Unit III, chapter-1-Body fluids and Blood
- 1. 1 By Mr. Audumbar Mali, Asst. Professor, Sahyadri College of Pharmacy, Methwade Unit-III 1. Body fluids and blood BP101T. Human Anatomy And Physiology-I (Theory)
- 2. 19-2 Body fluids are fluids inside the body of living organisms which serve as a medium for carrying nutrients to and waste products from the cells and a medium for carrying the chemical communicators that coordinate activities among cells. Examples of body fluids are interstitial fluid, blood plasma, urine, lymph, cerebrospinal fluid, aqueous humor, and sensorial fluid. The most abundant is interstitial fluid, which directly surrounds most cells and fills the spaces between them. It makes up about 17% of body weight. Another body fluid is blood plasma, which flows in the arteries and veins. It makes up about 5% of body weight. Other body fluids that occur in lesser amounts are urine, lymph, cerebrospinal fluid, aqueous humor, and sensorial fluid.
- 3. 19-3 Body Fluid Compartments: The total body fluid is distributed mainly between two compartments: the extra cellular fluid and the intracellular fluid. 1. Extra cellular fluids: All the fluids outside the cells are collectively called the extra cellular fluid. Together these fluids account for about 20 per cent of the body weight, or about 14 liters in a normal 70-kilogram adult. The extra cellular fluid contains the Interstitial fluid and the plasma. Interstitial fluid contains more than three fourths of the extra cellular fluid and plasma contains almost one fourth of the extra cellular fluid or about 3 liters.
- 4. 19-4 2. Intracellular fluids: All fluids inside the cells are collectively called the intracellular fluid. The intracellular fluid constitutes about 40 per cent of the total body weight in an “average” person. Note: There is another small compartment of fluid that is referred to as Tran cellular fluid. This compartment includes fluid in the sensorial, peritoneal, pericardial, and intraocular spaces, as well as the cerebrospinal fluid. It is usually considered to be a specialized type of extra cellular fluid. All the transcellular fluids together constitute about 1 to 2 liters.
- 5. 5 Functions of Blood • Transport of: – Gases, – nutrients, – waste products. • Regulation of pH and osmosis, • Maintenance of body temperature, • Protection against foreign substances, • Clot formation.
- 6. 6 Composition of Blood : - Plasma = straw colored liquid component of blood – Water = 92% – Solutes (plasma proteins) = 8% Formed elements = blood cells – Erythrocytes – Leukocytes – Thrombocytes
- 7. 7 Plasma Protiens : - Albumins = 55% of plasma proteins – Increases blood viscosity Globulins = 38% of plasma proteins – Gamma globulins – Serve as antibodies in immune response Fibrinogens = 7% of plasma proteins – Precursor to the protein fibrin – Major role in blood clotting mechanism
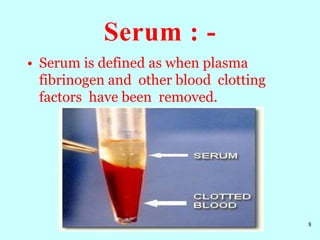
- 8. Serum : - 8 • Serum is defined as when plasma fibrinogen and other blood clotting factors have been removed.
- 9. Hematopoiesis or hemopoiesis : - • The process of formation of blood cells i.e. RBC’S, WBC’S and platelets is called as haematopoiesis and the sites where it occurs are known as hemopoietic tissues or organs (bone marrow, Liver, spleen). • Hematopoietic stem cells present in yolk sac migrate to other parts like spleen, liver and bone marrow. • The hematopoietic stem cells present in yolk sac at third week of embryo migrate to liver at around third month of foetal life. 9
- 10. • So, around third month of embryo the liver gets populated with these stem cells and become a major organ for haematopoiesis- DOMINANT MIGRATION. • Some hematopoietic stem cells also migrate to lymph nodes, spleen –MINOR MIGRATION. • Liver , lymph nodes and spleen continue as hematopoietic organs until birth. 10
- 11. • After birth, liver stops its hematopoietic activity because around 4 th month of foetal life migration of stem cells from liver, lymph nodes and spleen takes place to bone marrow. • So at time of fourth month of foetal life, hemopoiesis takes place in bone marrow. • Bone marrow is permanent residence for hematopoietic stem cells. • At time of birth, all hematopoietic stem cells are limited to bone marrow and bone marrow will be active. 11
- 12. • Active bone marrow is called as RED BONE MARROW and inactive bone marrow is called as YELLOW BONE MARROW. • Yellow bone marrow is accumulated with fat cells, so it is yellow in colour and red bone marrow is highly vascular and rich in hematopoietic stem cells. • In new born, if hematopoiesis is going on outside of bone marrow i.e. in liver, spleen and lymph nodes it is called as EXTRA MEDULLARY HEMATOPOIESIS. 12
- 14. 14 Such multipotential hematopoietic stem cells arise from the aorta-gonad-mesonephros region of the embryo (process illustrated below).
- 15. 15 Production of Formed Elements : - • Stem cells: All formed elements derived from single population. – Proerythroblasts: Develop into red blood cells, – Myeloblasts: Develop into basophils, neutrophils, eosinophils, – Lymphoblasts: Develop into lymphocytes, – Monoblasts: Develop into monocytes, – Megakaryoblasts: Develop into platelets.
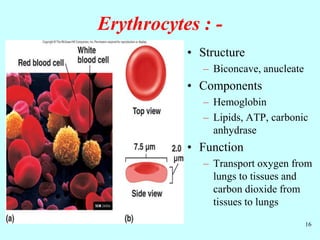
- 16. 16 Erythrocytes : - • Structure – Biconcave, anucleate • Components – Hemoglobin – Lipids, ATP, carbonic anhydrase • Function – Transport oxygen from lungs to tissues and carbon dioxide from tissues to lungs
- 17. 17 Erythropoiesis : - • Production of red blood cells called as an Erythropoiesis. – Stem cells proerythroblasts early erythroblasts intermediate late reticulocytes • Erythropoietin: Hormone to stimulate RBC production
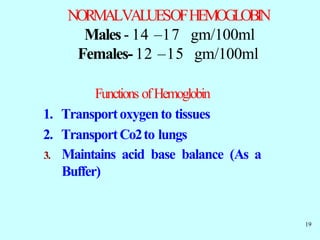
- 18. 18 Hemoglobin : - • It is a Red pigment Present in RBC of Blood. It is a conjugated protein, & Chromoprotein. It is made up of Iron and Protein. • Consists of: – 4 globin molecules: Transport carbon dioxide (carbonic anhydrase involved), nitric oxide. – 4 heme molecules: Transport oxygen • Iron is required for oxygen transport.
- 19. NORMALVALUESOFHEMOGLOBIN Males- 14 –17 gm/100ml Females- 12 –15 gm/100ml Functions ofHemoglobin 1. Transportoxygento tissues 2. TransportCo2to lungs 3. Maintains acid base balance (As a Buffer) 19
- 20. Formationof Hemoglobin:- i) 2 succinyl – CoA + 2 glysine Pyrrole ii) 4 Pyrrole Protoporphyrin IX iii) Protoporphyrin IX + Fe2+ Heme iv) Heme + Polypeptide Hemoglobin chain (α or β) v) 2 α chains + 2 β chains Haemoglobin A. 20
- 21. 21 Succinyl-CoA Glycine Pyridoxal phosphate αAmino -β-ketoadipic acid ALA (aminolevulinic acid )synthetase α amino-δ-Laevulinic acid ALAdehydrogenase. Porphobilinogen Protoporphyrin IX ferrous Haem globin haemoglobin
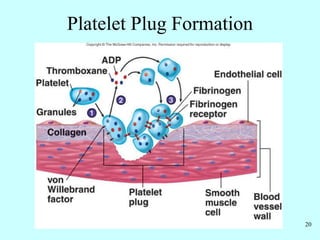
- 22. 22 Hemostasis : - • Arrest of bleeding, • Events preventing excessive blood loss : - – Vascular spasm: Vasoconstriction of damaged blood vessels, – Platelet plug formation, – Coagulation or blood clotting, – Fibrinolysis.
- 24. 24 Coagulation : - • Stages – Activation of prothrombinase – Conversion of prothrombin to thrombin – Conversion of fibrinogen to fibrin • Pathways – Extrinsic – Intrinsic
- 25. 25 Clot Formation : -
- 26. 26 Fibrinolysis : - • Clot dissolved by activity of plasmin, an enzyme which hydrolyzes fibrin
- 27. 27 Blood Groups : - Classified by genetically determined antigens located on the surface of erythrocytes. Two major classification systems : - – ABO System, – Rh System.
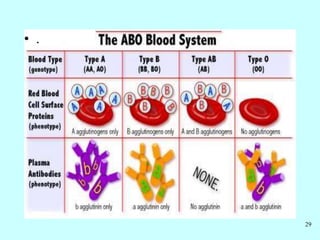
- 28. ABO blood System: - In ABO blood system classification of human blood based on the inherited properties of red blood cells (erythrocytes) as determined by the presence or absence of the antigens A and B, which are carried on the surface of the red cells. Persons may have type A, type B, type O, or type AB blood. Transfusion Reaction 28
- 29. 29 • .
- 30. Rh Blood Grouping : - Also based upon antigens located on the surface of erythrocytes. Named because it was first worked out on blood of Rhesus monkeys, Rh+ = 85% people have Rhesus antigen, and they do not make anti-Rhesus antibodies. Rh- = Remaining 15% peoples have no Rhesus antigen hence they make anti- Rhesus antibodies. 30
- 31. Rh Blood Groupings : - 31 If an Rh- person receives blood from an Rh+ donor, the body will start to make Rh+ antibodies (agglutinins) If during a second transfusion, Rh+ blood is again given, the antibodies produced after receiving the first transfusion will cause hemolysis of the blood from the second transfusion May result in death.
- 32. Blood transfusions : - Person with type A blood – May receive blood from type A or O donor – May not receive type B or AB blood Person with type B blood – May receive blood from type B or O donor – May not receive type A or AB blood Person with type AB blood – May receive blood from type A, type B, or type O donors – (universal recipients). 32
- 33. Person with type O blood – May only receive blood from type O donors – May donate blood to all other blood types – (Universal donors) 33
- 34. Blood Disorders : - 34 • .
- 35. Leukemia : - Malignant disease of blood forming tissue. Uncontrolled production and accumulation of immature WBC’s. May prevent production of normal RBC’s. May have uncontrolled infection due to abundance of immature or abnormal wbc’s that cannot fight infection or disease. 35
- 36. Infectious mononucleosis : - Contagious (i. e. spread from one persone to another persone) disease primarily affecting the lymph tissue but also affecting the blood. Caused by the epstein - barr virus (EBV). Occurs mainly in children and young adults. Affects females 3 times more than male. Most commonly transmitted through oral contact. Flu like symptoms, chronic fatigue. 36
- 37. Polycythemia : - It is an abnormally increased concentration of haemoglobin in the blood, either through reduction of plasma volume or increase in red cell numbers. It may be a primary disease of unknown cause, or a secondary condition linked to respiratory or circulatory disorder or cancer. Results in increased blood viscosity and elevated blood pressure. 37
- 38. Anemia : - Anaemia is a condition in which deficiency of red cells or of haemoglobin in the blood. Reduced oxygen carrying capacity of the blood. Nutritional anemia = caused by dietary deficiency due to inadequate iron, amino acids, or vitamin B12 consumption. Pernicious anemia = anemia due to insufficient hematopoiesis. Hemorrhagic anemia = anemia due to excessive loss of rbc’s due to bleeding. 38
- 39. Hemolyticanemia = anemia due to premature rupture of RBC membrane spilling hemoglobin and other cellular contents into the plasma: - – Hemoglobin defects – Abnormal RBC enzymes – Defects in RBC membrane – Parasites - toxins – Antibodies from incompatible blood Thalassemia = type of hereditary hemolytic anemia due to a defect in the production of hemoglobin 39
- 40. Aplastic anemia = anemia due to the destruction or inhibition of red bone marrow. Sickle cell anemia = due to abnormal hemoglobin (S shaped) that causes RBC to bend into a sickle shape. – Cells rupture easily – Cells get cut off blood supply to organs – Inherited condition due to faulty gene for hemoglobin production and formation 40
- 41. 41 Normal Sickle Sickle cell anemia
- 42. Hemophilia : - 42 It hereditary disorder of the coagulation process (blood will not clot) due to the lack of certain clotting factors in the blood (factor VIII).
- 43. Reticulo endothelial System : - • Reticuloendothelial System:-It is a network of cells and tissues found throughout the body, especially in the blood, general connective tissue, spleen, liver, lungs, bone marrow, and lymph nodes. They have both endothelial and reticular attributes and the ability to take up colloidal dye particles. Some of the reticuloendothelial cells found in the blood and in the general connective tissue are large in size. 43
- 44. • These cells are concerned with blood cell formation and destruction, storage of fatty materials, and metabolism of iron and pigment, and they play a role in inflammation and immunity. Some of the cells are motile —that is, capable of spontaneous motion— and phagocytic— they can ingest and destroy unwanted foreign material. 44
- 45. • The reticulo endothelial cells of the SPLEEN possess the ability to dispose of disintegrated erythrocytes. They do not, however, destroy hemoglobin, which is liberated in the process. The reticuloendothelial cells located in the blood cavities of the LIVER are called Kupffer cells. (i.e. a phagocytic cell which located in the liver and is involved in the breakdown of red blood cells are called as an Kupffer cells.) 45
- 46. These cells, together with the cells of gener al connective tissue and bone marrow, are capable of transforming into bile pigment then hemoglobin released by disintegrated erythrocytes. Microglial cells are a specialised population of macrophages that are found in the central nervous system (CNS). They remove damaged neurons and infections and are important for maintaining the health of the CNS. 43
- 47. Reticulo endothelial System : - 47
- 48. References: 1. Human Anatomy and Physiology-I, By Dr. Mahesh Prasad, Dr. Antesh Kumar Jha, Mr. Ritesh Kumar Srivastav, Nirali Prakashan, As per PCI Syllabus. Page No. 3.1 to 3.21. 2. Human Anatomy and Physiology-I, By Dr. S. B. Bhise and Dr. A. V. Yadav. Nirali Prakashan, As per PCI Syllabus. Page No. 5.1 to 5.14. 3. www.google.com.
- 49. Thank you 49