Ventilator
- 2. Prof. Dr. RS Mehta, BPKIHS 2
- 3. VENTILATOR A mechanical Prof. Dr. RS Mehta, BPKIHS 3 ventilator is a positive or negative pressure breathing device that can maintain ventilation and oxygen delivery for a prolonged period. Mechanical ventilation has been used for decades to support the respiratory functions of patients with various degrees of respiratory distress or failure.
- 4. Prof. Dr. RS Mehta, BPKIHS 4
- 5. Prof. Dr. RS Mehta, BPKIHS 5
- 6. PURPOSES To maintain gas exchange in case of acute and chronic respiratory failure. To maintain ventilatory support after CPR. To reduce pulmonary vascular resistance. To excrete increased CO2 production. To give general anesthesia with muscle relaxants. Prof. Dr. RS Mehta, BPKIHS 6
- 7. Indications for Mechanical Ventilation Upper airway obstruction and Lower airway obstruction as a result of blockage. Neuromuscular disorders as in Myasthenia gravis, Poliomyelitis, Gullian-Barre syndrome, Snake bite and inadequate reversal of anesthesia. Prof. Dr. RS Mehta, BPKIHS 7
- 8. ContD… Prof. Dr. RS Mehta, BPKIHS 8 Lung diseases which prevent proper exchange of O2 and CO2 as in Chest Injuries Pneumothorax, lung Infections, COPD, Acute Respiratory Distress Syndrome (ARDS). Post-operative cardiac surgery, any other surgery, shock & trauma. Respiratory arrest.
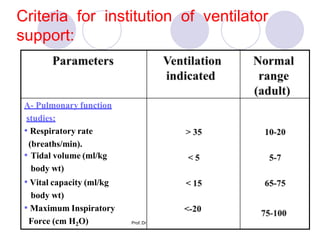
- 9. Criteria for institution of ventilator support: A- Pulmonary function studies: • Respiratory rate (breaths/min). • Tidal volume (ml/kg body wt) • Vital capacity (ml/kg body wt) • Maximum Inspiratory Force (cm H2O) Prof. Dr
- 10. Criteria for institution of ventilatory support: Prof. Dr. RS Mehta, BPKIHS 10
- 11. CLASSIFICATION OF VENTILATORS Ventilator Positive pressure Negative pressure Prof. Dr. RS Mehta, BPKIHS 11
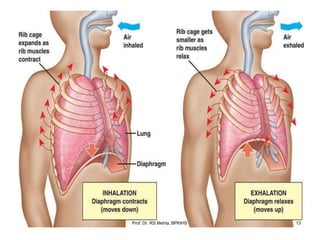
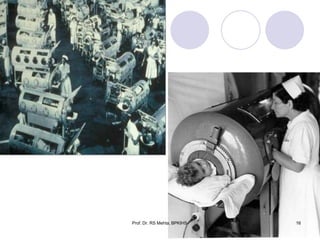
- 12. NEGATIVE PRESSURE VENTILATOR Elongated tank, which encases the patient up to the neck. The neck is sealed with a rubber gasket, the patient's face are exposed to the room air. These exert negative pressure on the external chest decreasing the intra-thoracic pressure during inspiration, allows air to flow into the lungs, filling its volume. The cessation of the negative pressure causes the chest wall to fall and exhalation to occur. Prof. Dr. RS Mehta, BPKIHS 12
- 13. Prof. Dr. RS Mehta, BPKIHS 13
- 14. Contd… These are simple to use and do not require intubations of the airway; consequently, they are especially adaptable for home use. It is used mainly in chronic respiratory failure associated with neuromuscular conditions such as poliomyelitis, muscular dystrophy and myasthenia gravis. The use of negative-pressure ventilators is restricted in clinical practice, however, because they limit positioning and movement and they lack adaptability to large or small body torsos (chests). Prof. Dr. RS Mehta, BPKIHS 14
- 15. Prof. Dr. RS Mehta, BPKIHS 15
- 16. Prof. Dr. RS Mehta, BPKIHS 16
- 17. POSITIVE PRESSURE VENTILATION Prof. Dr. RS Mehta, BPKIHS 17 Positive pressure ventilators inflate the lungs by exerting positive pressure on the airway forcing the alveoli to expand during inspiration. Expiration occurs passively.
- 18. ContD… Prof. Dr. RS Mehta, BPKIHS 18 Positive-pressure ventilators require an artificial airway (Endotracheal or tracheostomy tube) and use positive pressure to force gas into a patient's lungs. Inspiration can be triggered either by the patient or the machine.
- 19. Origins of mechanical ventilation •Negative-pressure ventilators (“iron lungs”) • Non-invasive ventilation first used in Boston Children’s Hospital in 1928 • Used extensively during polio outbreaks in 1940s – 1950s •Positive-pressure ventilators • Invasive ventilation first used at Massachusetts General Hospital in 1955 • Now the modern standard of mechanical ventilation The era of intensive care medicine began with positive-pressure ventilation The iron lung created negative pressure in abdomen as well as the chest, decreasing cardiac output. in 1953. Iron lung polio ward at Rancho Los Amigos Hospit1a8lProf. Dr. RS Mehta, BPKIHS
- 20. Mechanical Ventilators Classification Prof. Dr. RS Mehta, BPKIHS 20
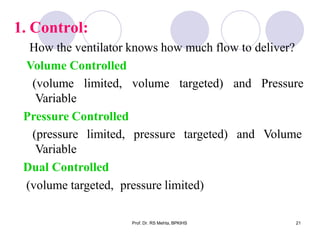
- 21. 1. Control: Prof. Dr. RS Mehta, BPKIHS 21 How the ventilator knows how much flow to deliver? Volume Controlled (volume limited, Variable Pressure Controlled volume targeted) and Pressure (pressure limited, pressure targeted) Variable Dual Controlled (volume targeted, pressure limited) and Volume
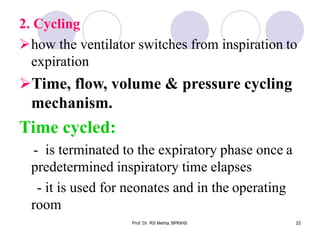
- 22. 2. Cycling how the ventilator switches from inspiration to expiration Time, flow, volume & pressure cycling mechanism. Time cycled: - is terminated to the expiratory phase once a predetermined inspiratory time elapses - it is used for neonates and in the operating room Prof. Dr. RS Mehta, BPKIHS 22
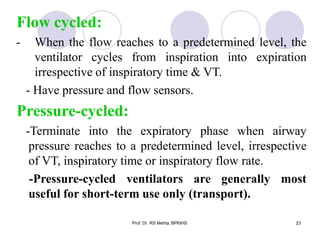
- 23. Flow cycled: Prof. Dr. RS Mehta, BPKIHS 23 - When the flow reaches to a predetermined level, the ventilator cycles from inspiration into expiration irrespective of inspiratory time & VT. - Have pressure and flow sensors. Pressure-cycled: -Terminate into the expiratory phase when airway pressure reaches to a predetermined level, irrespective of VT, inspiratory time or inspiratory flow rate. -Pressure-cycled ventilators are generally most useful for short-term use only (transport).
- 24. Volume cycled: Prof. Dr. RS Mehta, BPKIHS 24 Terminate in inspiration when a preselected volume is delivered. Many adult ventilators are volume cycled but also have secondary limits on inspiratory pressure to guard against pulmonary barotrauma. If inspiratory pressure exceeds the pressure limit, the machine cycles into expiration even if the selected volume has not been delivered.
- 25. 3. Triggering Prof. Dr. RS Mehta, BPKIHS 25 (What causes the ventilator to cycle to inspiration? ) Time: The ventilator cycles at a set frequency as determined by the controlled rate. Pressure: The ventilator senses the pt's inspiratory effort by way of a ↓ in the baseline pressure. Flow: Modern ventilators deliver a constant flow around the circuit throughout the respiratory cycle. A deflection in this flow by patient inspiration, is monitored by the ventilator and it delivers a breath, requires less work by the patient than pressure triggering.
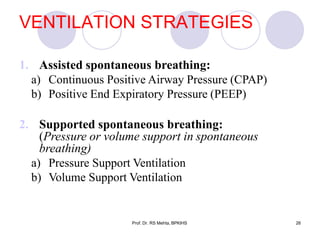
- 26. VENTILATION STRATEGIES Prof. Dr. RS Mehta, BPKIHS 26 1. Assisted spontaneous breathing: a) Continuous Positive Airway Pressure (CPAP) b) Positive End Expiratory Pressure (PEEP) 2. Supported spontaneous breathing: (Pressure or volume support in spontaneous breathing) a) Pressure Support Ventilation b) Volume Support Ventilation
- 27. ContD… Prof. Dr. RS Mehta, BPKIHS 27 3. Mixed respiratory support: a) Intermittent Mandatory Ventilation (IMV) b) Synchronized Intermittent Mandatory Ventilation (SIMV). 4. Controlled mechanical ventilation: a) Pressure Controlled Ventilation b) Volume Controlled Ventilation c) Controlled Ventilation d) High Frequency Ventilation
- 28. Important ventilation modes Prof. Dr. RS Mehta, BPKIHS 28 Controlled Mechanical Ventilation (CMV) - Pressure Controlled Ventilation (PCV) - Volume Controlled Ventilation (VCV) Intermittent Positive Pressure Ventilation (IPPV) Pressure Support Ventilation (PSV) Synchronized Intermittent Mandatory Ventilation (SIMV) Bi-level Positive Airway Pressure (BIPAP) Continuous positive airway pressure (CPAP) Inverse Ratio Ventilation (IRV)
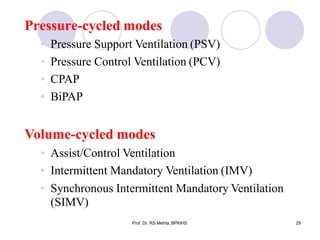
- 29. Pressure-cycled modes Prof. Dr. RS Mehta, BPKIHS 29 • Pressure Support Ventilation (PSV) • Pressure Control Ventilation (PCV) • CPAP • BiPAP Volume-cycled modes • Assist/Control Ventilation • Intermittent Mandatory Ventilation (IMV) • Synchronous Intermittent Mandatory Ventilation (SIMV)
- 30. CPAP The effect of CPAP is compared to inflating a balloon but not letting it completely deflate before inflating it again. The second inflation is easier to perform because resistance is decreased. A continuous level of elevated pressure is provided through the patient circuit to maintain adequate oxygenation, decrease the work of breathing. CPAP may be used invasively through an endotracheal tube or tracheostomy or non- invasively with a face mask or nasal prongs. Prof. Dr. RS Mehta, BPKIHS 30
- 31. PEEP Prof. Dr. RS Mehta, BPKIHS 31 PEEP is positive pressure that is applied by the ventilator at the end of expiration. This mode does not deliver breaths but is used as an adjunct to CV and SIMV to improve oxygenation by opening collapsed alveoli at the end of expiration.
- 32. CONTd… Prof. Dr. RS Mehta, BPKIHS 32 Complications from the increased pressure can include decreased cardiac output, lung rupture, and increased intracranial pressure. It is used to increase the surface area to prevent collapse of alveoli and to prevent atelectasis. PEEP is functionally the same as CPAP, but refers to the use of an elevated pressure during the expiratory phase of the ventilatory cycle.
- 33. Prof. Dr. RS Mehta, BPKIHS 33 A mode of mechanical ventilation in which the patient is allowed to breathe independently except during certain prescribed intervals, when a ventilator delivers a breath either under positive pressure or in a measured volume. INTERMITTENT MANDATORY VENTILATION
- 34. Synchronized Intermittent Mandatory Ventilation (SIMV) In this mode the ventilator provides a pre-set mechanical breath (pressure or volume limited) every specified number of seconds (determined by dividing the respiratory rate into 60 - thus a respiratory rate of 12 results in a 5 second cycle time). Within that cycle time the ventilator waits for the patient to initiate a breath using either a pressure or flow sensor. When the ventilator senses the first patient breathing attempt within the cycle, it delivers the preset ventilator breath. If the patient fails to initiate a breath, the ventilator delivers a mechanical breath at the end of the breath cycle. Prof. Dr. RS Mehta, BPKIHS 33
- 35. CONTD… SIMV is used as a primary mode of ventilation as well as a weaning mode. (During weaning, the preset rate is gradually reduced, allowing the patient to slowly regain breathing on their own.) The disadvantage of this mode is that it may increase the effort of breathing and cause respiratory muscle fatigue. When patient is breathing independently and adequately, ventilator does not support. Note: The ventilator initiates each breath in synchrony with the patient's breaths . Prof. Dr. RS Mehta, BPKIHS 35
- 36. CONTROLLED VENTILATION: IPPV Prof. Dr. RS Mehta, BPKIHS 36 The ventilator initiates and controls both the volume delivered and the frequency of breaths. • This mode is used for patients who are unable to initiate a breath. • It is indicated in patients with apnea, drug overdose, spinal cord injuries, CNS dysfunction, flail chest, neuromuscular disease, and paralysis from drugs. • If it is used with spontaneously breathing patients, they must be sedated and/or pharmacologically paralyzed so they don't breathe out of synchrony with the ventilator.
- 37. ASSIST CONTROL VENTILATION Prof. Dr. RS Mehta, BPKIHS 37 This mode is used for pts. who can initiate a breath but who have weakened respiratory muscles. In this mode, the ventilator provides a mechanical breath with either a pre-set tidal volume or peak pressure every time the pt. initiates a breath. If the pt. fail to initiate inspiration, the ventilator automatically goes into the back up mode and delivers the pre set rate and tidal volume until it senses an inspiratory effort. It is used in disease conditions like Myasthenia gravis, GB syndrome, post cardiac/respiratory arrest, pulmonary edema, ARDS, etc.
- 38. INVERSE RATIO VENTILATION (IRV) Prof. Dr. RS Mehta, BPKIHS 38 The normal inspiratory: expiratory ratio is 1:2, but this is reversed during IRV to 2:1 or greater (the maximum is 4:1). This method is used for patients who are still hypoxic, even with the use of PEEP.
- 39. CONTD… Prof. Dr. RS Mehta, BPKIHS 39 Longer inspiratory time increases the amount of air in the lungs at the end of expiration (the functional residual capacity) and improves oxygenation by re-expanding collapsed alveoli. The shorter expiratory time prevents the alveoli from collapsing again. This method requires sedation and therapeutic paralysis because it is very uncomfortable for the patient.
- 40. Time Cycled Ventilators Time-cycled ventilators terminate or control inspiration after a pre-set time. These ventilators are used in newborn & infants. Prof. Dr. RS Mehta, BPKIHS 40
- 41. There are several ventilation modes, the most important are: Summary Prof. Dr. RS Mehta, BPKIHS 40 Controlled Mechanical Ventilation (CMV) - Pressure Controlled Ventilation (PCV) - Volume Controlled Ventilation (VCV) Intermittent Positive Pressure Ventilation (IPPV) Pressure Support Ventilation (PSV) Synchronized Intermittent Mandatory Ventilation (SIMV) Bi-level Positive Airway Pressure (BIPAP) Continuous positive airway pressure (CPAP) Inverse Ratio Ventilation (IRV)
- 42. Summary… Prof. Dr. RS Mehta, BPKIHS 40 Pressure-cycled modes • Pressure Support Ventilation (PSV) • Pressure Control Ventilation (PCV) • CPAP • BiPAP Volume-cycled modes • Assist/Control • Intermittent Mandatory Ventilation (IMV) • Synchronous Intermittent Mandatory Ventilation (SIMV)
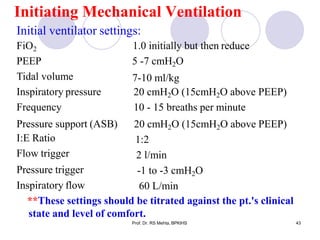
- 43. Initiating Mechanical Ventilation Prof. Dr. RS Mehta, BPKIHS 43 Initial ventilator settings: FiO2 PEEP Tidal volume Inspiratory pressure Frequency Pressure support (ASB) I:E Ratio Flow trigger Pressure trigger Inspiratory flow 1.0 initially but then reduce 5 -7 cmH2O 7-10 ml/kg 20 cmH2O (15cmH2O above PEEP) 10 - 15 breaths per minute 20 cmH2O (15cmH2O above PEEP) 1:2 2 l/min -1 to -3 cmH2O 60 L/min **These settings should be titrated against the pt.'s clinical state and level of comfort.
- 44. Prof. Dr. RS Mehta, BPKIHS 44
- 45. Indications for intubation Prof. Dr. RS Mehta, BPKIHS 45 •Criteria • Clinical deterioration • Tachypnea: RR >35 • Hypoxia: pO2<60mm Hg • Hypercarbia: pCO2 > 55mm Hg • Minute ventilation<10 L/min • Tidal volume <5-10 ml/kg • Negative inspiratory force < 25cm H2O (how strong the pt can suck in) •Initial vent settings • FiO2 = 50% • PEEP = 5cm H2O • RR = 12 – 15 breaths/min • VT = 10 – 12ml/kg • COPD = 10 ml/kg (prevent over- inflation) • ARDS = 8 ml/kg (prevent volu-trauma) • Permissive hyper-capnea • Pressure Support = 10cm H2O How the values trend should significantly impact clinical decisions
- 46. Indications for extubation Prof. Dr. RS Mehta, BPKIHS 46 • Demonstrated to be superior •Clinical parameters • Resolution/Stabilization of disease process • Hemodynamically stable • Intact cough/gag reflex • Spontaneous respirations • Acceptable vent settings • FiO2< 50%, PEEP < 8, PaO2 > 75, pH > 7.25 •General approaches • SIMV Weaning • Pressure Support Ventilation (PSV) Weaning • Spontaneous breathing trials and use of T-piece No weaning parameter completely accurate when used alone Numerical Parameters Normal Range Weaning Threshold P/F > 400 > 200 Tidal volume 5 - 7 ml/kg 5 ml/kg Respiratory rate 14 - 18 breaths/min < 40 breaths/min Vital capacity 65 - 75 ml/kg 10 ml/kg Minute volume 5 - 7 L/min < 10 L/min Greater Predictive Value Normal Range Weaning Threshold NIF (Negative Inspiratory Force) > - 90 cm H2O > - 25 cm H2O RSBI (Rapid < 50 < 100 Shallow Breathing Index) (RR/TV) Marino P, The ICU Book (2/e). 1998.
- 47. Spontaneous Breathing Trials SBTs do not guarantee that airway is stable or pt can self-clear secretions •Settings • PEEP = 5, PS = 0 – 5, FiO2 < 40% • Breathe independently for 30 – 120 min • ABG obtained at end of SBT •Failed SBT Criteria • RR > 35 for >5 min a 2• S O <90% for >30 sec • HR > 140 • Systolic BP > 180 or < 90mm Hg • Sustained increased work of breathing • Cardiac dysrhythmia • pH < 7.32 Causes of Failed SBTs Treatments Anxiety/Agitation Benzodiazepines or haldol Infection Diagnosis and tx Electrolyte abnormalities (K+, PO4-) Correction Pulmonary edema, cardiac ischemia Diuretics and nitrates Deconditioning, malnutrition Aggressive nutrition Neuromuscular disease Bronchopulmonary hygiene, early consideration of trach Increased intra-abdominal pressure Semirecumbent positioning, NGT Hypothyroidism Thyroid replacement Excessive auto-PEEP (COPD, asthma) Bronchodilator therapy Sena et al, ACS Surgery: Principles and Practice (2005). 46 Prof. Dr. RS Mehta, BPKIHS
- 48. Guidelines Suggesting the Need for Mechanical Ventilation Prof. Dr. RS Mehta, BPKIHS 47 Parameters that help us to guide to take the decision whether mechanical ventilation is needed or not? 1. Cl. Indices: Apnea with respiratory arrest RR >35 breaths per minute Paralysis of breathing muscle- GBS, MG head trauma, coma - an absent gag or cough reflex. - Effect of anesthetic and muscle relaxant - Others: shock, CCF, sepsis
- 49. 2. Mechanical indices Vital capacity <15 mL/kg Tidal volume <5 mL/ kg Maximum inspiratory force < –25 cm H2O 3. Respiratory gas tensions Direct indices PaO2 (<60 mm Hg) PaCO2 (>50 mm Hg with pH <7.25) Derived indices PaO2/FIO2 ratio < 300 mmHg Prof. Dr. RS Mehta, BPKIHS 47
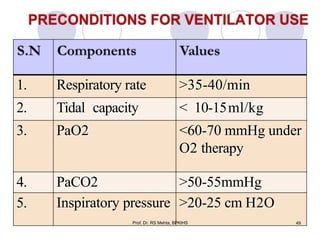
- 50. 1. Respiratory rate >35-40/min 2. Tidal capacity < 10-15ml/kg 3. PaO2 <60-70 mmHg under O2 therapy 4. 5. 49 PaCO2 >50-55mmHg Inspiratory pressure >20-25 cm H2O Prof. Dr. RS Mehta, BPKIHS
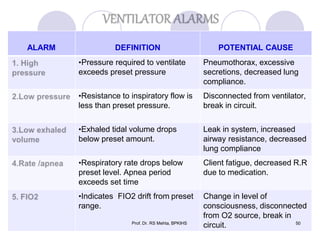
- 51. ALARM DEFINITION POTENTIAL CAUSE •Pressure required to ventilate exceeds preset pressure Pneumothorax, excessive secretions, decreased lung compliance. •Resistance to inspiratory flow is less than preset pressure. Disconnected from ventilator, break in circuit. •Exhaled tidal volume drops below preset amount. Leak in system, increased airway resistance, decreased lung compliance •Respiratory rate drops below preset level. Apnea period exceeds set time Client fatigue, decreased R.R due to medication. •Indicates FIO2 drift from preset range. Prof. Dr. RS Mehta, BPKIHS Change in level of consciousness, disconnected from O2 source, break in circuit. 50
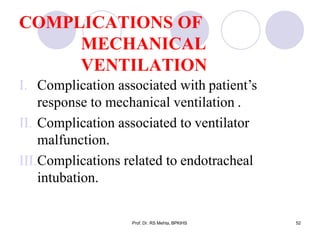
- 52. COMPLICATIONS OF MECHANICAL VENTILATION Prof. Dr. RS Mehta, BPKIHS 52 I. Complication associated with patient’s response to mechanical ventilation . II. Complication associated to ventilator malfunction. III.Complications related to endotracheal intubation.
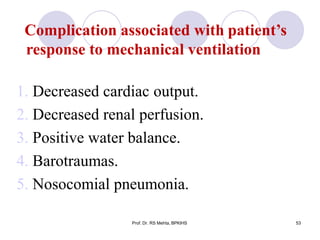
- 53. Complication associated with patient’s response to mechanical ventilation 1. Decreased cardiac output. 2. Decreased renal perfusion. 3. Positive water balance. 4. Barotraumas. 5. Nosocomial pneumonia. Prof. Dr. RS Mehta, BPKIHS 53
- 54. Complication associated to ventilator malfunction Prof. Dr. RS Mehta, BPKIHS 54 1. Alarms turned off or non-functional – may lead to apnea and respiratory arrest. 2. Low exhaled volume.
- 55. Complications related to endotracheal intubation Prof. Dr. RS Mehta, BPKIHS 55 1. Sinusitis and nasal injury 2. Tracheoesophageal fistula 3. Laryngeal or tracheal stenosis 4. Cricoid abscess
- 56. NURSING CARE OF PATIENTS ON VENTILATOR Prof. Dr. RS Mehta, BPKIHS 56 PHYSIOLOGICAL NEEDS: comfort activity nutrition elimination of wastes Patients are often not able to fulfill these needs by themselves, nursing function is then for example seeing to comfort, determining intake and output together with blood chemistry to assess adequacy of intravenous nutrition, and so on.
- 57. CONTD… Prof. Dr. RS Mehta, BPKIHS 57 SAFETY NEEDS: Threat of injury by person or machines Medication must be checked. Machines must be in best working condition. NEED TO BELONG: Security, means of communication Staff must communicate with the patient and patient must be allowed to respond. Patients need constant reassurance.
- 58. CONTD… Prof. Dr. RS Mehta, BPKIHS 58 NEED FOR RECOGNITION: Esteem, dignity, respect Patients must be treated with respect and addressed correctly. the choice and NEED TO CREATE: Expression of self, need to contribute Patients must be involved in implementation of their treatment.
- 59. CONTD.. Prof. Dr. RS Mehta, BPKIHS 59 NEED TO KNOW AND UNDERSTAND: Need for knowledge and comprehension An explanation of diagnosis and treatment on the patient’s level. SELF ACTUALIZATION: Order, truth, privacy Patients should have as much privacy as possible — pull screens or close doors. The patient has the right to be told the truth.
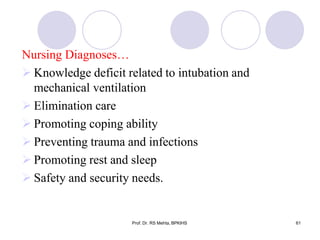
- 60. Nursing Diagnoses Prof. Dr. RS Mehta, BPKIHS 60 Ineffective breathing pattern Potential for pulmonary infection Impaired water and fluid regulation Oral hygiene Potential altered nutritional status: less than body requirement related to NPO status Potential for complications related to immobility
- 61. Nursing Diagnoses… Knowledge deficit related to intubation and mechanical ventilation Elimination care Promoting coping ability Preventing trauma and infections Promoting rest and sleep Safety and security needs. Prof. Dr. RS Mehta, BPKIHS 61
- 62. Prof. Dr. RS Mehta, BPKIHS 62
- 63. WEANING: Weaning is the process of withdrawing mechanical ventilator support and transferring the work of breathing from the ventilator to the patient. It is done only when patient is free from the cause to be kept on mechanical ventilation. Weaning success is defined as effective spontaneous breathing without any mechanical ventilation for 24 hours or more. Prof. Dr. RS Mehta, BPKIHS 63
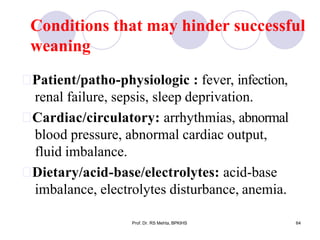
- 64. Conditions that may hinder successful weaning Prof. Dr. RS Mehta, BPKIHS 64 Patient/patho-physiologic : fever, infection, renal failure, sepsis, sleep deprivation. Cardiac/circulatory: arrhythmias, abnormal blood pressure, abnormal cardiac output, fluid imbalance. Dietary/acid-base/electrolytes: acid-base imbalance, electrolytes disturbance, anemia.
- 65. Criteria for weaning Prof. Dr. RS Mehta, BPKIHS 65 Tidal volume be above a given threshold (greater than 5 ml/kg), Respiratory frequency be below a given count (less than 30 breaths/min), Oxygen partial pressure be above a given threshold (PaO2 greater than 60mm Hg) and FIO2 <40% Vital capacity 10 to 15 ml/kg.
- 66. Since weaning is the graded removal of a therapeutic modality, the sudden withdrawal will not be tolerated. So, weaning from the following 5 modalities should be independently assessed. 1. Supplemental oxygen 2. PEEP 3. Mechanical ventilation 4. Artificial airway 5. Ionotrops Prof. Dr. RS Mehta, BPKIHS 66
- 67. Methods of Weaning Prof. Dr. RS Mehta, BPKIHS 67 1 T-piece trial, 2 Continuous Positive Airway Pressure (CPAP) weaning, 3 Synchronized Intermittent Mandatory Ventilation (SIMV) weaning, 4 Pressure Support Ventilation (PSV) weaning.
- 68. Signs of Weaning Intolerance Criteria Prof. Dr. RS Mehta, BPKIHS 68 Diaphoresis Dyspnoea & Labored respiratory pattern Increased anxiety, Restlessness, Decrease in level of consciousness Dysrhythmia, Increase or decrease in heart rate of > 20 beats /min. or heart rate > 110 b/m, Sustained heart rate >20% higher or lower than baseline
- 69. Criteria… Increase or decrease in blood pressure of > 20 mm Hg Systolic blood pressure >180 mm Hg or <90 mm Hg Increase in respiratory rate of > 10 above baseline or > 30 Sustained respiratory rate greater than 35 breaths/minute Tidal volume ≤5 ml/kg, Sustained minute ventilation <200 ml/kg/minute SpO2 < 90%, PaO2 < 60 mmHg, decrease in PH of < 7.35. Increase in PaCO2. Prof. Dr. RS Mehta, BPKIHS 69
- 70. NURSING CARE OF THE PATIENT BEING WEANED Assess the client for the weaning criteria. Monitor the activity level, assess dietary intake and monitor results of the lab tests. Assess client’s & family’s level of understanding of weaning. Explain that patient may feel shortness of breath initially & provide encouragement as needed. Monitor vital signs, pulse oximetry, ECG changes, ABG analysis & respiratory pattern continuously for the first 20-30 min & then every 5 min until weaning is complete. 69Prof. Dr. RS Mehta, BPKIHS
- 71. Nursing Care… Prof. Dr. RS Mehta, BPKIHS 71 Implement the weaning method prescribed: ASB, IMV, SIMV, CPAP, T-piece, etc…. Maintain a patent airway, suction the airway as needed. Monitor the ABG level & Pulmonary Function Test as per requirement. Terminate the weaning if adverse reactions occur. Assess psychological dependence if the physiologic parameters indicate weaning is feasible or patient still resists.
- 72. Elimination Care: Prof. Dr. RS Mehta, BPKIHS 72 Catheter care Proper cleaning, use of bed pan if possible. Optimal Level of Mobility: The nurse should help active or passive range of motion every 6-8 hours to prevent contractures and venous stasis.
- 73. Promoting Optimal Communication: Assessment of the ability of the ventilator- dependent patient's to communicate and thus identify the patient's limitations. Use non-verbal methods of communication. Use of signals, signs, nodding, palm writing, lip reading. Provide paper & pencil, magic slate. Be alert to non-verbal clues. Allow patient to respond and repeat explanations. Prof. Dr. RS Mehta, BPKIHS 73
- 74. Preventing trauma and infections: Prof. Dr. RS Mehta, BPKIHS 74 Positioning of the ventilator tubing should be such that there is minimal pulling or distortion of the tube in the trachea to reduce the risk of trauma to the trachea. Monitoring of cuff pressure every 8 hrs to maintain the pressure less than 25cm of H2O. Tracheotomy care at least every 8 hourly & more frequent if need.
- 75. Preventing trauma and infections… Prof. Dr. RS Mehta, BPKIHS 75 Oral care frequently because the oral cavity is the primary source of contamination of the lungs in the intubated and compromised patients. The naso-gastric tube can increase the risk of aspiration, leading to nosocomial pneumonia hence the patient should be positioned with the head elevated above the stomach. All prescribed medications should be given on time.
- 76. Promoting coping Ability: Prof. Dr. RS Mehta, BPKIHS 76 Encouraging family to verbalize their feelings about the ventilators, patient's condition is beneficial. Explanation about the procedures every time they are performed helps to reduce anxiety.
- 77. Rest & Sleep: Prof. Dr. RS Mehta, BPKIHS 77 Keep calm & quiet environment. Turn monitor alarm down if possible. Provide dim light during night & soft music if possible. Cover patient eyes with clean gauze.
- 78. Oral Hygiene: Prof. Dr. RS Mehta, BPKIHS 78 Provide oral care every 2 hourly as oral mucus membranes dry in 2 hours. Moisten the mouth with solutions that do not contain alcohol or lemon. Moistens the lips with lubricant. It prevents drying, cracking & excoriation. Brush the client’s teeth as twice daily as dental caries are prevented by saliva. Suction oral secretions from the mouth as secretions pool in oro-pharynx because of the inflated tracheal cuff. Assess for pressure areas at the corner of the mouth.
- 79. SAFETY & SECURITY NEEDS Prof. Dr. RS Mehta, BPKIHS 79 Secure physically, mentally, emotionally. Prevent trauma & infection Perform hand-hygiene & adopt sterile techniques. Prevention of cross-infection & nosocomial infection. Maintain warm & adequate body temperature. Put side-rails. Visiting hours should be defined.
- 80. ARTIFICIAL AIRWAY: 1. COMBITUBE. 2. LMA (Laryngeal Mask Airway) 3. OROPHARYNGEAL airway 4. NASOPHARYNGEAL airway 5. ETT 6. TRACHEOSOTOMY tube. Prof. Dr. RS Mehta, BPKIHS 79
- 81. 0ropharyngeal Airway: There are A.A. with length 25-35 cm, sized 5-10 mm (acco. Int. diameter), vol. capacity of ET tube is from 35- 45 ml (which is abt. About half the vol. of anatomical dead space in adults 1ml/kg). 80Prof. Dr. RS Mehta, BPKIHS
- 82. THANK YOU!!! 81 Prof. Dr. RS Mehta, BPKIHS