychosocial management PsychoEducation Supportive psychotherapy CBT for resistant hallucinations and delusions- Cognitive remediation Social skills training
- 29. Rehabilitation Helps to reintegrate Training in Self care, ADLs Attending skills, Communication skills, Ability to concentrate… Vocational training, working in a supportive environment Helps in the management of Negative symptoms Dealing with resistant symptoms Dependency / institutionalized syndrome
- 30. Rehabilitation – ctd Day care centers / hospitals Half way homes / Supported accommodation Occupational Therapy Vocational training Supportive working environments Home environment
- 33. Family work Psycho education Learning better coping strategies Familiarizing with medications, symptoms, risk assessments and limit settings Dealing with expressed emotions (EE) Need for optimal stimulation Family groups Supportive counselling to the family members
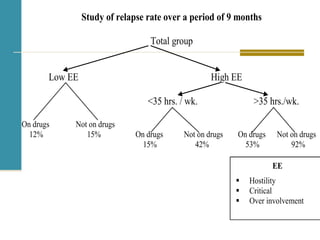
- 34. EE Hostility Critical Over involvement Study of relapse rate over a period of 9 months Total group Low EE High EE <35 hrs. / wk. >35 hrs./wk. On drugs Not on drugs 12% 15% On drugs Not on drugs On drugs Not on drugs 15% 42% 53% 92%
- 35. Community Awareness Reducing stigma Avoiding provoking behaviours Rehabilitation Community Care
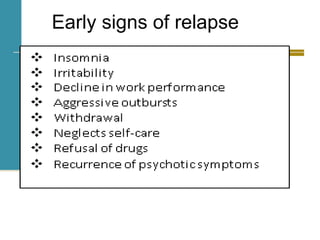
- 36. Early signs of relapse
- 37. Outcome 30% - good recovery with previous level of functioning 30% - good recovery with residual symptoms. able to function socially without help. 30% - handicapped by the illness. getting frequent relapses and exacerbations. need long term, closely supervised care 10% - get worse, suicide
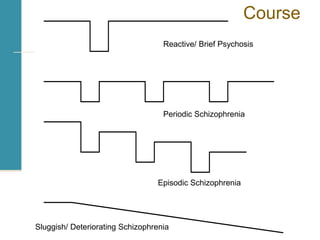
- 38. Reactive/ Brief Psychosis Periodic Schizophrenia Episodic Schizophrenia Sluggish/ Deteriorating Schizophrenia Course
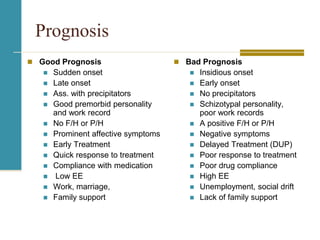
- 39. Prognosis Good Prognosis Sudden onset Late onset Ass. with precipitators Good premorbid personality and work record No F/H or P/H Prominent affective symptoms Early Treatment Quick response to treatment Compliance with medication Low EE Work, marriage, Family support Bad Prognosis Insidious onset Early onset No precipitators Schizotypal personality, poor work records A positive F/H or P/H Negative symptoms Delayed Treatment (DUP) Poor response to treatment Poor drug compliance High EE Unemployment, social drift Lack of family support
Editor's Notes
- Aggressive symptoms such as assaultiveness and verbal abuse frequently occur in association with positive symptoms. Impairment in attention and executive functioning as well as affective symptoms such as loss of interest occur with negative symptoms