UNIT 4-WPS Office.pptx
- 2. • The cardiovascular (cardio – heart, vascular – blood vessels) system is divided for descriptive purposes into two main parts: the heart, whose pumping action ensures constant circulation of the blood the blood vessels, which form a lengthy network through which the blood flows. • The heart pumps blood into two anatomically separate systems of blood vessels : the pulmonary circulation and the systemic circulation.
- 4. •The right side of the heart pumps blood to the lungs (the pulmonary circulation) where gas exchange occurs, i.e. the blood collects oxygen from the airsacs and excess carbon dioxide diffuses into the airsacs for exhalation. •The left side of the heart pumps blood into the systemic circulation, which supplies the rest of the body. Here, tissue wastes are passed into the blood for excretion, and body cells extract nutrients and O2.
- 5. THE HEART • The heart is a roughly cone-shaped hollow muscular organ. • It is about 10 cm long and is about the size of the owner’s fist. • It weighs about 225 g in women and is heavier in men (about 310 g). • Position The heart lies in the thoracic cavity in the mediastinum (the space between the lungs). • It lies obliquely, a little more to the left than the right, and presents a base above, and an apex below.
- 6. •The apex is about 9 cm to the left of the midline at the level of the 5th intercostal space, i.e. a little below the nipple and slightly nearer the midline. •The base extends to the level of the 2nd rib.
- 8. Organs associated with the heart Inferiorly – the apex rests on the diaphragm. Superiorly – the great blood vessels, i.e. the aorta, superior vena cava, pulmonary artery and pulmonary veins. Posteriorly – the oesophagus, trachea, left and right bronchus, descending aorta, inferior vena cava and thoracic vertebrae. Laterally – the lungs – the left lung overlaps the left side of the heart. Anteriorly – the sternum, ribs and intercostal muscles.
- 10. Structure •The heart wall is composed of three layers of tissue : pericardium, myocardium and endocardium.
- 11. Endocardium •The innermost layer of the cardiac wall is known as the endocardium. It lines the cavities and valves of the heart. •Structurally, the endocardium is comprised of loose connective tissue and simple squamous epithelial tissue – it is similar in its composition to the endothelium which lines the inside of blood vessels. •In addition to lining the inside of the heart, the endocardium also regulates contractions.
- 12. Myocardium •The myocardium is composed of cardiac muscle and is an involuntary striated muscle. The myocardium is responsible for contractions of the heart.
- 13. Pericardium •The epicardium is the outermost layer of the heart, formed by the visceral layer of the pericardium. It is composed of connective tissue and fat. The connective tissue secretes a small amount of lubricating fluid into the pericardial cavity. •In addition to the connective tissue and fat, the epicardium is lined by on its outer surface by simple squamous epithelial cells.
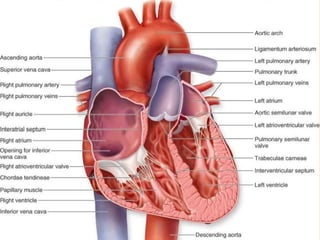
- 14. Interior of the heart Atria : These are the thin-walled receiving chambers of heart. They are separated from each other by inter- auricular septum. Interauricular septum has an oval depression called fossa ovalis. It is a remnant of the embryonic aperture called foramen ovalis.
- 16. Superior vena cava, inferior vena cava and coronary sinus open into the right atrium. Opening of the postcaval is guarded by a Eustachian valve while the Thebesian valve guards the opening of coronary sinus into right atrium. Four pulmonary veins open into the left atrium. These openings are without valves.
- 17. Both the atria open into the ventricles of their respective sides by atrioventricular apertures. These openings are guarded by cuspid valves. The tricuspid valve is present in the right AV aperture and bicuspid valve (mitral valve) is present in the left AV aperture. All these heart valves help in maintaining a unidirectional flow of blood. They also avoid back flow of blood.
- 18. Ventricles : These are inferior, thick-walled pumping chambers of the heart. The right and left ventricles are separated by an interventricular septum. Wall of the left ventricle is more muscular and about 3-times thicker than the right ventricle. Inner surface of the ventricles shows several ridges called columnae carnae or trabeculae carnae which divide the lumen of ventricle into small pockets or fissures.
- 19. •The lumen of ventricles also shows inelastic fibers called chordae tendinae. These attach the bicuspid and tricuspid valves to the ventricular wall (papillary muscles) and regulate their opening and closing. •The right ventricle opens into the pulmonary aorta and left ventricle opens into the aorta. These openings are guarded by three semilunar valves each. These valves prevent the backward flow of blood into the ventricles.
- 20. Flow of blood through heart
- 21. •The two largest veins of the body, the superior and inferior venae cavae, empty their contents into the right atrium. •This blood passes via the right atrioventricular valve into the right ventricle, and from there is pumped into the pulmonary artery or trunk (the only artery in the body which carries deoxygenated blood). •The opening of the pulmonary artery is guarded by the pulmonary valve, formed by three semilunar cusps.
- 22. •This valve prevents the backflow of blood into the right ventricle when the ventricular muscle relaxes. After leaving the heart the pulmonary artery divides into left and right pulmonary arteries, which carry the venous blood to the lungs where exchange of gases takes place: carbon dioxide is excreted and oxygen is absorbed.
- 23. •Two pulmonary veins from each lung carry oxygenated blood back to the left atrium. •Blood then passes through the left atrioventricular valve into the left ventricle, and from there it is pumped into the aorta, the first artery of the general circulation. •The opening of the aorta is guarded by the aortic valve, formed by three semilunar cusps.
- 25. •From this sequence of events it can be seen that the blood passes from the right to the left side of the heart via the lungs, or pulmonary circulation. •However, it should be noted that both atria contract at the same time and this is followed by the simultaneous contraction of both ventricles.
- 26. Blood supply to the heart (the coronary circulation) •Arterial supply The heart is supplied with arterial blood by the right and left coronary arteries, which branch from the aorta immediately distal to the aortic valve. •The coronary arteries receive about 5% of the blood pumped from the heart, although the heart comprises a small proportion of body weight. •This large blood supply, especially to the left ventricle.
- 28. •The coronary arteries traverse the heart, eventually forming a vast network of capillaries. •Venous drainage Most of the venous blood is collected into a number of cardiac veins that join to form the coronary sinus, which opens into the right atrium. The remainder passes directly into the heart chambers through little venous channels.
- 29. Conducting system of the heart •The heart possesses the property of autorhythmicity, which means it generates its own electrical impulses and beats independently of nervous or hormonal control, i.e. it is not reliant on external mechanisms to initiate each heartbeat.
- 30. •However, it is supplied with both sympathetic and parasympathetic autonomic nerve fibres, which increase and decrease respectively the intrinsic heart rate. •In addition, the heart responds to a number of circulating hormones, including adrenaline (epinephrine) and thyroxine.
- 31. •Small groups of specialised neuromuscular cells in the myocardium initiate and conduct impulses, causing coordinated and synchronised contraction of the heart muscle •This pathway is made up of 5 elements: •The sino-atrial (SA) node •The atrio-ventricular (AV) node •The bundle of His •The left and right bundle branches •The Purkinje fibres
- 33. •Sinoatrial node (SA node) • This small mass of specialised cells lies in the wall of the right atrium near the opening of the superior vena cava. The sinoatrial cells generate these regular impulses because they are electrically unstable. •This instability leads them to discharge (depolarise) regularly, usually between 60 and 80 times a minute.
- 34. •This depolarisation is followed by recovery (repolarisation), but almost immediately their instability leads them to discharge again, setting the heart rate. •Because the SA node discharges faster than any other part of the heart, it normally sets the heart rate and is called the pacemaker of the heart. •Firing of the SA node triggers atrial contraction.
- 35. •Atrioventricular node (AV node) This small mass of neuromuscular tissue is situated in the wall of the atrial septum near the atrioventricular valves. •Normally, the AV node merely transmits the electrical signals from the atria into the ventricles. •There is a delay here; the electrical signal takes 0.1 of a second to pass through into the ventricles.
- 36. •This allows the atria to finish contracting before the ventricles start. •The AV node also has a secondary pacemaker function and takes over this role if there is a problem with the SA node itself, or with the transmission of impulses from the atria. •Its intrinsic firing rate, however, is slower than that set by the SA node (40–60 bpm).
- 37. •Atrioventricular bundle (AV bundle or bundle of His) This is a mass of specialised fibres that originate from the AV node. •The AV bundle crosses the fibrous ring that separates atria and ventricles then, at the upper end of the ventricular septum, it divides into right and left bundle branches. •Within the ventricular myocardium the branches break up into fine fibres, called
- 38. •The AV bundle, bundle branches and Purkinje fibres transmit electrical impulses from the AV node to the apex of the myocardium where the wave of ventricular contraction begins, then sweeps upwards and outwards, pumping blood into the pulmonary artery and the aorta.
- 39. Nerve supply to the heart •The heart is influenced by autonomic (sympathetic and parasympathetic) nerves originating in the cardiovascular centre in the medulla oblongata. •The vagus nerves (parasympathetic) supply mainly the SA and AV nodes and atrial muscle. •The sympathetic nerves supply the SA and AV nodes and the myocardium of atria and ventricles.
- 40. The cardiac cycle • At rest, the healthy adult heart is likely to beat at a rate of 60–80 bpm. During each heartbeat, or cardiac cycle, the heart contracts and then relaxes. The period of contraction is called systole and that of relaxation, diastole.
- 42. •Stages of the cardiac cycle •Taking 74 bpm as an example, each cycle lasts about 0.8 of a second and consists of •1) atrial systole – contraction of the atria • 2)ventricular systole – contraction of the ventricles •3)complete cardiac diastole – relaxation of the atria and ventricles.
- 43. •The superior vena cava and the inferior vena cava transport deoxygenated blood into the right atrium at the same time as the four pulmonary veins bring oxygenated blood into the left atrium. The atrioventricular valves are open and blood flows passively through to the ventricles. The SA node triggers a wave of contraction that spreads over the myocardium of both atria, emptying the atria and completing ventricular filling (atrial systole 0.1 s).
- 44. • After this brief delay, the AV node triggers its own electrical impulse, which quickly spreads to the ventricular muscle via the AV bundle, the bundle branches and Purkinje fibres. This results in a wave of contraction which sweeps upwards from the apex of the heart and across the walls of both ventricles pumping the blood into the pulmonary artery and the aorta (ventricular systole 0.3 s).
- 45. •The high pressure generated during ventricular contraction is greater than that in the aorta and forces the atrioventricular valves to close, preventing backflow of blood into the atria. •After contraction of the ventricles there is complete cardiac diastole, a period of 0.4 seconds, when atria and ventricles are relaxed. During this time the myocardium recovers in preparation for the next heartbeat, and the atria refill in preparation for the next cycle.
- 46. Heart sounds • There are two heart sounds, each corresponding to a particular event in the cardiac cycle. The sound through the stethoscope like “lub dup”. The first sound, ‘lub’, is fairly loud and is due to the closure of the atrioventricular valves. This corresponds with the start of ventricular systole. The second sound, ‘dup’, is softer and is due to the closure of the aortic and pulmonary valves. This corresponds with ventricular diastole.
- 48. BLOOD PRESSURE •Blood pressure is the force or pressure that the blood exerts on the walls of the blood vessels. •Systemic arterial blood pressure maintains the essential flow of blood into and out of the organs of the body.
- 49. •The arterial blood pressure, is the result of the discharge of blood from the left ventricle into the already full aorta. •Blood pressure varies according to the time of day, the posture, gender and age of the individual. Blood pressure falls at rest and during sleep.
- 50. sphygmomanometer
- 51. •Systolic and diastolic pressure When the left ventricle contracts and pushes blood into the aorta, the pressure produced within the arterial system is called the systolic blood pressure. • In adults it is about 120 mmHg. •When complete cardiac diastole occurs and the heart is resting following the ejection of blood, the pressure within the arteries is much lower and is called diastolic blood pressure. • In an adult this is about 80 mmHg.
- 52. •The difference between systolic and diastolic blood pressures is the pulse pressure. •Arterial blood pressure is measured with a sphygmomanometer and is usually expressed with the systolic pressure written above the diastolic pressure: •The normal blood pressure- 120/80 mmHg.
- 53. PULSE • Pulse is felt by slightly compressing an artery against an underlying bone or flat muscle by the three middle fingers. • It is felt in the radial, brachial, carotids, femoral and dorsalis pedis arteries. • The subject should be seated comfortably or lying supine. • The radial pulse is best felt with the subject's forearm in mid prone position and wrist slightly flexed. • The following observations are made:
- 54. • Rate: The rate is expressed as beats per minute. The counting is started when the subjects pulse has settled down after an initial quickened due to nervousness. The beats should be counted for at least one minute. The normal resting heart rate is 72 ± 10 beats/min. • Causes of increase in pulse rate: Exercise, anxiety,excitement, fever, thyrotoxicosis, sleep. • Causes of decrease in pulse rate: Regular athletic training, myxedema and sleep. • Rhythm: Normally the pulse beats at regular intervals and therefore is regular. An irregular pulse is seen in disease
- 55. Factors affecting pulse rate are as follows: • Age: ↓with age • Fever: ⬆ with fever • Gender: ⬆ after puberty male slightly <than female • Medications: E.g. ⬆ with epinephrine and with digitalis • Exercise: ⬆ with exercise • Hypovolemia: ⬆ with blood loss • Position changes: Sitting or standing→ pooling of blood in dependent vessels →↓ BP and ⬆ HR • Stress: ⬆ with stress
- 57. BLOOD VESSELS •Blood vessels vary in structure, size and function, and there are several types: arteries, arterioles, capillaries, venules and veins.
- 58. Arteries and arterioles •These are the blood vessels that transport blood away from the heart. They vary considerably in size and their walls consist of three layers of tissue •1)tunica adventitia or outer layer of fibrous tissue •2) tunica media or middle layer of smooth muscle and elastic tissue •3)tunica intima or inner lining of squamous epithelium called endothelium.
- 59. •The amount of muscular and elastic tissue varies in the arteries depending upon their size and function. • In the large arteries, sometimes called elastic arteries, the tunica media consists of more elastic tissue and less smooth muscle. •This allows the vessel wall to stretch, absorbing the pressure wave generated by the heart as it beats.
- 60. •These proportions gradually change as the arteries branch many times and become smaller until in the arterioles (the smallest arteries) the tunica media consists almost entirely of smooth muscle.
- 62. Capillaries •The smallest arterioles break up into a number of minute vessels called capillaries. •Capillary walls consist of a single layer of endothelial cells sitting on a very thin basement membrane, through which water and other small molecules can pass.
- 63. •Blood cells and large molecules such as plasma proteins do not normally pass through capillary walls. •The capillaries form a vast network of tiny vessels that link the smallest arterioles to the smallest venules.
- 64. Veins and venules •Veins are blood vessels that return blood at low pressure to the heart. •The walls of the veins are thinner than those of arteries but have the same three layers of tissue. • They are thinner because there is less muscle and elastic tissue in the tunica media, because veins carry blood at a lower pressure than arteries.
- 65. •veins possess valves, which prevent backflow of blood, ensuring that it flows towards the heart. •They are formed by a fold of tunica intima and strengthened by connective tissue. • The cusps are semilunar in shape with the concavity towards the heart.
- 66. •Valves are abundant in the veins of the limbs, especially the lower limbs where blood must travel a considerable distance against gravity when the individual is standing. •The smallest veins are called venules.
- 68. •Thank you....