International Journal of COPD
Dovepress
open access to scientific and medical research
ORIGInAL RESEARCH
Open Access Full Text Article
Inspiratory drive is related to dynamic pulmonary
hyperinlation in COPD patients
Diego Gatta 1
Marco Fredi 2
Giovanni Aliprandi 2
Laura Pini 1
Claudio Tantucci 1
1
Respiratory Medicine Unit,
Department of Medical and
Surgical Sciences, University of
Brescia, Brescia, Italy; 2Respiratory
Rehabilitation Unit, Hospital Domus
Salutis, Brescia, Italy
Background: Baseline high neuromuscular drive is present in chronic obstructive pulmonary
disease (COPD). In moderate-to-very severe COPD patients, both static and/or dynamic
pulmonary hyperinflation have been demonstrated at rest.
Aim: To assess the influence of dynamic hyperinflation on neuromuscular drive at rest.
Methods: We recruited 22 patients with severe-to-very severe COPD showing resting dynamic
pulmonary hyperinflation, as assessed by the baseline reduction of inspiratory capacity (IC)
(,80% of predicted). IC, occlusion pressure (P0.1), maximal inspiratory pressure (MIP), and their
ratio were measured at end-expiratory lung volume (EELV) before and after acute inhalation of
400 mcg of albuterol (metered-dose inhaler plus spacer). In these patients the bronchodilator
response was assessed also as lung volume changes.
Results: Only in COPD patients with a marked increase in IC (.12% of baseline and at least
200 mL) after bronchodilator, resting P0.1 showed a clinically significant decrease, despite the
EELV diminution (P , 0.001). MIP was augmented following EELV reduction and therefore
the P0.1/MIP ratio was markedly decreased (P , 0.001). In contrast, no changes in these indices
were found after bronchodilator in COPD patients with insignificant variations of IC. Breathing
pattern parameters did not vary in both sub-groups after albuterol.
Conclusion: Following bronchodilator, significant P0.1 decrease, MIP increase, and reduction
of the P0.1/MIP ratio were found only in COPD patients with a marked IC increase and these
changes were closely related. These findings suggest that bronchodilators, by decreasing dynamic
hyperinflation, may control exertional and/or chronic dyspnea partly through a reduction of
central neuromuscular drive.
Keywords: chronic obstructive pulmonary disease, control of breathing, inspiratory muscles,
dynamic hyperinflation, bronchodilators
Introduction
Correspondence: Claudio Tantucci
Medicina Interna I, University of Brescia,
Spedali Civili di Brescia P.zzale Spedali
Civili, 1 25123 Brescia, Italy
Tel +3 90 3039 8069
Fax +3 90 3039 8069
Email tantucci@med.unibs.it
submit your manuscript | www.dovepress.com
Dovepress
http://dx.doi.org/10.2147/COPD.S38320
In patients with moderate-to-severe chronic obstructive pulmonary disease (COPD),
parameters reflecting static and dynamic pulmonary hyperinflation (DH) such as endexpiratory lung volume (EELV) or inspiratory capacity (IC) correlate better than forced
expiratory volume in 1 second (FEV1) with chronic dyspnea,1 and progressive DH
is thought to be the main limiting factor of their exercise capacity because of related
intolerable breathlessness.2,3 In COPD patients, the occurrence of DH, either at rest
or during exercise, is thought to induce dyspnea mainly by causing neuromechanical
(or neuroventilatory) dissociation.3 However, a high inspiratory drive that is widely
documented in severe-to-very severe COPD5 might also contribute to increased dyspnea
in these patients.
International Journal of COPD 2013:8 169–173
© 2013 Gatta et al, publisher and licensee Dove Medical Press Ltd. This is an Open Access article
which permits unrestricted noncommercial use, provided the original work is properly cited.
169
�Dovepress
Gatta et al
By increasing the expiratory flow reserve at low lung
volumes, bronchodilators can reduce chronic and exertional
dyspnea essentially by decreasing baseline EELV (or increasing IC) in moderate-to-severe COPD patients6–8 with DH, and
better neuromechanical coupling is believed to be responsible
to a large extent for such improvement.9
The aim of the study was to assess whether the acute
reduction of resting DH possibly obtained by bronchodilator
administration could influence the neuromuscular inspiratory
drive and its ratio with the inspiratory muscles’ strength in
stable COPD patients with marked airflow obstruction.
Methods
We prospectively evaluated a cohort of stable severe to very
severe COPD outpatients with baseline IC values less than
80% of their predicted values, consecutively enrolled at the
Respiratory Rehabilitation Unit, Hospital Domus Salutis,
Brescia, Italy. The diagnosis of COPD was made according to the following criteria: (1) smoking history of more
than 20 pack-years and/or the presence of other known risk
factors for COPD; (2) baseline FEV1/vital capacity ratio
less than the 5th percentile of normal limits;10 (3) increase
of FEV1 less than 10% of the predicted value and less than
200 mL in absolute value after 400 mcg of inhaled albuterol
(metered-dose inhaler plus spacer); (4) no history or evidence of other diseases with chronic airflow obstruction such
as chronic asthma, bronchiectasis, constrictive bronchiolitis,
tuberculosis, and cystic fibrosis.
At least 24 hours after withdrawal of long-acting beta-2
agonists, short and long-acting anti-cholinergics, and slowrelease theophylline, in the absence of exacerbation in the
preceding 12 weeks, the patients underwent both in baseline
condition and 30 minutes after the inhalation of albuterol
(400 mcg by metered-dose inhaler plus spacer) pulmonary
function tests (spirometry, maximal flow/volume curve,
lung volumes by N2-multibreath wash-out test) (System
1070, Medical Graphics, St Paul, MN, USA), determination
of mouth pressure 100 milliseconds after the beginning of
quiet inspiration during airways occlusion (P0.1) performed
at EELV, and measurements of maximal inspiratory pressure (MIP) at EELV during a Muller maneuver (Resp Mech
module, Medical Graphics, St Paul, MN, USA). Both P0.1
and MIP were obtained in triplicate with adequate time
intervals among the different measurements and the values
used for analysis were the average of the two highest ones.
Subsequently, the patients were classified, according to the
IC changes after acutely inhaled albuterol, in volume nonresponders (increase of IC , 12% and 200 mL of baseline:
170
submit your manuscript | www.dovepress.com
Dovepress
group 1) and volume responders (increase of IC 12% and
200 mL of baseline: group 2).
All spirometric parameters were analyzed as percent
of predicted values.10 The IC predicted values were those
proposed by Tantucci et al.11 Predicted values of IC for
those patients aged less than 65 were obtained by backextrapolating the reference equations. The patients were
recruited and tested if able to correctly perform the pulmonary function tests according to the American Thoracic
Society guidelines.12 The study was approved by the Ethics
Committee of the Hospital “Spedali Civili” of Brescia and
each patient signed an informed consent for collection and
treatment of data.
Statistical analysis
Differences between groups were assessed according to an
unpaired nonparametric test (Mann-Whitney test) while comparisons of functional parameters before and after albuterol
within groups were performed by a paired nonparametric test
(Wilcoxon test). The Pearson’s linear correlations were used
to establish association between the variables of interest and
the determination coefficients were also given. A P-value
less than 0.05 was considered as statistically significant.
The calculations were made using the SPSS 14.0 statistical
package (IBM Corporation, Armonk, NY, USA). Data were
expressed as mean ± standard deviation.
Results
Twenty-two COPD patients (18 male) with a mean age of
72 ± 6 years and FEV1 equal to 0.78 ± 0.26 L (33% ± 11%
predicted) were studied. Their anthropometric and functional
characteristics are shown in Table 1. At baseline, a severe
reduction of FEV1 with a marked increase of residual volume
and functional residual capacity and reduction of IC were
observed in these patients who exhibited, as expected, high
values of P0.1.
No significant differences, however, were found at rest
for spirometric parameters, lung volumes, neuromuscular
drive, and maximal isometric force of inspiratory muscles
between volume non-responders (group 1: increase of
IC , 12% and 200 mL of baseline) and volume responders
(group 2: increase of IC 12% and 200 mL of baseline)
(Table 1).
Following inhalation of albuterol, FEV1 increased by
50 ± 50 mL (from 0.87 ± 0.25 L to 0.92 ± 0.22 L) in group 1 and
by 130 ± 70 mL (from 0.74 ± 0.27 L to 0.87 ± 0.28 L) in group 2.
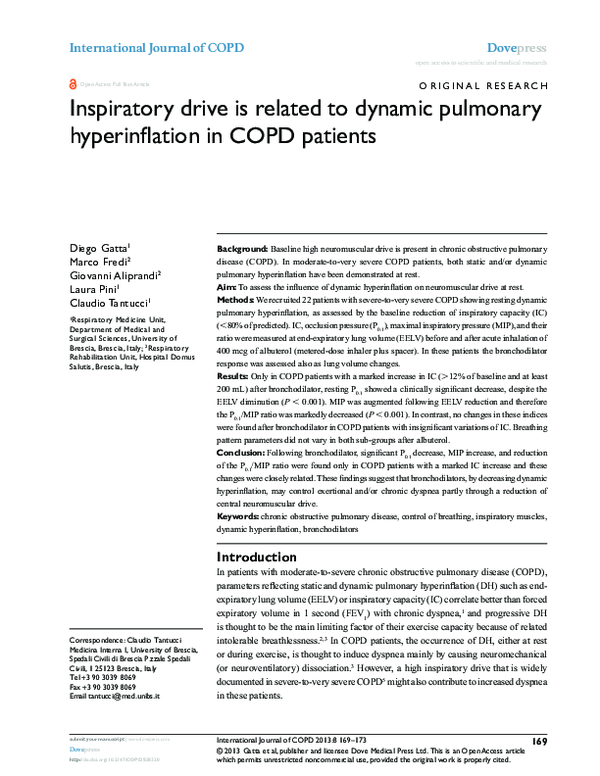
P0.1, MIP, and their ratio (P0.1/MIP%) are displayed in
Table 2, before and after albuterol for all patients and those
International Journal of COPD 2013:8
�Inspiratory drive and dynamic hyperinlation in COPD
Dovepress
neuromuscular drive at rest (r2 = 0.59; P , 0.01). A similar
relationship was found between changes in IC (as a percentage of baseline) and P0.1/MIP% ratio, as shown in Figure 1,
panel B (r2 = 0.56; P , 0.01). No variations of the breathing
pattern parameters such as tidal volume (Vt), respiratory rate
(RR), inspiratory (Ti) and expiratory time (Te), mean inspiratory flow (VT/Ti), and duty cycle (Ti/Ttot) were observed
before and after albuterol administration in both groups of
COPD patients.
Table 1 Anthropometric and functional characteristics observed
in all patients and two groups of them, divided according to the
absence (n = 7) or presence (n = 15) of signiicant change of
IC (.12% from baseline and 200 mL) after acute bronchodilator
at rest
n
Age (year)
Gender (M/F)
Smoke exposure
(pack years)
SVC (% pred)
FEV1 (% pred)
FVC (% pred)
FEV1/FVC %
IC (% pred)
RV (% pred)
TLC (% pred)
P0.1 (cm H2O)
MIP (cm H2O)
PaO2 (mmHg)
PaCO2 (mmHg)
22
68 ± 8
18/4
45 ± 22
7
71 ± 6
7/0
43 ± 20
15
66 ± 10
11/4
46 ± 23
ns
/
ns
78 ± 20
33 ± 10
74 ± 19
35 ± 9
55 ± 18
190 ± 63
121 ± 24
4.7 ± 1.2
69 ± 19
66 ± 10
44 ± 5
77 ± 23
33 ± 9
73 ± 20
36 ± 12
59 ± 27
183 ± 60
115 ± 23
4.2 ± 0.5
78 ± 20
64 ± 7
42 ± 7
79 ± 20
33 ± 11
74 ± 19
34 ± 7
54 ± 14
193 ± 67
124 ± 25
4.9 ± 1.4
65 ± 18
67 ± 11
45 ± 6
ns
ns
ns
ns
ns
ns
ns
ns
ns
ns
ns
Discussion
The results of this study indicate that in stable COPD patients
at rest the neuromuscular output to inspiratory muscles
is related to the degree of pulmonary hyperinflation and
the reduction of DH possibly achieved by bronchodilator
induces a significant decrease of inspiratory drive. Since
bronchodilators have been shown to limit exertional and
chronic dyspnea in COPD mainly by decreasing DH, our
findings suggest that this may occur partly because of
reduction on central motor output to inspiratory muscles.
It has been demonstrated that COPD patients have a high
neural drive even at rest, as reflected by the increased baseline
P0.1.5 Many factors have been implicated to explain this
elevated motor command to inspiratory muscles. Included
among them are increased airflow resistance, abnormal gas
exchange, weak respiratory muscles, and high ventilatory
requirements.13
Much evidence has been collected showing that distressing breathlessness in moderate-to-severe COPD patients
is mostly linked to the occurrence of DH.3 The imbalance between the volume displacement and the muscular
effort required to achieve it, known as neuromechanical
or neuroventilatory dissociation, is thought to be the main
mechanism by which DH causes chronic and exertional
dyspnea in COPD.9 Other mechanisms, however, have been
invoked in COPD patients as able to generate dyspnea and
Note: Data are mean ± SD.
Abbreviations: IC, inspiratory capacity; SVC, slow vital capacity; FEV1, forced
expiratory volume in 1 second; FVC, forced vital capacity; RV, residual volume;
TLC, total lung capacity; P0.1, mouth pressure 100 milliseconds after the beginning
of quiet inspiration during airways occlusion; MIP, maximal inspiratory pressure; SD,
standard deviation.
with and without significant increase of IC (as a percentage
of baseline).
Despite the reduction of EELV as reflected by the increase
of IC, P0.1 was significantly reduced in volume responder
COPD patients (P , 0.001). Since MIP values increased
with decreasing EELV, P0.1/MIP% was markedly decreased
in volume responder COPD patients after albuterol. In contrast, marginal changes in P0.1 and no changes in MIP and
P0.1/MIP% were observed in volume non-responder COPD
patients after bronchodilator.
Changes in IC (as a percentage of baseline) and P0.1 following acute administration of albuterol are plotted in Figure 1,
panel A, showing a close direct correlation between reduction of DH (as reflected by the IC increase) and decreased
Table 2 Resting values of IC and P0.1, MIP, and their ratio before (Pre-Br) and after (Post-Br) acute administration of bronchodilator
P
ΔIC , 12% bas
n
IC (L)
ΔIC . 12% bas
P
Pre-Br
Post-Br
Pre-Br
Post-Br
7
7
15
15
1.77 ± 0.45
1.88 ± 0.48
1.30 ± 0.46
1.66 ± 0.49
,0.05
6±4
,0.001
ΔIC (% bas)
P0.1 (cm H2O)
30 ± 13
4.2 ± 0.5
4.0 ± 0.6
3.8 ± 1.4
,0.001
78 ± 20
79 ± 20
,0.05
ns
4.9 ± 1.4
MIP (cm H2O)
65 ± 18
70 ± 20
,0.01
P0.1/MIP%
5.5 ± 1.1
5.1 ± 1.1
ns
8.2 ± 3.0
5.8 ± 2.0
,0.01
Notes: Clinically signiicant improvement of P0.1 and MIP and P0.1/MIP ratio were observed only in COPD patients with signiicant increase in IC. Data are mean ± SD.
Abbreviations: IC, inspiratory capacity; P0.1, mouth pressure 100 millseconds after the beginning of quiet inspiration during airways occlusion; MIP, maximal inspiratory
pressure; COPD, chronic obstructive pulmonary disease; Pre-Br, pre-bronchodilator; Post-Br, post-bronchodilator; bas, baseline; SD, standard deviation.
International Journal of COPD 2013:8
submit your manuscript | www.dovepress.com
Dovepress
171
�Dovepress
Gatta et al
A
B
8
3
r2 = 0.56
P < 0.01
−∆ P0.1/MIP (%)
−∆ P0.1 (cm H2O)
r2 = 0.59
P < 0.01
2
1
0
−10
0
10
20
30
40
50
60
∆IC (% baseline)
6
4
2
0
−10
0
10
20
30
40
50
60
∆IC (% baseline)
Figure 1 Relationship between changes in IC and P0.1 (A) and P0.1/MIP% (B), following bronchodilator in groups of stable severe-to-very severe COPD patients at rest.
Note: The vertical lines indicate the threshold of a signiicant increase in IC.
Abbreviations: IC, inspiratory capacity; P0.1, mouth pressure 100 millseconds after the beginning of quiet inspiration during airways occlusion; MIP, maximal inspiratory
pressure; COPD, chronic obstructive pulmonary disease.
particularly an increased sense of work/effort following
stimuli such as increased ventilatory requirements, elevated
EELV, and a related increase in elastic inspiratory threshold
load due to intrinsic positive end-expiratory pressure.3,9,14
A high inspiratory neural drive, especially in the presence of functionally or intrinsically weakened inspiratory
muscles is in fact associated with a greater respiratory
effort.15
The neural pathways underlying the sense of work/effort
include corollary discharge from motor cortical and bulbar
centers16 and possibly multiple afferences from mechanical
and metabolic receptors of respiratory and skeletal muscles
to the sensory cortex that are believed to contribute to the
dyspnea sensation.13
In our work we showed a clear link between neuromuscular output level and severity of DH at rest in stable COPD
patients and the possibility of significantly reducing it when
an effective desufflation is achievable, in this case after
acute bronchodilator inhalation, as indicated by a marked
IC increase.
The effect on the reduction of respiratory drive observed
in COPD patients who significantly increase IC after bronchodilator is likely even greater than we have shown, given
the corresponding reduction in EELV that per se should
increase, not decrease P0.1 because of better force-length
relationship of the inspiratory muscles. In fact, although we
did not measure directly EELV, with the reasonable assumption that total lung capacity remains unchanged after acute
inhalation of albuterol, the IC variation specularly reflects
the EELV change.
172
submit your manuscript | www.dovepress.com
Dovepress
Therefore, the decrease of neuromuscular output at rest
in COPD patients after bronchodilating drugs may reflect
an effective desufflation in the absence of important FEV1
change also when the lung volumes and IC measurements
cannot be adequately performed.
Drugs or non-pharmacological interventions that are
effective in decreasing DH may diminish both the degree of
neuromuscular uncoupling and the amount of neuromuscular
drive. It is conceivable that either mechanism can contribute
to reduce chronic and exertional dyspnea in COPD.
Finally, our results could be useful to explain the wide
range of resting values of P0.1 observed in COPD patients
with apparently similar severity of airflow obstruction, as
measured by spirometry, taking into account the possible
effect of different degrees of pulmonary hyperinflation.
Some limits of the study need to be addressed. The
amount of neural drive is indirectly assessed by the P0.1 measurement at the mouth. The dynamically hyperinflated COPD
patients have some intrinsic positive end-expiratory pressure.
Thus, changes of esophageal P0.1 (that truly reflect the neuromuscular output) occur before those of mouth P0.1 and the
two measurements correspond only when the initial pressure
decay is linear, as it usually is. The inspiratory muscles in
COPD can be intrinsically weak (myopathy, sarcopenia,
etc) and P0.1 could be influenced by the force developed at
the beginning of inspiration, without carefully reflecting the
central neural drive. However, this seems unlikely because
early (the first 100 milliseconds) contraction of inspiratory
muscles is not impaired under these circumstances, as found
in several neuromuscular diseases.17,18
International Journal of COPD 2013:8
�Inspiratory drive and dynamic hyperinlation in COPD
Dovepress
Although baseline parameters were not significantly
different between volume and non-volume responders, the
first group tends to be younger with more females, showing
slightly higher P0.1 and lower MIP. Since the sample size
is small, we cannot exclude that these differences could be
relevant when larger cohorts are examined.
In conclusion, a large P0.1 decrease, MIP increase, and
reduction of the P0.1/MIP ratio were found after bronchodilator only in COPD patients with a marked IC increase. More
interestingly, the improvement of DH and the decrease in
neuromuscular drive were closely related. These findings
indicate that decreasing DH by bronchodilators is associated with a reduction of the central neuromuscular drive
and effort/work related sensation, suggesting that corollary
discharge linked to an augmented central inspiratory output
is an adjunctive mechanism promoting dyspnea in COPD
patients with dynamic hyperinflation.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Eltayara L, Becklake MR, Volta CA, Milic-Emili J. Relationship
between chronic dyspnea and expiratory flow limitation in patients with
chronic obstructive pulmonary disease. Am J Respir Crit Care Med.
1996;154(6 Pt 1):1726–1734.
2. O’Donnell DE. Breathlessness in patients with chronic airflow limitation.
Mechanisms and management. Chest. 1994;106(3):904–912.
3. O’Donnell DE, Revill SM, Webb KA. Dynamic hyperinflation and
exercise intolerance in chronic obstructive pulmonary disease. Am J
Respir Crit Care Med. 2001;164(5):770–777.
4. Diaz O, Villafranca C, Ghezzo H, et al. Role of inspiratory capacity on
exercise tolerance in COPD patients with and without expiratory flow
limitation at rest. Eur Respir J. 2000;16(2):269–275.
5. Sorli J, Grassino A, Lorange G, Milic-Emili J. Control of breathing
in patients with chronic obstructive lung disease. Clin Sci Mol Med.
1978;54(3):295–304.
6. Tantucci C, Duguet A, Similowki T, Zelter M, Derenne JP, Milic
Emili J. Effect of salbutamol on dynamic hyperinflation in chronic
obstructive pulmonary disease patients. Eur Respir J. 1998;12(4):
799–804.
7. Boni E, Corda L, Franchini D, et al. Volume effectand exertional
dyspnea after bronchodilator in patients with COPD with and without
expiratory flow limitation at rest. Thorax. 2002;57(6):528–532.
8. O’Donnell DE, Voduc N, Fitzpatrick M, Webb KA. Effect of salmeterol
on the ventilatory response to exercise in chronic obstructive pulmonary
disease. Eur Respir J. 2004;24(1):86–94.
9. O’Donnell DE, Webb KA. Exertional breathlessness in patients with
chronic airflow limitation. The role of lung hyperinflation. Am Rev
Respir Dis. 1993;148(5):1351–1357.
10. [No authors listed]. Standardized lung function testing. Report working
party. Bull Eur Physiopathol Respir. 1983;19 Suppl 5:1–95.
11. Tantucci C, Pinelli V, Cossi S, et al. Reference values and repeatability
of inspiratory capacity for men and women aged 65–85. Resp Med.
2006;100(5):871–877.
12. [No authors listed]. Lung function testing: selection of reference values
and interpretative strategies. American Thoracic Society. Am Rev Respir
Dis. 1991;144(5):1202–1218.
13. Manning HL, Schwartzstein RM. Pathophysiology of dyspnea. New
Engl J Med. 1995;333:1547–1553.
14. Yan S. Sensation of inspiratory difficulty during inspiratory threshold
and hyperinflationary loadings. Effect of inspiratory muscle strength.
Am J Respir Crit Care Med. 1999;160(5 Pt 1):1544–1549.
15. O’Connell JM, Campbell AH. Respiratory mechanics in airways
obstruction associated with inspiratory dyspnea. Thorax. 1976;31(6):
669–677.
16. McCloskey DI. Corollary discharges: motor commands and
perception. In: Brookhart JM, Mountcastle VB, editors. Handbook of
Physiology Section 1 the Nervous System Volume I Cellular Biology
of Neurons, Part 2. Bethesda: American Physiology Society; 1981:
1415–1417.
17. Bégin R, Bureau MA, Lupien L, Lumieux B. Control of breathing in
Duchenne’s muscular dystrophy. Am J Med. 1980;69(2):227–234.
18. Tantucci C, Massucci M, Piperno R, Betti L, Grassi V, Sorbini CA.
Control of breathing and respiratory muscle strength in patients with
multiple sclerosis. Chest. 1994;105(4):1163–1170.
International Journal of COPD
Dovepress
Publish your work in this journal
The International Journal of COPD is an international, peer-reviewed
journal of therapeutics and pharmacology focusing on concise rapid
reporting of clinical studies and reviews in COPD. Special focus is given
to the pathophysiological processes underlying the disease, intervention
programs, patient focused education, and self management protocols.
This journal is indexed on PubMed Central, MedLine and CAS. The
manuscript management system is completely online and includes a
very quick and fair peer-review system, which is all easy to use. Visit
http://www.dovepress.com/testimonials.php to read real quotes from
published authors.
Submit your manuscript here: http://www.dovepress.com/international-journal-of-copd-journal
International Journal of COPD 2013:8
submit your manuscript | www.dovepress.com
Dovepress
173
�
 Marco Fredi
Marco Fredi Laura Pini
Laura Pini