Session 5 rieb challenging cases
- 1. Challenging Cases: Treating Pain and Addiction Launette Rieb, MD, MSc, CCFP, FCFP, dip. ABAM Clinical Associate Professor, UBC Director, St. Paul’s Hospital Goldcorp Addiction Medicine Fellowship FME & CPSBC 27th Annual Pain and Suffering Symposium March 7-8, 2014, Vancouver, BC, Canada
- 2. Learning Objectives Participate in group discussion of cases Help generate a differential diagnosis Gain ideas of management strategies for patients with pain and addiction Reflect on your own practice and identify patients that may need a new approach
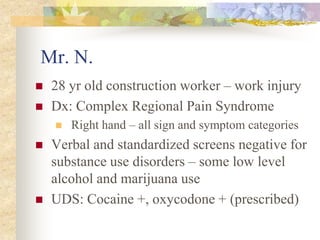
- 3. Mr. N. 28 yr old construction worker – work injury Dx: Complex Regional Pain Syndrome Right hand – all sign and symptom categories Verbal and standardized screens negative for substance use disorders – some low level alcohol and marijuana use UDS: Cocaine +, oxycodone + (prescribed)
- 4. Mr. N, cont’d Broaching the topic: “Your urine drug screen has come back. Do you have any ideas about what it might have shown?” Rapport/honesty + things not on the UDS “It has come back with cocaine. Some people in pain use cocaine. Do you want to tell me about your experience?”
- 5. Mr. N. cont’d “If you are using cocaine I can help you get treatment and help you with your pain” Addiction history came spilling out Years of struggle with alcohol and cocaine – predating injury but worsened by it Totally out of control now, frightened By the end of the conversation – relieved
- 6. Mr. N. cont’d Plan: Residential drug and alcohol Tx 103d Returned drug and alcohol free, off opioids Then a multidisciplinary pain management program could begin PT, OT, Psych, Kin, med management Participated well One binge drinking episode – re-stabilized Good concurrent 12 step involvement
- 7. Mr. N. cont’d Medications blister packed: Gabapentin 1200 mg q8h Amitriptyline 125 mg hs – with a plan to taper Cymbalta 60 mg ii qam Naproxen 500 q 12 h Quetiapine 25 mg bid-tid prn Employer supportive: RTW modified duties Though in pain he felt he could deal with it He felt the treatment he received saved his life
- 8. Mr. N. Reflections What could have happened if I had not done a UDS on assessment? What would you do if he denied cocaine use even once the sample was confirmed? What other techniques do you use to encourage patients to reveal their substance use histories to you? What would you offer if his USD was oxycodone -, opioid+, and cocaine+ ?
- 9. Mr. D. 47 year old married at home father, degree is psychology, no family history of SUD Age 19: L4-5 discectomy for prolapse Post-op give Tylenol #3 He mixed these with ETOH to get high 10 years later – recurrent disc – surgery Initially successful then increasing low back pain over the next year
- 10. Mr. D, con’t GP managed Tried different medications, low dose at 1st Hydromorphone short acting up to 80 mg/d Would run out early, would crush and smoke Prozac 60 mg/d Ativan 4 mg/d Pain still unmanageable on above regime Referred on
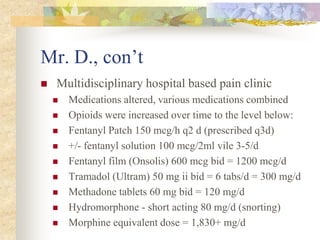
- 11. Mr. D., con’t Multidisciplinary hospital based pain clinic Medications altered, various medications combined Opioids were increased over time to the level below: Fentanyl Patch 150 mcg/h q2 d (prescribed q3d) +/- fentanyl solution 100 mcg/2ml vile 3-5/d Fentanyl film (Onsolis) 600 mcg bid = 1200 mcg/d Tramadol (Ultram) 50 mg ii bid = 6 tabs/d = 300 mg/d Methadone tablets 60 mg bid = 120 mg/d Hydromorphone - short acting 80 mg/d (snorting) Morphine equivalent dose = 1,830+ mg/d
- 12. Mr. D., con’t Other medications Fluoxetine 80 mg/d (adverse rxn - duloxetine) Diazepam 2.5 mg bid (+still using lorazepam) Sudafed 2 tabs/d Caffeine pills and energy drinks He still felt pain, otherwise felt “Great!” Function: ran triathlons, others see sedation Total cost to wife’s insurance = $3,000/wk
- 13. Mr. D., con’t Voluntary admission to a medically supervised residential treatment facility: education, 12 step, group, 1:1, CBT, etc. Methadone and fluoxetine same dose at 1st Stopped tramadol on admission Stopped all fentanyl after 2 d taper Added quetiapine 25 mg q6h No withdrawal seen
- 14. Mr. D., con’t Tapered the methadone over 3 weeks to 5 mg tid Dose held until in withdrawal Switched to Butrans patch 10 mcg initially – not quite enough Then over to Suboxone titrated to 6 mg/d where he has maintained for 8 months
- 15. Mr. D., followup Now 9 months since admission to recovery Current meds Suboxone 6 mg/d Prozac 60 mg/d and tapering Seroquel 125 mg/d and tapering Has attended 12 step daily, has a sponsor No relapses or slips, despite divorcing No more pain issues, GAF 95/100
- 16. Mr. D., Reflections Primary pain disorder or substance use disorder? Opioid induced hyperalgesia? How can the opioids besides methadone be stopped abruptly without withdrawal? How can Suboxone and 12 step combined control both the pain and addiction issues?
- 17. Ms. J. 19 year old street entrenched female youth Pierced, tattooed, black clothes torn Presents asking for methadone Past Medical History Severe ankle sprain a year prior, air cast Initial x-ray negative Ongoing pain, ER visits – “drug seeking” Friends helped out with pills then heroin No mood issues, sleep broken
- 18. Ms. J., cont’d Medications Ibuprofen 400mg 1-2 prn Acetaminophen ineffective Substance Use History Tobacco started age 12, currently 1ppd Marijuana started age 13, currently 2-3 jnts/d Alcohol started age 13, 2 beer/wk, rare binges Heroin – started 6 months prior with smoked heroin escalating to ¾ gm/d iv divided tid
- 19. Ms. J., cont’d Social history On the street since age 17 Father alcoholic, violent, she left home Recent breakup with boyfriend Has a dog which makes housing a challenge Exam – bony tenderness right ankle What are the next steps?
- 20. Ms. J., cont’d Management Converted to methadone 85 mg/d Referred to community counselor for housing X-ray, CT, bone scan – occult fracture and low grade osteomyelitis Antibiotics Surgical intervention – internal fixation Temporary oxycodone for several weeks following surgery
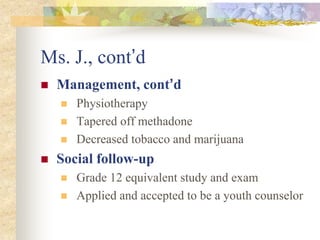
- 21. Ms. J., cont’d Management, cont’d Physiotherapy Tapered off methadone Decreased tobacco and marijuana Social follow-up Grade 12 equivalent study and exam Applied and accepted to be a youth counselor
- 22. Ms. J., Case Highlights What can begin as pseudo-addiction (seeking pain relief but labeled as drug seeking) can become full blown addiction People who fall outside the average (due to class, race, sexual orientation, body ornamentation, age, lifestyle, etc.) can be misdiagnosed or not fully seen Treat the underlying condition Challenge yourself to see whole the person
- 23. Ms. J, Reflections How would your management change if her investigations had been negative? What if she was in an abusive relationship where she was being assaulted? What if her pain was unbearable even on methadone?
- 24. Mr. L. 44 year old man presented in 2004 Heroin 2 – 3 gm/d for many years Detoxed in the past but craving > relapse Hepatitis C positive Mild to moderate OA knees Converted to methadone 210 mg/d Stable for 2 years, urine drug screens clear
- 25. Mr. L., cont’d 2006 he decides to sells condo and travel Voluntary rapid taper from methadone Relapses in Europe due to exposure Returns and re-stabilized on methadone Another rapid taper (10 mg/d) for travel Getting some knee pain at end of taper Declines NSAIDS, acetaminophen
- 26. Mr. L., cont’d Oxycodone 5 mg bid controlled pain Leaves for China 2008 re-appears after hospitalization for endocarditis secondary to intravenous use Attending a residential “detox”, given… Methadone 100 mg/d (daily dispensed) Oxycodone (IR) 20 mg iii tid = 180 mg/d Diazepam 10 mg bid - tid prn (weekly disp.)
- 27. Mr. L., cont’d Patient reports knee pain very high He curtails walking, and is not attending physiotherapy, nor swimming He looks sedated in the office, but he claims it is due to poor sleep from pain What could be going on? Next steps?
- 28. Mr. L., cont’d Changed to long acting oxycodone 80mg tid Patient reports it doesn’t work – wants IR Tapered off diazepam Daily dispensed all medication, witnessed 1st dose, upset at being “treated like a child” Pain reported to be worse, less function What next?
- 29. Mr. L., cont’d Offered TCAs, NSAIDS, atypical anti- psychotics, SNRIs, neuromodulators, etc. All declined for various reasons, including HCV Physiotherapy prescribed, pool pass, not used Orthopaedic surgeon reviews – offers bilateral knee replacements, patient declines Hepatologist contacted Ok to take acetaminophen up to 1500 mg/d Ok to take NSAIDs like ibuprofen full strength Patient declines
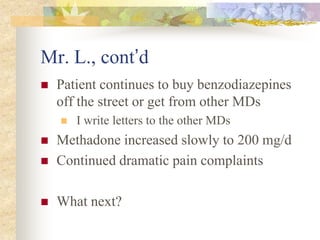
- 30. Mr. L., cont’d Patient continues to buy benzodiazepines off the street or get from other MDs I write letters to the other MDs Methadone increased slowly to 200 mg/d Continued dramatic pain complaints What next?
- 31. Mr. L., cont’d Considering OIPS and OD risk… Oxycodone tapered to elimination (involuntary – not happy) Methadone increased to 260 mg/d Once completed… Pt less sedated, reports lower pain, attends physio with some positive results, goes to UBC for continuing education classes
- 32. Mr. L., cont’d Then he starts to report more pain Pt has clear UDS so we can split his methadone dose (q8h), makes no difference Patient wants oxycodone and diazepam He gets an advocate to protect his rights Claims I refuse to treat his pain What next?
- 33. Mr. L., cont’d Pt. says he wants tapered off methadone December 2009 the pharmacist calls to say he saw Mr. L. hand his methadone to another person who drank it. Mr. L. called in for discussion – and he says he hasn’t been taking his methadone – he sometimes “shares” it with a friend. Admits to selling oxycodone previously.
- 34. Mr. L., cont’d All methadone prescribing stops and a letter is given to him about why He presents angry, threatening to report me to CPSBC, shows me a letter to this effect Care transferred to colleague (same clinic) Letter written to Mr. L. outlining options Soon colleague must discharge him too. Observations or questions?
- 35. Mr. X 48 y.o. male iron worker injured 2002 Fall, R knee: torn cartilage, meniscus, ACL with OR Knee gives way leading to other falls Pain with any movement Wakes at night moaning in pain Not working, limited household chores
- 36. Mr. X, cont’d Past Medical History Low back injuries ++ ongoing pain, Tyl #4 # elbow, torn rot. cuff, # pelvis, # ribs, #leg Asthma Motorcycle accident killing 1st wife Depressed mood, anxiety, abuse issues Cluster headaches
- 37. Mr. X, cont’d Medications Salbutamol 2 puffs prn Topiramate 25 mg q6h (for cluster h/a) Buproprion 150 mg bid (for mood) Diazepam 10 mg 1-2 hs prn (for sleep) Meperidine 50 mg 2 q4h (tapered to 1 q6h) Tylenol #4 2 q4h prn (tapered to 1 q6h)w/d
- 38. Mr. X, cont’d Substance Use History Caffeine - 1 cup per d Nicotine - 1ppd since age 15, stopped along with his spouse 5 yrs ago Marijuana - None (gets paranoid)
- 39. Mr. X, cont’d Social drinking age 22-40s Escalated at 24 when wife killed Stopped briefly once spouse returned Back up to scotch 26 oz per day with tolerance, loss of control, compulsion, preoccupation, personality changes, anxiety only w/d symp. (spouse drinks wine) Alcohol
- 40. Mr. X, cont’d Tyl #4 for 7 yrs for back pain After knee injury T#4 - 4 q4h Morphine tablets initially, off now Meperidine 50 mg “chewing them like candy” Hiding pills from wife, running out early One heroin use (guilt, biker stigma) Opioids
- 41. Mr. X, cont’d “Recreational use” from 20s-40s “Problem” after 1st wife killed after a divorce and post knee injury 2002-03: cocaine 1-2 gm IV every 1-2 d Paranoid, $ problems, tolerance, loss of control, depression, use despite consequences. Stopped after wife left. Cocaine
- 42. M. X, cont’d Speed (amphetamines) Used in his 20s to stay alert on long motorcycle road trips. Last use 20 yrs ago. No other street drug or herbal remedy use
- 43. Mr. X, cont’d Diagnosis Chronic knee and low back pain Substance dependence: alcohol, cocaine, opioid, nicotine in remission Depression in partial remission Recommendations At home taper and stop ETOH, family MD informed, if problems then residential detox In Pain Management Program (PMP) taper meperidine, codeine and benzodiazepines
- 44. Mr. X – Follow Up Self tapered ETOH, diazepam & meperidine at home prior to PMP During PMP he fell and # ribs, wrenched knee again, delays in taper of codeine Almost off codeine with much better function and lowered pain by end of PMP Sharing international award winning poetry He and spouse happy with achievements
- 45. Mr. X - Reflections Opioid induced pain sensitivity? Primary mood induced pain sensitivity? Alcohol induced mood changes…? Or primarily substance use disorder driven on intake by alcohol dependence, which once treated regulated all other responses. Your thoughts?
- 46. Your Cases Do you have any examples of a patient with past dependence that was at high risk of relapse until the pain got under control? Other cases from your practice you’d like the group’s input on?
- 47. Summary Develop a differential diagnosis Special considerations need to be applied to those with present or past addiction Analgesic control is needed to prevent relapse to substance dependence in those with past addiction Substance dependence can develop when exposed to severe untreated pain – see the whole person Active substance dependence needs addressing in order to then get pain under control You can be compassionate and set clear parameters for care to benefit all!
- 48. Good Resource
- 49. Resources Butler D and Moseley G L. Explain Pain. Noigroup Publications, Adelaide, Australia (2003) Moseley G L. Painful Yarns. Dancing Giraffe Press (2007) See references in my plenary talk