J Gastrointest Surg (2007) 11:1673–1679
DOI 10.1007/s11605-007-0341-6
Surgical Management of Gastro–Gastric Fistula
After Divided Laparoscopic Roux-en-Y Gastric Bypass
for Morbid Obesity
O. N. Tucker & S. Szomstein & R. J. Rosenthal
Received: 23 July 2007 / Accepted: 11 September 2007 / Published online: 3 October 2007
# 2007 The Society for Surgery of the Alimentary Tract
Abstract
Background Gastro–gastric fistula (GGF) formation is uncommon after divided laparoscopic Roux-en-Y gastric bypass
(LRYGB) for morbid obesity. Optimal surgical management remains controversial.
Methods A retrospective review was performed of a prospectively maintained database of patients undergoing LRYGB
from January 2001 to October 2006.
Results Of 1,763 primary procedures, 27 patients (1.5%) developed a GGF and 10 (37%) resolved with medical
management, whereas 17 (63%) required surgical intervention. An additional seven patients requiring surgical intervention
for GGF after RYGB were referred from another institution. Indications for surgery included weight regain, recurrent, or
non-healing gastrojejunal anastomotic (GJA) ulceration with persistent abdominal pain and/or hemorrhage, and/or recurrent
GJA stricture. Remnant gastrectomy with GGF excision or exclusion was performed in 23 patients (96%) with an average
in-hospital stay of 7.5 days (range, 3–27). Morbidity in six patients (25%) was caused by pneumonia, n=2; wound
infection, n=2; staple-line bleed, n=1; and subcapsular splenic hematoma, n=1. There were no mortalities. Complete
resolution of symptoms and associated ulceration was seen in the majority of patients.
Conclusion Although uncommon, GGF formation can complicate divided LRYGB. Laparoscopic remnant gastrectomy
with fistula excision or exclusion can be used to effectively manage symptomatic patients who fail to respond to
conservative measures.
Keywords Complications . Roux-en-Y gastric bypass .
Morbid obesity . Fistula . Remnant gastrectomy
Abbreviations
AA
antecolic antegastric
BMI
body mass index
CT
computed tomography
GE
gastroesophageal
GUGI
GGF
EGD
LRG
LRYGB
POD
PPI
RG
RR
RYGB
gastrograffin upper gastrointestinal study
gastro–gastric fistula
Esophagogastroduodenoscopy
laparoscopic remnant gastrectomy
laparoscopic Roux-en-Y gastric bypass
postoperative day
proton pump inhibitor
remnant gastrectomy
retrocolic retrogastric
Roux-en-Y gastric bypass
This paper was presented at the SSAT Poster Presentation session on
May 21st 2007 at the SSAT Annual Meeting at Digestive Disease
Week, Washington (poster ID M1590).
O. N. Tucker : S. Szomstein : R. J. Rosenthal (*)
The Bariatric Institute and Division of Minimally Invasive
Surgery, Cleveland Clinic Florida,
2950 Cleveland Clinic Blvd.,
Weston, FL 33331, USA
e-mail: rosentr@ccf.org
Introduction
Surgery is the preferred technique to achieve weight loss
and resolution of comorbidity in the morbidly obese.1
However, surgery is not without its complications, and a
�1674
wide variety of approaches have been developed over the
last three decades in an attempt to reduce morbidity and
improve outcome. Laparoscopic Roux-en-Y gastric bypass
(LRYGB) is currently the most commonly performed
bariatric procedure worldwide.2–6 Despite advances in
technology and improvements in surgical technique, adverse events contributing to serious morbidity and mortality
are seen after LRYGB. Fistula formation is an uncommon
but potentially significant complication. The most common
type encountered is a gastro–gastric fistula (GGF) with an
abnormal communication between the gastric pouch and
the excluded stomach, which can result in failure of weight
loss, weight regain, intractable marginal ulceration with
recurrent upper gastrointestinal hemorrhage, pain, and
stricture formation.
Historically, the technique of gastroplasty, its subsequent
modification to the vertical banded gastroplasty, and the
early open RYGB procedures involved the creation of a
non-divided or partially divided gastric pouch.7–9 GGF
rates of 49% were reported after primary RYGB when the
pouch and stomach were stapled in continuity or partially
divided.10 Following complete transection of the gastric
segments, Capella and Capella10 reported a significant
reduction in the incidence of GGF to 2.6%, with further
reduction with the use of jejunal limb interposition.11 These
surgical techniques minimize the incidence of GGF
formation but do not eliminate it. GGF continue to occur
with a reported incidence of up to 6%.10,12,13 We have
previously reported a 1.2% incidence of GGF in our series
of patients after divided LRYGB.14
The optimal management of GGF remains controversial,
and reports of surgical treatment of this complication are
infrequent.10,12,15 We wished to determine the incidence of
GGF in our patient population of 1,763 morbidly obese
patients who underwent primary divided LRYGB to
determine the indications for intervention and to evaluate
a novel surgical approach to symptomatic GGF. We present
our results on laparoscopic remnant gastrectomy (LRG) with
tract excision or exclusion without interference with the
gastrojejunostomy in the management of patients with
symptomatic GGF after LRYGB.
Methods
Review of a prospectively maintained database and medical
records of consecutive patients undergoing primary
LRYGB from January 2001 to October 2006 was undertaken. All procedures were performed by two surgeons (S.
S. and R.J.R.) in accordance with the National Institute of
Health consensus criteria.16 Study permission was obtained
from the Institutional Review Board. All patients had a
Gastrograffin upper gastrointestinal study (GUGI) on
J Gastrointest Surg (2007) 11:1673–1679
postoperative day (POD) 1, and oral intake commenced if
normal. Patients were discharged on POD 2 to 4 on a
3-month course of a proton pump inhibitor (PPI). Patients
were reviewed at 2 weeks, 2 and 6 months, and yearly
thereafter. All data including demographic data, weight,
body mass index (BMI), co-morbidities, prior surgery,
reason for revision, complications, and outcome, including
mortality, morbidity, readmission rate, and weight loss,
were analyzed.
Surgical Technique of Laparoscopic Roux-en-Y Gastric
Bypass
A standard seven-trocar LRYGB was performed.17 A 15- to
20-ml pouch was created with a linear stapler with
reinforcement of the last three vertical firings with bovine
pericardial strips. A 50-cm biliopancreatic and >100-cm
antecolic antegastric (AA) alimentary limb determined by
BMI were fashioned. GJA and pouch staple-line integrity
was confirmed by air insufflation, methylene blue instillation, and esophagogastroduodenoscopy (EGD).
Diagnosis and Management of Patients with GGF
Patients with persistent nausea, vomiting, failure of weight
loss, weight regain, intractable GJA ulceration, persistent
epigastric pain, recurrent upper gastrointestinal hemorrhage,
and GJA stricture underwent surgeon-performed EGD,
GUGI, barium contrast study with supine and lateral
decubitus views, and/or double contrast abdominal CT
(Fig. 1). All patients with a GGF were treated with a PPI
regardless of symptoms, with the addition of sucralfate for
concomitant marginal ulceration and/or stricture. Indications for surgery were failed medical management in a
symptomatic patient, weight regain with non-resolution of
comorbidity, recurrent or non-healing GJA ulceration with
persistent abdominal pain and/or hemorrhage, and recurrent
GJA stricture.
Surgical Technique of Laparoscopic Remnant Gastrectomy
Trocar site placement was identical to primary LRYGB.17
The greater curve vessels were divided to the GEJ, the
postgastric space entered with remnant mobilization, and a
window was created separating pouch and remnant. Intraoperative EGD was performed to delineate the fistula. The
distal antrum was transected with a linear stapler proximal
to the pylorus. The pouch was vertically transected medial
to the GGF over an Ewald tube with a linear stapler. In the
presence of a small pouch, the remnant was vertically
transected lateral to the GGF, leaving a narrow stomach
margin. All staple lines were over-sewn. Repeat EGD was
performed to confirm fistula excision or exclusion, fol-
�J Gastrointest Surg (2007) 11:1673–1679
1675
tectomy, appendicectomy and two previous caesarian
sections; the second, had a laparoscopic cholecystectomy
and bilateral tubal ligation; and the third, had a total
abdominal hysterectomy with bilateral salpingoophorectomy. Concomitant surgery was performed at the time of
LRYGB in two patients, umbilical hernia repair in one, and
laparoscopic cholecystectomy in the other. All procedures
were completed laparoscopically (100%). The mean length
of hospital stay was 3.7 days (range, 3–5). During followup, three patients (18%) developed acute cholecystitis
requiring laparoscopic cholecystectomy.
The indications for surgery were failure of medical
management in 17 (100%), weight regain in 9 (53%),
persistent epigastric pain in 10 (59%), vomiting in 5 (29%),
persistent GJA ulceration in 13 (76%) with significant
hemorrhage in 3 (18%), and non-resolving GJA stenosis in
8 (47%) patients (some patients had more than one
indication). Surgery was performed at a mean of
24.9 months after primary LRYGB (range, 4–57). LRG
was performed in all 17 patients and completed laparoscopically in 16 (94%). One patient required conversion
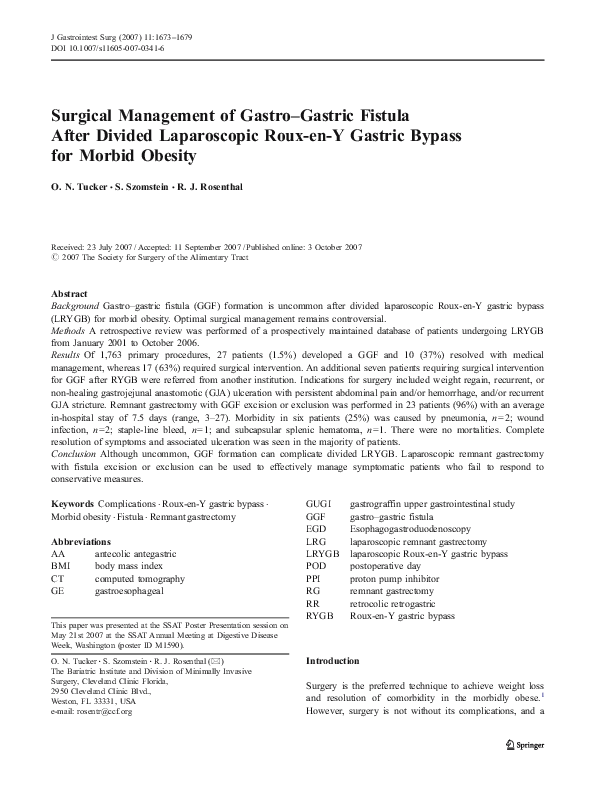
(6%) because of excess intraluminal air in the gastrointesFigure 1 Gastrograffin upper gastrointestinal contrast study demonstrating contrast extravasation from the lateral aspect of the gastric
pouch (P) through a fistulous tract (arrows) into the remnant stomach
(R) after laparoscopic Roux-en-Y gastric bypass; E esophagus.
lowed by air insufflation to check staple-line integrity. The
gastric remnant was extracted through the umbilicus.
Results
Over a 70-month period from January 2001 to October
2006, 1,763 patients underwent LRYGB for morbid
obesity. Of the 1,763 procedures performed, 27 patients
(1.5%) developed a GGF. All LRYGB procedures in these
27 patients were performed in a standard fashion with an
AA approach, and all were completed laparoscopically. All
27 patients were prescribed a treatment course of a PPI. In
addition, sucralfate was commenced in patients with
concomitant GJA ulceration and/or stenosis. Ten patients
(37%) with GGF after LRYGB responded to medical
treatment with symptom resolution. The remaining 17
patients (63%) had persistent symptoms despite maximum
medical treatment and required surgical intervention.
Of the 17 patients who required surgical intervention, the
majority were women with a male/female ratio of 1:5. At
the time of their primary LRYGB, their mean age was
42 years (range, 30–58), with a mean weight of 325 lb
(range 215–570), and a mean BMI of 49.7 kg/m2 (range,
35–61; Table 1). Three patients had a history of previous
abdominal surgery. One patient had a prior open cholecys-
Table 1 Patient Characteristics at Primary Laparoscopic Roux-en-Y
Gastric Bypass
Patients with gastro–gastric fistula requiring
surgery (n)
Gender (n)
Male
Female
Age (year)
Mean
Range
Weight (lb)
Mean
Range
BMI (kg/m2)
Mean
Range
Comorbidities (n)
Hypertension
Ischemic heart disease
Hyperlipidemia
Diabetes
Osteoarthritis
Chronic muscle and joint pain
Obstructive sleep apnoea
Gastroesophageal reflux
Deep venous thrombosis
Pulmonary embolus
Depression
Hypothyroidism
Others
Data in parentheses are percentages.
BMI Body mass index
17/27 (63%)
14 (82)
3 (18)
42
30–58
325
215–570
49.7
35–61
13 (76)
2 (12)
8 (47)
7 (41)
9 (53)
7 (41)
11 (65)
7 (41)
2 (12)
2 (12)
4 (23)
1 (6)
4 (23)
�1676
tinal tract after an intraoperative EGD. Remnant gastrectomy with pouch trimming and GGF excision was performed
in 12 patients (71%); four (23.5%) of these patients
required GJA excision and reanastomosis for stomal
obliteration secondary to longstanding marginal ulceration.
LRG without pouch trimming was performed in 5 patients
(29%) for exclusion of GGF. Five of 17 (29.4%) patients
developed early postoperative complications that delayed
discharge. One patient required 3 days of intravenous
antibiotics for a wound infection. A second patient
developed unexplained pyrexia, nausea, and tachycardia.
A GUGI and abdominal CT scan were normal with no
evidence of a leak or collection, and the patient responded
to conservative treatment. The third patient discharged
purulent fluid from his surgical drain on POD 7. An
anastomotic or staple-line leak was suspected, but a GUGI
and abdominal CT were entirely normal. He was discharged home on oral antibiotics with the drain in situ,
remained well, and the drain was subsequently removed in
the outpatient clinic. Hemorrhage from the gastric staple
line occurred in a single patient who was taking an oral
anticoagulant before surgery. This patient underwent an
urgent exploratory laparoscopy that required conversion to
an open approach to achieve hemostasis with over-sewing
of the pouch staple line. A fifth patient developed
pneumonia, which responded to oral antibiotics. The mean
length of stay for the 17 patients was 6.1 days (range,
3–10).
An additional seven patients were referred for surgery
from other centers with symptomatic GGF after open
RYGB in five (71%), and LRYGB in two (29%). Four
patients had a RYGB with GJA ring reinforcement (57%)
and two a non-divided RYGB with staple-line disruption
(28.5%). All patients were female. Incomplete data was
available for weight, BMI, and comorbidity at the time of
primary RYGB, and this data, was not included. The
patients presented for surgery at a mean of 7.8 years (range,
2–20) from the time of primary RYGB at a mean age of
42 years (range, 27–52). Indications for surgery were
intractable epigastric pain in four (57%), non-resolving
GJA stenosis in one (14%), recurrent GJA ulceration in
three (43%) with hemorrhage in one (14%), coexistent
jejuno–gastric fistula in one (14%), and vomiting in four
(57%). Six of the seven patients underwent RG (86%). The
remaining patient had a prior ring reinforcement of an open
retrocolic retrogastric (RR) RYGB. At laparotomy, pouch
outlet obstruction with ring erosion and GGF was evident.
The eroded ring was removed, the GJA was excised and
reanastomosed, the GGF transected, and a tube gastrostomy
inserted. LRG was attempted in four patients and completed
successfully in two (50%). An open approach was used in
the remaining two patients. Remnant gastrectomy with
pouch trimming and GGF excision was performed in five
J Gastrointest Surg (2007) 11:1673–1679
patients (71%). In four (57%) patients, the gastric bypass
was converted from a RR to an AA RYGB with excision
and reanastomosis of the GJA, and insertion of a tube
gastrostomy in addition to pouch trimming and GGF
excision. Remnant gastrectomy with GGF exclusion was
performed in one patient. In addition, an appendicectomy
was performed in one patient. Three complications were
observed, a subcapsular splenic hematoma, pneumonia, and
a superficial wound infection. The mean duration of
hospital stay was 9.4 days (range, 3–27).
Our incomplete follow-up is promising with symptom
resolution in the majority of patients (87%), resolution of
GGF and GJA ulceration in all 24 patients, and further
weight loss of an average of 27 lb in 21 patients (87%).
Four patients required surgical intervention for late
complications after LRG, including open adhesiolysis for
small bowel obstruction at 1 month, laparoscopic adhesiolysis for small bowel obstruction at 4 months, incarcerated
umbilical port site hernia repair at 13 months, and a
converted procedure for an internal hernia at the jejunojejunal anastomosis at 21 months.
Discussion
There are many factors responsible for GGF formation after
LRYGB (Table 2). Non-divided RYGB procedures have
been associated with an unacceptably high incidence of
GGF because of breakdown of the staple line with
reestablishment of continuity between the gastric segTable 2 Pathogenesis of Gastro–Gastric Fistula After Laparoscopic
Roux-en-Y Gastric Bypass
Description
Iatrogenic
Anastomotic Leak
Operation type
Marginal ulcer,
perforation
Foreign body erosion
Natural tendency
Poor surgical technique
Incomplete gastric transection
Pouch staple line disruption
Gastrojejunal anastomotic disruption
Coagulation injury
Ischemic necrosis due to foreign body:
VBG, LAGB
Incomplete gastric transection
Non-divided gastric bypass
Tissue ischemia
Staple migration
Use of non-absorbable suture material
Preanastomotic rings in banded gastric
bypass
Bovine pericardial strips
Natural gastric migration to reattach to the
remnant
LAGB Laparoscopic adjustable gastric banding, VBG vertical banded
gastroplasty
�J Gastrointest Surg (2007) 11:1673–1679
ments.10 In our series, two patients referred to us for
surgical management of symptomatic GGF from other
centers had a prior non-divided RYGB with staple-line
disruption (28.5%). Subsequent technical variations with
reinforcement of divided RYGB procedures with bands or
rings to increase restriction and prevent stomal and pouch
dilation were also plagued with a high incidence of
GGF.7,10 Intragastric migration of the band or ring with
erosion of the staple line was implicated in the evolution of
GGF in these procedures.7,10 Four of the patients referred to
us from other centers with symptomatic GGF had a prior
RYGB with GJA ring reinforcement (57%). At laparotomy,
two of the four rings had completely eroded through the
gastric staple line, whereas the other two were densely
adhered to the gastric wall. Ischemic necrosis because of
the presence of a constricting ring or band may have been
responsible for GGF in the latter two cases.
In the current era of divided RYGB, the majority of GGF
are caused by poor surgical technique with failure to
completely divide the stomach during pouch creation with
maintenance of continuity between the pouch and remnant.
Cucchi et al.13 reported a 6% incidence in divided gastric
bypass and recommended meticulous oversewing of staple
lines, careful anastomotic technique with good bites of
healthy tissue, avoidance of alimentary limb obstruction,
and intraoperative confirmation of GJA integrity using
methylene blue. Another common cause of GGF is an acute
leak from the GJA or the pouch staple-line disruption,
which is reported in up to 4.3% of patients after LRYGB.18
We have previously reported a 1.7% incidence of GJA leak,
of whom 27% subsequently developed a GGF.14 Malfunctioning of linear staplers can also occur, although this
complication has become uncommon with the advent of
more sophisticated devices.19 Various techniques have been
used to reduce the occurrence of pouch staple-line leak and
GGF, including jejunal and/or omental interposition, suture
reinforcement of the staple line, vapor-heated fibrin sealant,
and more recently, bovine pericardial strips.20–23
Figure 2 Schematic representation of a gastro–gastric fistula after
laparoscopic Roux-en-Y gastric bypass; GJA gastrojejunal anastomosis, GGF gastro–gastric fistula, HCL hydrochloric acid, P cells parietal
cells, G cells gastrin cells.
1677
Table 3 Surgical Management of Gastro–Gastric Fistula
n=24 patients
Remnant gastrectomy,
n=23 (96)
Additional procedures
Fistula transection,
n=1 (4)
Remnant gastrectomy with GGF excision,
n=9
Remnant gastrectomy with GGF exclusion,
n=6
Remnant gastrectomy with redo GJA,
n=8
Gastrostomy, n=4
Appendicectomy, n=1
Conversion from RR RYGB to AA RYGB,
n=4
Removal of eroded ring, GGF transection,
redo GJA, tube gastrostomy, n=1
Data in parentheses are percentages.
GGF Gastro–gastric fistula, RR retrocolic retrogastric, AA antecolic
antegastric, RYBG Roux-en-Y gastric bypass
In our series, the incidence of symptomatic GGF of 1.5%
after 1,763 primary LRYGB is relatively low compared to
other published series.13,15,24 Of these 27 patients, 37%
resolved without further intervention. We believe this is
because of standardization of our surgical approach to
LRYGB. At the beginning of the procedure, dissection
commences high on the gastric fundus to expose the angle
of His and the gastroesophageal junction. This exposure
allows the creation of a small lesser curve-based pouch and
ensures exclusion of the fundus with complete separation of
the gastric segments under direct vision. Incomplete
division of the apical portion of the stomach during pouch
construction can predispose to GGF formation.25 We
routinely perform a posterior wall stapled GJA and close
the anterior enterotomy in two layers with an absorbable
suture creating a narrow 1.5-cm outlet. To reduce the risk of
staple-line leak and hemorrhage, the lateral pouch staple
line is reinforced with bovine pericardial strips. The
integrity of the GJA and pouch staple line are then
confirmed by a combination of intraoperative EGD, air
insufflation, and methylene blue instillation. Non-absorbable suture use, staple migration, and tissue ischemia have
all been implicated in the development of stomal ulceration.10,14,24 Although peristrips could act as a foreign body
resulting in localized erosion and/or ulceration with
subsequent GGF formation, no cases have been recorded
in our series. We also use diathermy judiciously, as a
localized coagulation injury may predispose to GGF
formation. In our institution, we routinely perform GUGI
study on POD 1, facilitating the detection of acute leaks
and permitting early intervention.26
Persistent ulceration at the GJA predisposes to a
localized perforation and subsequent GGF formation. We
have previously reported a 4.2% incidence of marginal
ulceration after LRYGB, with a significant increase up to
�1678
53.3% in patients with a demonstrable GGF.14 To reduce
the risk of GJA ulceration, we preoperatively test and treat
patients positive for Helicobacter pylori. Eradication of H.
pylori has been demonstrated to significantly reduce the
incidence of marginal ulceration.27,28 Patients are also
encouraged to stop smoking. In addition, after LRYGB,
patients are discharged on a 3-month course of a PPI.29
A number of patients with symptomatic GGF will
respond to conservative management.30 The aim of medical
treatment is to attenuate the increased acid production in the
remnant stomach because of stimulation of parietal and
antral G-cells by food entering through the fistula (Fig. 2).
The acid from the remnant stomach spills over through the
fistula into the pouch and contributes to marginal ulceration
formation.31 Acid production, although significantly reduced, has been observed in the gastric pouch by
stimulation of residual parietal cells.32,33 PPI significantly
decrease acid production in the excluded gastric remnant. In
our unit, patients are commenced on a 6-week treatment
course of a PPI, with the addition of sucralfate in the
presence of marginal ulceration. Sucralfate provides a
protective barrier to the gastric pouch and jejunal mucosa,
reducing damage by refluxed acid from the remnant
stomach through the GGF.14,30 Patients are reevaluated
after 6 weeks to assess symptoms, and a repeat EGD is
performed. If patients fail to respond to maximal medical
therapy and develop GGF-related complications, surgery is
indicated. Currently, there is no accepted surgical technique
to manage symptomatic GGF. In our unit, we favor a LRG
with trimming of the gastric pouch and excision or
exclusion of the fistulous tract. This approach does not
interfere with the gastrojejunal anastomosis. In our series,
23 of 24 patients (96%) underwent a RG with GGF
excision in 74% and GGF exclusion in 26% (Table 3).
The pouch size determines the need for fistula excision or
exclusion. In the presence of an adequately sized small
pouch, we exclude the tract by vertical transection of the
gastric remnant just lateral to the fistula. To date, there has
been no evidence of ischemia of the narrow cuff of the
stomach left in situ lateral to the GGF. It is important to
excise as much of the antrum as possible to avoid the
creation of a retained antrum and the theoretical risk of
hypergastrinemia. Therefore, the distal stomach is transected just proximal to the pylorus. Remnant gastrectomy
can be performed successfully by a laparoscopic approach in
the majority of patients. In our series, a laparoscopic
approach was attempted in 21 patients (91%) and completed
in 18 (78%). As expected, the conversion rate for remnant
gastrectomy was higher in patients referred from other
centers, the majority of whom had a primary open RYGB.
Excision of the GJA with reanastomosis is required in the
presence of significant marginal ulceration with stomal
stenosis or prior RYGB, where complete pouch revision is
J Gastrointest Surg (2007) 11:1673–1679
required. Eight patients (35%) in our series required excision
of the GJA with reanastomosis, of whom four (50%) were
converted from a RR to AA RYGB. After RG, adverse
events were observed in the early postoperative period in six
patients (25%), and our surgical reintervention rate was
4.1%. A leak was suspected in one patient but not proven,
and a second patient developed pyrexia of unknown origin.
No deaths were recorded in this series.
Conclusion
In summary, GGF formation can complicate divided LRYGB.
Asymptomatic GGF can be managed conservatively. There is
no standardized surgical treatment approach for symptomatic
GGF. Reports of surgical treatment for this complication are
rare. In this study, we present a novel surgical procedure to
treat GGF, which consists of a laparoscopic approach with
RG with or without trimming of the gastric pouch and/or
fistulous tract, while leaving the GJA intact in the majority of
patients. Based on our early experience, we recommend LRG
with fistula excision or exclusion as an effective option with a
low morbidity and no mortality in the management of
symptomatic GGF after LRYGB.
References
1. Maggard MA, Shugarman LR, Suttorp M, Maglione M, Sugerman
HJ, Livingston EH, Nguyen NT, Li Z, Mojica WA, Hilton L, Rhodes
S, Morton SC, Shekelle PG. Meta-analysis: surgical treatment of
obesity. Ann Intern Med 2005;142(7):547–559.
2. DeMaria EJ, Jamal MK. Surgical options for obesity. Gastroenterol
Clin North Am 2005;34(1):127–142.
3. Rosenthal RJ, Szomstein S, Kennedy CI, Soto FC, Zundel N.
Laparoscopic surgery for morbid obesity: 1,001 consecutive
Bariatric operations performed at The Bariatric Institute,
Cleveland Clinic Florida. Obes Surg 2006;16(2):119–124.
4. Cottam DR, Nguyen NT, Eid GM, Schauer PR. The impact of
laparoscopy on Bariatric surgery. Surg Endosc 2005;19(5):621–627.
5. Nguyen NT, Silver M, Robinson M, Needleman B, Hartley G,
Cooney R, Catalano R, Dostal J, Sama D, Blankenship J, Burg K,
Stemmer E, Wilson SE. Result of a national audit of Bariatric
surgery performed at academic centers: a 2004 University
HealthSystem Consortium Benchmarking Project. Arch Surg
2006;141(5):445–449.
6. Wittgrove AC, Clark GW. Laparoscopic gastric bypass, Roux-en-Y500 patients: technique and results, with 3–60 month follow-up.
Obes Surg 2000;10(3):233–239.
7. Gomez CA. Gastroplasty in morbid obesity. Surg Clin North Am
1979;59(6):1113–1120.
8. Mason EE. Vertical banded gastroplasty for obesity. Arch Surg
1982;117(5):701–706.
9. Mason EE, Doherty C, Cullen JJ, Scott D, Rodriguez EM, Maher JW.
Vertical gastroplasty: evolution of vertical banded gastroplasty.
World J Surg 1998;22(9):919–924.
10. Capella JF, Capella RF. Gastro–gastric fistulas and marginal ulcers
in gastric bypass procedures for weight reduction. Obes Surg
1999;9(1):22–27.
�J Gastrointest Surg (2007) 11:1673–1679
11. Fobi MA, Lee H, Igwe D, Jr, Stanczyk M, Tambi JN. Prospective
comparative evaluation of stapled versus transected silastic ring
gastric bypass: 6-year follow-up. Obes Surg 2001;11(1):18–24.
12. Stanczyk M, Deveney CW, Traxler SA, McConnell DB, Jobe BA,
O’Rourke RW. Gastro–gastric fistula in the era of divided
Roux-en-Y gastric bypass: strategies for prevention, diagnosis,
and management. Obes Surg 2006;16(3):359–364.
13. Cucchi SG, Pories WJ, MacDonald KG, Morgan EJ. Gastrogastric
fistulas. A complication of divided gastric bypass surgery. Ann
Surg 1995;221(4):387–391.
14. Carrodeguas L, Szomstein S, Soto F, Whipple O, Simpfendorfer
C, Gonzalvo JP, Villares A, Zundel N, Rosenthal R. Management
of gastrogastric fistulas after divided Roux-en-Y gastric bypass
surgery for morbid obesity: analysis of 1,292 consecutive patients
and review of literature. Surg Obes Relat Dis 2005;1(5):467–474.
15. Gumbs AA, Duffy AJ, Bell RL. Management of gastrogastric
fistula after laparoscopic Roux-en-Y gastric bypass. Surg Obes
Relat Dis 2006;2(2):117–121.
16. Gastrointestinal surgery for severe obesity. Consens Statement
1991;9(1):1–20.
17. Szomstein S. How we do it: laparoscopic Roux-en-Y gastric
bypass. Contemp Surg 2007;62(3):106–111.
18. Hamilton EC, Sims TL, Hamilton TT, Mullican MA, Jones DB,
Provost DA. Clinical predictors of leak after laparoscopic
Roux-en-Y gastric bypass for morbid obesity. Surg Endosc
2003;17(5):679–684.
19. Favretti F, Segato G, De MF, Pucciarelli S, Nitti D, Lise M.
Malfunctioning of linear staplers as a cause of gastro–gastric
fistula in vertical gastroplasty]. G Chir 1990;11(3):157–158.
20. Shikora SA, Kim JJ, Tarnoff ME. Reinforcing gastric staple-lines
with bovine pericardial strips may decrease the likelihood of
gastric leak after laparoscopic Roux-en-Y gastric bypass. Obes
Surg 2003;13(1):37–44.
21. Sapala JA, Wood MH, Schuhknecht MP. Anastomotic leak
prophylaxis using a vapor-heated fibrin sealant: report on 738
gastric bypass patients. Obes Surg 2004;14(1):35–42.
1679
22. Lee MG, Provost DA, Jones DB. Use of fibrin sealant in
laparoscopic gastric bypass for the morbidly obese. Obes Surg
2004;14(10):1321–1326.
23. Zorrilla PG, Salinas RJ, Salinas-Martinez AM. Vertical banded
gastroplasty–gastric bypass with and without the interposition of
jejunum: preliminary report. Obes Surg 1999;9(1):29–32.
24. Filho AJ, Kondo W, Nassif LS, Garcia MJ, Tirapelle RA, Dotti
CM. Gastrogastric fistula: a possible complication of Roux-en-Y
gastric bypass. JSLS 2006;10(3):326–331.
25. Gould JC, Garren MJ, Starling JR. Lessons learned from the first
100 cases in a new minimally invasive Bariatric surgery program.
Obes Surg 2004;14(5):618–625.
26. Sims TL, Mullican MA, Hamilton EC, Provost DA, Jones DB.
Routine upper gastrointestinal Gastrografin swallow after laparoscopic Roux-en-Y gastric bypass. Obes Surg 2003;13(1):66–72.
27. Rasmussen JJ, Fuller W, Ali MR. Marginal ulceration after
laparoscopic gastric bypass: an analysis of predisposing factors
in 260 patients. Surg Endosc 2007 19.
28. Carrodeguas L, Szomstein S, Zundel N, Lo ME, Rosenthal R.
Gastrojejunal anastomotic strictures following laparoscopic
Roux-en-Y gastric bypass surgery: analysis of 1291 patients.
Surg Obes Relat Dis 2006;2(2):92–97.
29. Gumbs AA, Duffy AJ, Bell RL. Incidence and management of
marginal ulceration after laparoscopic Roux-Y gastric bypass.
Surg Obes Relat Dis 2006;2(4):460–463.
30. Gustavsson S, Sundbom M. Excellent weight result after
Roux-en-Y gastric bypass in spite of gastro–gastric fistula. Obes
Surg 2003;13(3):457–459.
31. MacLean LD, Rhode BM, Nohr C, Katz S, McLean AP. Stomal
ulcer after gastric bypass. J Am Coll Surg 1997;185(1):1–7.
32. Siilin H, Wanders A, Gustavsson S, Sundbom M. The proximal
gastric pouch invariably contains acid-producing parietal cells in
Roux-en-Y gastric bypass. Obes Surg 2005;15(6):771–777.
33. Hedberg J, Hedenstrom H, Nilsson S, Sundbom M, Gustavsson S.
Role of gastric acid in stomal ulcer after gastric bypass. Obes Surg
2005;15(10):1375–1378.
�
 Olga Tucker
Olga Tucker