Typhoid fever ppt.
- 1. TYPHOID FEVER Sapana thakor m.sc nursing Community health nursing
- 2. The term enteric fever or typhoid fever is a communicable disease, found only in man and includes both typhoid fever caused by S.Typhi and paratyphoid fever caused by S.Paratyphi A, B and C . It is an acute generalized infection of the reticulo endothelial system, intestinal lymphoid tissue, and the gall bladder.
- 3. EPIDEMIOLOGY
- 6. • HOST • Age group : Typhoid fever may occur at any age but it is considered to be a disease mainly of children and young adults. In endemic areas, the highest attack rate occurs in children aged 8-13 years.
- 7. Gender and race : Typhoid fever cases are more commonly seen in males than in females. On the contrary, females have a special predilection to become chronic carriers. Occupation : Certain categories of persons handling the infective material and live cultures of S. typhi are at increased risk of acquiring infection. Socio-economic factors : It is a disease of poverty as it is often associated with inadequate sanitation facilities and unsafe water supplies.
- 8. • Environmental factors : Though the cases are observed through out the year, the peak incidence of typhoid fever is reported during July - September. This period coincides with the rainy season and a substantial increase in fly population. • Social factors : pollution of drinking water supplies, open air defecation, and urination, low standards of food and personal hygiene, and health ignorance.
- 9. Nutritional status :Malnutrition may enhance the susceptibility to typhoid fever by altering the intestinal flora or other host defences. Incubation period : Usually 10-14 days but it may be as short as 3 days or as long as 21 days depending upon the dose of the inoculums. Reservoir of infection : Man is the only known reservoir of infection - cases or carriers. Period of communicability: A case is infectious as long as the bacilli appear in stool or urine.
- 10. Mode of transmission : The disease is transmitted by faeco - oral route or urine – oral routes – either directly through hands soiled with faeces or urine of cases or carriers or indirectly by ingestion of contaminated water, milk, food, or through flies. Contaminated ice, ice-creams, and milk products are a rich source of infection.
- 11. Symptoms ■ No symptoms - if only a mild exposure; some people become "carriers" of typhoid. ■ Poor appetite, ■ Headaches, ■ Generalized aches and pains, ■ Fever, Lethargy, Lethargy, ■ Lethargy, ■ Diarrhea, ■ Have a sustained fever as high as 103 to 104 degrees Fahrenheit (39 to 40 degrees Celsius), ■ Chest congestion develops in many patients, and abdominal pain and discomfort are common, ■ Constipation, mild vomiting, slow heartbeat.
- 12. • First week: The disease classically presents with step-ladder fashion rise in temperature (40 - 41°C) over 4 to 5 days, accompanied by headache, vague abdominal pain, and constipation. • Second week: Between the 7 th -10 th day of illness, mild hepato- splenomegally occurs in majority of patients. Relative bradycardia may occur and rose-spots may be seen. • Third week: The patient will appear in the "typhoid state" which is a state of prolonged apathy, toxaemia, delirium, disorientation and/or coma. Diarrhoea will then become apparent. If left untreated by this time, there is a high risk (5-10%) of intestinal hemorrhage and perforation. • Rare complications: Typhoid hepatitis,Emphyema, Osteomyelitis, and Psychosis. 2-5% patients may become Gall-bladder carriers
- 13. Rose spots
- 15. Diagnosis Diagnosis of typhoid fever is made by ■ Blood, bone marrow, or stool cultures test ■ Widal test ■ Slide agglutination ■ Antimicrobial susceptibility testing
- 16. Management of typhoid fever: • General: Supportive care includes • Maintenance of adequate hydration. • Antipyretics. • Appropriate nutrition. • Specific: Antimicrobial therapy is the mainstay treatment. Selection of antibiotic should be based on its efficacy, availability and cost. • Chloramphenicol , Ampicillin ,Amoxicillin , Trimethoprim &Sulphamethoxazole ,Fluroquinolones • In case of quinolone resistance – Azithromycin, 3rd generation cephalosporins (ceftriaxone)
- 17. Control of Typhoid fever MEASURES DIRECTED TO RESERVOIR a) Case detection and treatment b) Isolation c)Disinfection of stools and urine d)Detection & treatment of carriers MEASURES AT ROUTES OF TRANSMISSION a) Water sanitation b) Food sanitation c) Excreta disposal d) Fly control MEASURES FOR SUSCEPTIBLES a) immunoprophylaxis b)health education
- 18. • Keep the premises and kitchen utensils clean. • Dispose rubbish properly. • Keep hands clean and fingernails trimmed. • Wash hands properly with soap and water before eating or handling food, and after toilet or changing diapers. • Drinking water should be from the mains and preferably boiled. • Purchase fresh food from reliable sources. Do not patronize illegal hawkers. • Avoid high-risk food like shellfish, raw food or semi-cooked food. • Wear clean washable aprons and caps during food preparation. • Clean and wash food thoroughly. • Scrub and rinse shellfish in clean water. Immerse them in clean water for sometime to allow self-purification. • Remove the viscera if appropriate HEALTH PROMOTION
- 19. • Store perishable food in refrigerator, well covered. • Handle and store raw and cooked food especially seafood separately (upper compartment of the refrigerator for cooked food and lower compartment for raw food) to avoid cross contamination. • Clean and defrost refrigerator regularly and keep the temperature at or below 4ºc • Cook food thoroughly. • Do not handle cooked food with bare hands; wear gloves if necessary. • Consume food as soon as it is done. • If necessary, refrigerate cooked leftover food and consume as soon as possible. Reheat thoroughly before consumption. Discard any addled food items. • Exclude typhoid carrier from handling food and from providing care to children.
- 20. Specific protection THREE TYPES OF VACCINES 1. Injectable Typhoid vaccine (TYPHIM –Vi,TYPHIVAX) 2. The live oral vaccine (TYPHORAL) 3. TAB vaccine
- 21. Injectable Typhim -Vi 1. This single-dose injectable typhoid vaccine, from the bacterial capsule of S. typhi strain of Ty21a. 2. This vaccine is recommended for use in children over 2 years of age. 3. Sub-cutaneous or intramuscular injection 4. Efficacy : 64% -72%
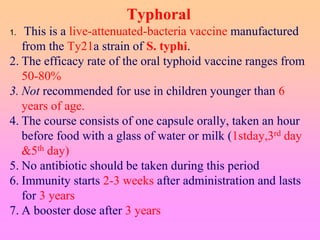
- 22. Typhoral 1. This is a live-attenuated-bacteria vaccine manufactured from the Ty21a strain of S. typhi. 2. The efficacy rate of the oral typhoid vaccine ranges from 50-80% 3. Not recommended for use in children younger than 6 years of age. 4. The course consists of one capsule orally, taken an hour before food with a glass of water or milk (1stday,3rd day &5th day) 5. No antibiotic should be taken during this period 6. Immunity starts 2-3 weeks after administration and lasts for 3 years 7. A booster dose after 3 years
- 23. International Classification of Disease Codes for Typhoid fever Disease ICD-9 ICD-10 Typhoid & paratyphoid fevers 002 A01 Typhoid fever 002.0 A01.0
- 24. THANK YOU