Stroke pt management
- 2. ACUTE STAGE Positioning strategies Improving respiratory and circulatory function Prevent pressure sores Prevent from deconditioning
- 3. POSITIONING STRATEGIES In supine In side lying on normal side In side lying affected side Sitting
- 4. IMPROVE RESPIRATORY AND CIRCULATORY FUNCTION Breathing exercise Chest expansion exercise Postural drainage Huffing and coughing techniques Passive and active ankle & toe exercise ( after careful assessment)
- 5. PREVENT PRESSURE SORES Proper positioning Relieve pressure points by padding and cushion Frequent turning and changing position Prevent from moisture Use cotton clothing Tight fitting cloth is prevented Use of water bed, air bed & foam mattress
- 6. PREVENT FROM DECONDITIONING Early mobilization in the bed (active turning, supine to sit, sit to supine, sitting, sit to stand) Pelvic bridging exercise Early propped up positioning, sitting & then later to standing Moving around the bed Facilitate movement of functioning limbs
- 7. PT INTERVENTIONS Improve sensory function Flexibility& Joint integrity Improve strength Manage spasticity Improve Movement control Postural control & Functional Mobility Improve Function Managing shoulder pain Improve LL function Improve balance Improve locomotion Improve aerobic function Improve feeding and swallowing Improve motor learning Patient and family education
- 8. Improve sensory function Positioning hemiplegic side towards door or main part of room Presentation of repeated sensory stimuli Stretching, stroking, superficial & deep pressure, icing, vibration Wt. bearing ex & Join approximation technique Stoking with different texture fabrics Pressure application Improve other senses like use of visual & auditory PNF technique, use of bilateral UE
- 9. Flexibility & Joint Integrity Soft tissue, Joint mobilization & ROM exercise AROM & PROM with end range stretch Effective positioning & edema reduction Streching program & splinting Suggested activities Arm cradling Table top polishing Self overhead activities in supine & sitting & reaching to the floor
- 10. Improve strength Strengthening of agonist & antagonistic muscle Graded exercise program using free weights, Thera bands, sand bags & isokinetic devices For weak patients (<3/5), gravity eliminated exercise using power boards, sling suspension or aquatic exercise is indicated Gravity-resisted active movements are indicated (>3/5 strength)
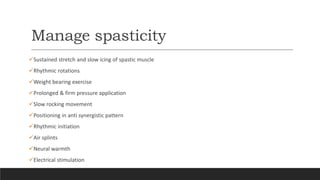
- 11. Manage spasticity Sustained stretch and slow icing of spastic muscle Rhythmic rotations Weight bearing exercise Prolonged & firm pressure application Slow rocking movement Positioning in anti synergistic pattern Rhythmic initiation Air splints Neural warmth Electrical stimulation
- 12. Improve Movement control Dissociation & selection of desired movement Select postures that assist desired movements through optimal biomechanical stabilization & use of optimal point in range Start with assisted movement, followed by active & resisted movement Task oriented exercise
- 13. Postural control & functional mobility Suggested exercise Rolling Supine to sit and sit to supine Sitting Bridging Sit to stand & sit down Modified plantigrade Standing Transfer
- 14. In pusher syndrome Passive correction often fails Use visual stimuli to correct Sit on the normal side & ask patient to lean on you Sitting on Swiss ball Environmental boundary can be used e.g. corner or doorway
- 15. Improve UE function Early mobilization, ROM & positioning strategies Relearning of movement pattern & retraining of missing component UL weight bearing exercises Dynamic stabilization exercise Picking up objects, Reaching activities Lifting activities Manipulation of common objects Push up ex. In various position Kitchen sink exercise Functional movement like hand to mouth & hand to opposite shoulder Advance training-CIMT, biofeedback , NMES ,FES
- 16. Managing shoulder pain Proper handling & positioning of shoulder joint Reducing subluxation, NMES, gentle mobilization( grade 1& 2) Use of supportive devices & slings Use of overhead pulley is contraindicated TENS & Heat therapy
- 17. Improving LL function Strengthening muscles in appropriate manner Suggested activities –PNF pattern of LL -Holding against elastic band resistance around upper thighs in supine or standing positions -Standing, lateral side steps -Exercise to improve pelvic control Facilitation of DF Cycling or treadmill training
- 18. Improve balance Facilitate symmetrical weight bearing on both side Postural perturbations can be induced in different positions Sit or stand on movable surface to increase challenge Reaching activities Dual task training e.g. Carrying object while walking Divert attention Single limb stance Exercise on trampoline
- 19. Improve locomotion Initial gait training between parallel bars Proceed outside bars with aids and then walking without aids Walking forward, backward, sideways & in cross patterns PBWSTT with higher speed improve overall locomotor activity & overground speed Proper use of orthotics & wheelchair
- 20. Improve aerobic function Early mobilization & functional activity Treadmill training & cycling ergometer Symptom limited graded exercise training Exercise at 40-70% of VO2max, 3 times a week for 20-60 minutes Proper rest should be given Gradually progressed to 30 minutes continuous program Regular exercise reduces risk of recurrent stroke
- 21. Improve feeding & swallowing Proper head position in chin down position Movements of lips, tongue, cheeks & jaw Firm pressure to anterior 3rd of tongue with tongue depressor to stimulate posterior elevation of tongue Puffing, blowing bubbles & drinking thick liquids through straw Food presentation in proper position Texture of food should be smooth Tasty food should be given to facilitate swallowing reflex Stroking the neck during swallowing
- 22. Improve motor learning Strategy development- patient as an active explorer of activity - Modify strategy of activity in correct posture Feedback- Intrinsic and extrinsic feedback, Positive and negative feedback Practice- Repeated practice of functional activity, Practice in different environment
- 23. Patient & family education Give information, counsel family members about patient’s capabilities & limitations Give information as much as Patient or family can assimilate Provide open discussion & communication Be supportive, sensitive & maintain a positive supporting nature Give psychological support Refer to help groups