Nutrition and Mental Health
- 1. Nutrition as a Factor inNutrition as a Factor in Mental HealthMental Health The evidence is steadily increasing !The evidence is steadily increasing ! Mona Moorhouse B.Sc., B.Ed., RDMona Moorhouse B.Sc., B.Ed., RD Registered Dietitian, Royal Ottawa Mental Health CenterRegistered Dietitian, Royal Ottawa Mental Health Center
- 2. OutlineOutline 1.Discuss studies on nutrition and:1.Discuss studies on nutrition and: MoodMood Drug DependenceDrug Dependence Alzheimer’s DiseaseAlzheimer’s Disease 2.Review some diet recommendations.2.Review some diet recommendations. 3.Questions3.Questions
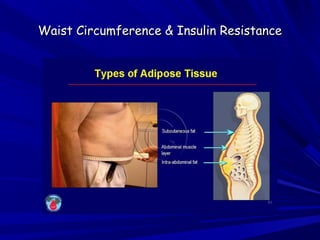
- 3. Waist Circumference & Insulin ResistanceWaist Circumference & Insulin Resistance
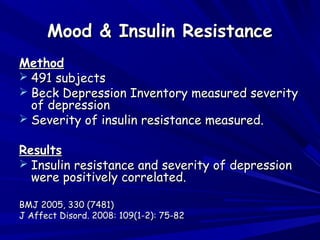
- 5. Mood & Insulin ResistanceMood & Insulin Resistance MethodMethod 491 subjects491 subjects Beck Depression Inventory measured severityBeck Depression Inventory measured severity of depressionof depression Severity of insulin resistance measured.Severity of insulin resistance measured. ResultsResults Insulin resistance and severity of depressionInsulin resistance and severity of depression were positively correlated.were positively correlated. BMJ 2005, 330 (7481)BMJ 2005, 330 (7481) J Affect Disord. 2008: 109(1-2): 75-82J Affect Disord. 2008: 109(1-2): 75-82
- 6. It shows up in your bloodworkIt shows up in your bloodwork
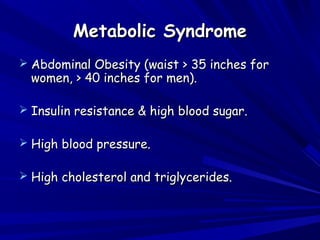
- 7. Metabolic SyndromeMetabolic Syndrome Abdominal Obesity (waist > 35 inches forAbdominal Obesity (waist > 35 inches for women, > 40 inches for men).women, > 40 inches for men). Insulin resistance & high blood sugar.Insulin resistance & high blood sugar. High blood pressure.High blood pressure. High cholesterol and triglycerides.High cholesterol and triglycerides.
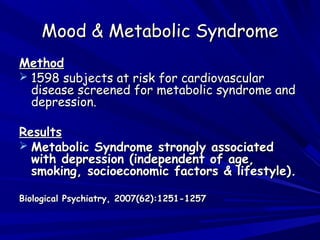
- 8. Mood & Metabolic SyndromeMood & Metabolic Syndrome MethodMethod 1598 subjects at risk for cardiovascular1598 subjects at risk for cardiovascular disease screened for metabolic syndrome anddisease screened for metabolic syndrome and depression.depression. ResultsResults Metabolic Syndrome strongly associatedMetabolic Syndrome strongly associated with depression (independent of age,with depression (independent of age, smoking, socioeconomic factors & lifestyle).smoking, socioeconomic factors & lifestyle). Biological Psychiatry, 2007(62):1251-1257Biological Psychiatry, 2007(62):1251-1257
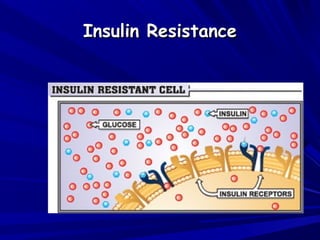
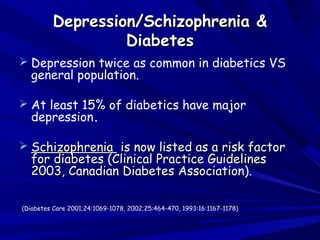
- 9. Depression/Schizophrenia &Depression/Schizophrenia & DiabetesDiabetes Depression twice as common in diabetics VS general population. At least 15% of diabetics have major depression. SchizophreniaSchizophrenia is now listed as a risk factoris now listed as a risk factor for diabetes (Clinical Practice Guidelinesfor diabetes (Clinical Practice Guidelines 2003, Canadian Diabetes Association).2003, Canadian Diabetes Association). (Diabetes Care 2001;24:1069-1078, 2002;25:464-470, 1993:16:1167-1178)
- 11. Glycemic Load and MoodGlycemic Load and Mood Method 42 healthy overweight subjects42 healthy overweight subjects Assigned to either a high or low glycemic load dietAssigned to either a high or low glycemic load diet for 6 months.for 6 months. Results Subjects on the high glycemic load diet experienced worsening mood over 6 months compared to subjects on the low glycemic load diet. Physiology & Behavior 98 (2009) 374-379Physiology & Behavior 98 (2009) 374-379
- 12. Carbohydrate Craving in Alcohol Dependence:Carbohydrate Craving in Alcohol Dependence: SubjectsSubjects 3 groups; a high carbohydrate craving (3 groups; a high carbohydrate craving (nn= 10), a low= 10), a low carbohydrate craving group (carbohydrate craving group (nn= 11), and a non-= 11), and a non- addicted control group (addicted control group (nn= 12).= 12). ResultsResults The carbohydrate-craving alcohol-dependentThe carbohydrate-craving alcohol-dependent subjects were uniquely sensitive to the adversesubjects were uniquely sensitive to the adverse effects of a diet high in refined carbohydrate (ieeffects of a diet high in refined carbohydrate (ie high glycemic load).high glycemic load). Moorhouse et al.Moorhouse et al. May 2000May 2000 Alcoholism: Clinical and Experimental ResearchAlcoholism: Clinical and Experimental Research Volume 24, Issue 5,Volume 24, Issue 5, pages 635–643,pages 635–643,
- 13. Low Glycemic Index (GI) FoodsLow Glycemic Index (GI) Foods Eating low Glycemic Index foods helps: Control your blood sugar levels. Control your cholesterol level. Control your appetite. Lower your risk of getting heart disease. Lower your risk of getting type 2 diabetes. Source: Canadian Diabetes Association 2008Source: Canadian Diabetes Association 2008
- 14. Mood & Omega 3 FatsMood & Omega 3 Fats Three main omega-3 fats:Three main omega-3 fats: EPA (fish fats)EPA (fish fats) DHA (fish fats)DHA (fish fats) ALA (vegetable oils, flax, nuts, leafyALA (vegetable oils, flax, nuts, leafy vegetables)vegetables)
- 15. Brain Cell Membranes are 2/3 Omega -3Brain Cell Membranes are 2/3 Omega -3 Fatty AcidsFatty Acids
- 16. EPA & DHAEPA & DHA Brain cell membranes rich inBrain cell membranes rich in DHADHA areare more fluid.more fluid. EPAEPA improves immune function and has aimproves immune function and has a protective effect in the brain.protective effect in the brain. Neuro-Signals (Neurosignals) 2009, 17(2):144-52Neuro-Signals (Neurosignals) 2009, 17(2):144-52
- 17. Mood & Omega-3 FatsMood & Omega-3 Fats MethodMethod Meta-analysis of 29 studies up to 2009Meta-analysis of 29 studies up to 2009 ResultsResults Evidence provides support for a benefit of Omega-3Evidence provides support for a benefit of Omega-3 fats in people with depressive illness.fats in people with depressive illness. Greatest benefits of Omega-3 fats were inGreatest benefits of Omega-3 fats were in individuals with more severe depression.individuals with more severe depression. American Journal of Clinical Nutrition, 2010, 91(3): 757-770American Journal of Clinical Nutrition, 2010, 91(3): 757-770
- 18. Mood, the Immune System &Mood, the Immune System & Celiac DiseaseCeliac Disease Celiac Disease (an autoimmune disease)Celiac Disease (an autoimmune disease) is positively associated with Depression.is positively associated with Depression. Ludvigsson et al. 2007, Celiac disease and risk of mood disorders.Ludvigsson et al. 2007, Celiac disease and risk of mood disorders. Journal of Affective DisordersJournal of Affective Disorders
- 19. Mood & Celiac DiseaseMood & Celiac Disease Treatment of Celiac Disease with a gluten-Treatment of Celiac Disease with a gluten- free diet is associated with improved mood.free diet is associated with improved mood. Neurological Science 2003, 24: 311-317.Neurological Science 2003, 24: 311-317. The Journal of Postgraduate Medicine 2002The Journal of Postgraduate Medicine 2002
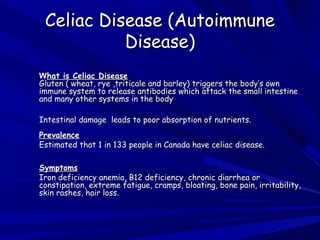
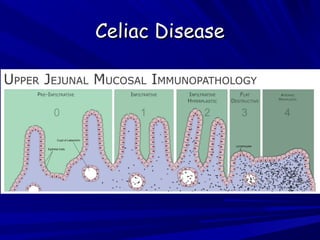
- 20. Celiac Disease (AutoimmuneCeliac Disease (Autoimmune Disease)Disease) WWhat is Celiac Diseasehat is Celiac Disease Gluten ( wheat, rye ,triticale and barley) triggers the body’s ownGluten ( wheat, rye ,triticale and barley) triggers the body’s own immune system to release antibodies which attack the small intestineimmune system to release antibodies which attack the small intestine and many other systems in the bodyand many other systems in the body Intestinal damage leads to poor absorption of nutrients.Intestinal damage leads to poor absorption of nutrients. PrevalencePrevalence Estimated that 1 in 133 people in Canada have celiac disease.Estimated that 1 in 133 people in Canada have celiac disease. SymptomsSymptoms Iron deficiency anemia, B12 deficiency, chronic diarrhea orIron deficiency anemia, B12 deficiency, chronic diarrhea or constipation, extreme fatigue, cramps, bloating, bone pain, irritability,constipation, extreme fatigue, cramps, bloating, bone pain, irritability, skin rashes, hair loss.skin rashes, hair loss.
- 22. National Institutes of Health, Consensus DevelopmentNational Institutes of Health, Consensus Development Conference Statement, Celiac Disease, August 2004.Conference Statement, Celiac Disease, August 2004. ““Define the relationship between celiacDefine the relationship between celiac disease, autoimmune disorders &disease, autoimmune disorders & neuropsychiatric disorders”.neuropsychiatric disorders”.
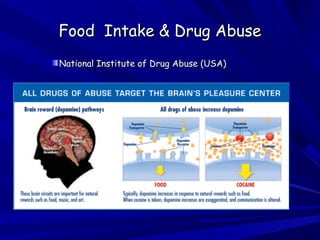
- 24. Food Intake & Drug AbuseFood Intake & Drug Abuse National Institute of Drug Abuse (USA)National Institute of Drug Abuse (USA)
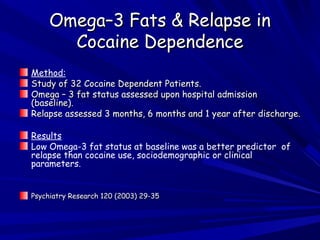
- 25. Omega–3 Fats & Relapse inOmega–3 Fats & Relapse in Cocaine DependenceCocaine Dependence Method: Study of 32 Cocaine Dependent Patients.Study of 32 Cocaine Dependent Patients. Omega – 3 fat status assessed upon hospital admissionOmega – 3 fat status assessed upon hospital admission (baseline).(baseline). Relapse assessed 3 months, 6 months and 1 year after discharge.Relapse assessed 3 months, 6 months and 1 year after discharge. Results Low Omega-3 fat status at baseline was a better predictor of relapse than cocaine use, sociodemographic or clinical parameters. Psychiatry Research 120 (2003) 29-35Psychiatry Research 120 (2003) 29-35
- 26. Triggers for Drug CravingTriggers for Drug Craving Alcoholics Anonymous & the HALT acronymAlcoholics Anonymous & the HALT acronym HH ungerunger AA ngernger LL onelyonely TT iredired
- 27. Digestive Tract & Pleasure/SurvivalDigestive Tract & Pleasure/Survival Center in the BrainCenter in the Brain
- 28. Food Restriction & Drug CravingFood Restriction & Drug Craving Alcoholics have elevated GHRELIN levels.Alcoholics have elevated GHRELIN levels. Elevated GHRELIN is positively correlatedElevated GHRELIN is positively correlated with intensity of alcohol craving in alcoholism.with intensity of alcohol craving in alcoholism. Food restriction increases ghrelin levels, drugFood restriction increases ghrelin levels, drug craving & the rewarding effects of drugs.craving & the rewarding effects of drugs. Cabeza de Vaca et al. Food Restriction Enhances the CentralCabeza de Vaca et al. Food Restriction Enhances the Central Rewarding Effect of Abused Drugs. The Journal ofRewarding Effect of Abused Drugs. The Journal of Neuroscience 1998,18(18):7502-7510.Neuroscience 1998,18(18):7502-7510.
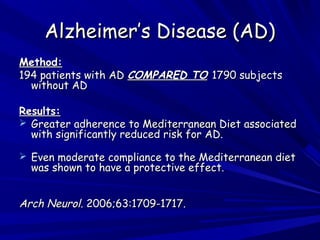
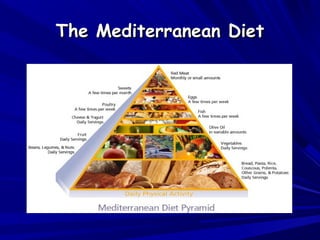
- 30. Alzheimer’s Disease (AD)Alzheimer’s Disease (AD) Method:Method: 194 patients with AD194 patients with AD COMPARED TOCOMPARED TO 1790 subjects1790 subjects without ADwithout AD Results:Results: Greater adherence to Mediterranean Diet associatedGreater adherence to Mediterranean Diet associated with significantly reduced risk for AD.with significantly reduced risk for AD. Even moderate compliance to the Mediterranean dietEven moderate compliance to the Mediterranean diet was shown to have a protective effect.was shown to have a protective effect. Arch Neurol.Arch Neurol. 2006;63:1709-1717. 2006;63:1709-1717.
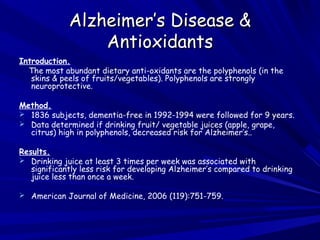
- 31. Alzheimer’s Disease &Alzheimer’s Disease & AntioxidantsAntioxidants Introduction. The most abundant dietary anti-oxidants are the polyphenols (in the skins & peels of fruits/vegetables). Polyphenols are strongly neuroprotective. Method. 1836 subjects, dementia-free in 1992-1994 were followed for 9 years. Data determined if drinking fruit/ vegetable juices (apple, grape, citrus) high in polyphenols, decreased risk for Alzheimer’s.. Results. Drinking juice at least 3 times per week was associated with significantly less risk for developing Alzheimer’s compared to drinking juice less than once a week. American Journal of Medicine, 2006 (119):751-759.
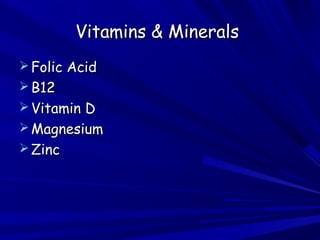
- 32. Vitamins & MineralsVitamins & Minerals Folic AcidFolic Acid B12B12 Vitamin DVitamin D MagnesiumMagnesium ZincZinc
- 33. Recommendations toRecommendations to Promote Mental HealthPromote Mental Health
- 34. Consider eating more like theConsider eating more like the Mediterraneans do.Mediterraneans do.
- 35. The Mediterranean DietThe Mediterranean Diet
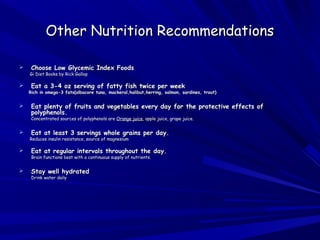
- 36. Other Nutrition RecommendationsOther Nutrition Recommendations Choose Low Glycemic Index FoodsChoose Low Glycemic Index Foods Gi Diet Books by Rick GallopGi Diet Books by Rick Gallop Eat a 3-4 oz serving of fatty fish twice per weekEat a 3-4 oz serving of fatty fish twice per week Rich in omega-3 fats(albacore tuna, mackeral,halibut,herring, salmon, sardines, trout)Rich in omega-3 fats(albacore tuna, mackeral,halibut,herring, salmon, sardines, trout) Eat plenty of fruits and vegetables every day for the protective effects ofEat plenty of fruits and vegetables every day for the protective effects of polyphenols.polyphenols. Concentrated sources of polyphenols areConcentrated sources of polyphenols are Orange juiceOrange juice, apple juice, grape juice., apple juice, grape juice. Eat at least 3 servings whole grains per day.Eat at least 3 servings whole grains per day. Reduces insulin resistance, source of magnesiumReduces insulin resistance, source of magnesium Eat at regular intervals throughout the day.Eat at regular intervals throughout the day. Brain functions best with a continuous supply of nutrients.Brain functions best with a continuous supply of nutrients. Stay well hydratedStay well hydrated Drink water dailyDrink water daily
- 37. Other RecommendationsOther Recommendations Aim for a healthy weight & a healthy waistAim for a healthy weight & a healthy waist circumferencecircumference (40” for men, 35” for women)(40” for men, 35” for women) Talk to your family doctor if you haveTalk to your family doctor if you have persistent gastrointestinal problems.persistent gastrointestinal problems. ExerciseExercise Improves mood, increases length of sobriety, improves insulinImproves mood, increases length of sobriety, improves insulin resistance, improves sleep and much more.resistance, improves sleep and much more.
- 40. Prevent Diabetes & Weight GainPrevent Diabetes & Weight Gain Start with “Big Volume, Small Calorie”Start with “Big Volume, Small Calorie” Foods.Foods. • Reduces appetite stimulating hormonesReduces appetite stimulating hormones produced in an empty stomach.produced in an empty stomach. • Eg. vegetable soups, salad, rawEg. vegetable soups, salad, raw vegetables, fruit.vegetables, fruit.
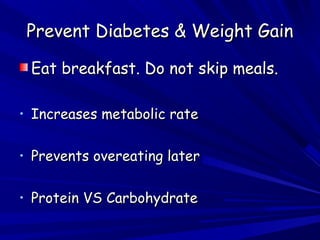
- 41. Prevent Diabetes & Weight GainPrevent Diabetes & Weight Gain Eat breakfast. Do not skip meals.Eat breakfast. Do not skip meals. • Increases metabolic rateIncreases metabolic rate • Prevents overeating laterPrevents overeating later • Protein VS CarbohydrateProtein VS Carbohydrate
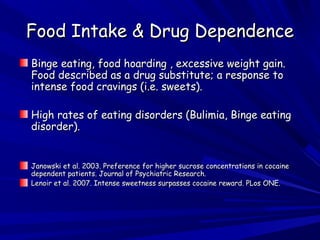
- 42. Food Intake & Drug DependenceFood Intake & Drug Dependence Binge eating, food hoarding , excessive weight gain.Binge eating, food hoarding , excessive weight gain. Food described as a drug substitute; a response toFood described as a drug substitute; a response to intense food cravings (i.e. sweets).intense food cravings (i.e. sweets). High rates of eating disorders (Bulimia, Binge eatingHigh rates of eating disorders (Bulimia, Binge eating disorder).disorder). Janowski et al. 2003. Preference for higher sucrose concentrations in cocaineJanowski et al. 2003. Preference for higher sucrose concentrations in cocaine dependent patients. Journal of Psychiatric Research.dependent patients. Journal of Psychiatric Research. Lenoir et al. 2007. Intense sweetness surpasses cocaine reward. PLos ONE.Lenoir et al. 2007. Intense sweetness surpasses cocaine reward. PLos ONE.
- 58. Nutrition & SobrietyNutrition & Sobriety Positive association between nutritionPositive association between nutrition education & drug abuse treatmenteducation & drug abuse treatment outcomes (Addiction Severity Index).outcomes (Addiction Severity Index). ROMHC Meadow Creek AddictionROMHC Meadow Creek Addiction Treatment Program includes NutritionTreatment Program includes Nutrition Education.Education. Grant LP et al. Nutrition Education is Positively Associated withGrant LP et al. Nutrition Education is Positively Associated with Substance Abuse Treatment Program Outcomes. Journal of theSubstance Abuse Treatment Program Outcomes. Journal of the American Dietetic Association 2004, 104: 604-610.American Dietetic Association 2004, 104: 604-610.
- 60. Liquids VS SolidsLiquids VS Solids • Liquids have little satiety value and canLiquids have little satiety value and can contain many calories.contain many calories. • Avoid fruit juices and eat the wholeAvoid fruit juices and eat the whole fresh fruit.fresh fruit. • Avoid soft drinksAvoid soft drinks
- 61. Try an Afternoon SnackTry an Afternoon Snack • Appetite usually starts to increase byAppetite usually starts to increase by late afternoon.late afternoon. • A mid afternoon snack containingA mid afternoon snack containing protein (eg yogurt, low fat cheese &protein (eg yogurt, low fat cheese & whole grain crackers etc.) can helpwhole grain crackers etc.) can help prevent hunger buildup.prevent hunger buildup.
- 62. ExerciseExercise
- 63. Emphasize FiberEmphasize Fiber • eg. whole fruits, whole vegetables,eg. whole fruits, whole vegetables, whole grains, legumes.whole grains, legumes. • Aim for 25 – 35 grams fiber per day.Aim for 25 – 35 grams fiber per day. • Creates a feeling of fullness.Creates a feeling of fullness.
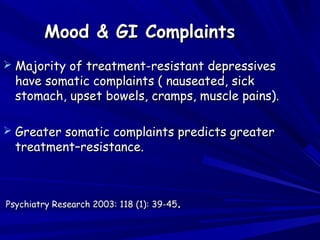
- 65. Mood & GI ComplaintsMood & GI Complaints Majority of treatment-resistant depressivesMajority of treatment-resistant depressives have somatic complaints ( nauseated, sickhave somatic complaints ( nauseated, sick stomach, upset bowels, cramps, muscle pains).stomach, upset bowels, cramps, muscle pains). Greater somatic complaints predicts greaterGreater somatic complaints predicts greater treatment–resistance.treatment–resistance. Psychiatry Research 2003: 118 (1): 39-45Psychiatry Research 2003: 118 (1): 39-45..
- 66. Mood & Immune SystemMood & Immune System Altered immune function may play a role inAltered immune function may play a role in the development of major depressionthe development of major depression.. Miller et al. Inflammation and Its Discontents; The Role ofMiller et al. Inflammation and Its Discontents; The Role of Cytokines in the Pathophysiology of Major Depression. BiologicalCytokines in the Pathophysiology of Major Depression. Biological Psychiatry 2009Psychiatry 2009
- 67. AcknowledgementsAcknowledgements Thank you to:Thank you to: Susannah Juteau M.Sc. (Nutrition)Susannah Juteau M.Sc. (Nutrition) Dietetic Intern McGill UniversityDietetic Intern McGill University For assisting in the research for thisFor assisting in the research for this presentation.presentation.
Editor's Notes
- Food restriction increases the rewarding and stimulating effects of drugs of abuse. Food restriction increases the rewarding and stimulating effects of drugs of abuse. Food Restriction as a stimulus for drug abuse.
- A huge topic and this is a very small sampling of the of the literature. Many topics and information I cannot possibly Cover in the limited time available.
- Depression may not be merely an emotional response to diabetic complications There may be a metabolic cause and effect relationship between depression and diabetes. Biological Psychiatry 2003, 54(3) 318-329 . Depression may not be merely an emotional response to diabetic complications. There may be a metabolic cause and effect relationship between depression and diabetes. Biological Psychiatry 2003, 54(3) 318-329 .
- Finnish subjects .Relationship between diabetes insulin resistance is not clearly understood. Is depression causing metabolic effects that are leading to insulin resistance or is insulin resistance causing impaired glucose metabolism in the brain leading to depression. Is insulin resistance the common factor i.e. leading eventually to both diabetes and depression. S Stress is a factor in depression and stress increases cortisol levels which in turn favors fat deposition in the abdominal area.
- Common in Schizophrenia and Depression
- Genetics, medications, lifestyle
- Randomized control trial Tufts University , Human nutrition Research center, School of Medicine, Boston All food provided
- Whenever I have a patient I have instructed to eat low GI and I suspect they’re not following my advice I look at ther bloodwork
- EPA and DHA are not efficiently synthesized in humans and therefore should be obtained directly from the diet particularly by consuming fish
- making which improves the flow of neurotransmitters important to mood (ie serotonin, dopamine, norepinephrine
- Updated systematic review and meta-analysis of the effects of n-3 long-chain polyunsaturated fatty acids on depressed mood. Appleton KM, Rogers PJ, Ness AR. School of Psychology, Queen's University, Belfast, UK. k.appleton@qub.ac.uk Comment in: Updated systematic review and meta-analysis of the effects of n-3 long-chain polyunsaturated fatty acids on depressed mood. Appleton KM, Rogers PJ, Ness AR. School of Psychology, Queen's University, Belfast, UK. k.appleton@qub.ac.uk Comment in:
- Common misdiagnoses are IBS, chronic fatigue syndrome, fibromyalgia
- as discussed membranes are 2/3 omega -3 fatsLow omega 3 fats play a role in aggression. Association between low omega 3 fats and aggression in cocaine addicts. (Drug and alcohol Dependence 2003.
- Data suggest but do not prove a causal relationship between n-6 or n-3 status and relapse potential in cocaine addiction
- Hormone in the stomach Ghrelin (appetite stimulant) increases as the stomach empties goes to the brain and stimu;ates appetite also goes to the VTA reward or pleasure center
- A case-control study nested within a community-based cohort in New York, NY. Columbia University Medical Center, 622 W 168th St; PH 19th floor; New York, NY 10032 ( [email_address] ). It is possible that diet is related to socioeconomic status or to other habits or characteristics related to better health and a lower risk for AD. Another explanation for our findings is that lower adherence to the MeDi could represent a consequence and not a cause of AD. Given the growing evidence for contribution of vascular risk factors in AD risk, vascular mechanisms are important to consider. 32 - 34 At the same time, there is strong evidence relating the MeDi to lower risk of vascular risk factors such as dyslipidemia, 5 - 6 hypertension, 3 , 5 - 7 abnormal glucose metabolism, 3 , 6 and coronary heart disease. 6 Second, the MeDi effect may be mediated by nonvascular mechanisms, such as oxidation or inflammation. Growing evidence implicates oxidative damage in the pathogenesis of AD 36 - 37 with neurons at risk for AD degeneration having increased lipid peroxidation, nitration, free carbony The association does not seem to be mediated by vascular comorbidity. This could be the result of either other biological mechanisms (oxidative or inflammatory) being implicated or measurement error of the vascular variables. the associations between MeDi and AD remain unchanged and significant even when simultaneously adjusting for the most commonly considered potential confounders for AD, such as age, sex, ethnicity, education, APOE genotype, caloric intake, and BMI. Higher adherence to MeDi reduced risk for probable AD either with or without coexisting stroke.
- Japanese Americans in King County, Washington Quercitin
- Screening for Eating Disorders at ROMHC & referral to Eating Disorders Clinic. Use of Tryptophan
- Topics include neurochemistry of addiction & role of nutrition in restoring normal brain function, hypoglycemia, effects of food restriction upon drug craving, how to control appetite, meal planning etc.