Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser.
Related Papers
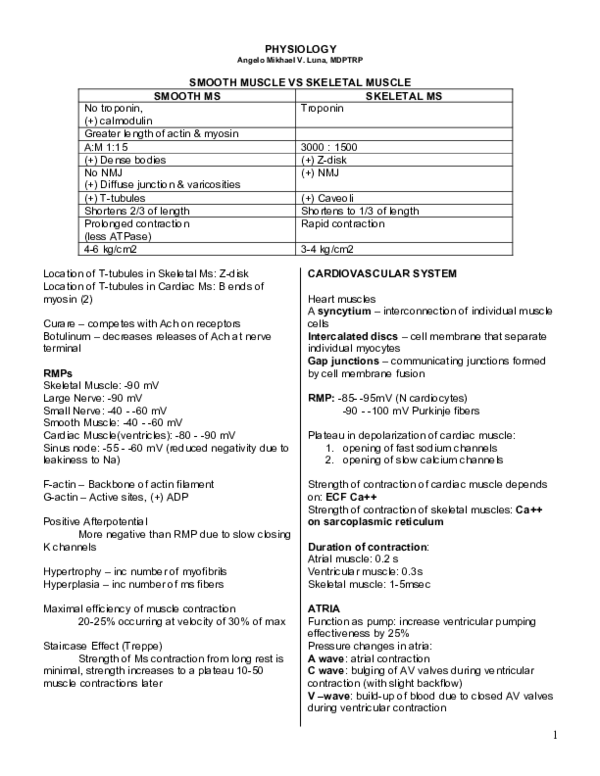
PHYSIOLOGY
Angelo Mikhael V. Luna, MDPTRP
SMOOTH MUSCLE VS SKELETAL MUSCLE
SMOOTH MS
SKELETAL MS
Troponin
No troponin,
(+) calmodulin
Greater length of actin & myosin
A:M 1:15
(+) Dense bodies
No NMJ
(+) Diffuse junction & varicosities
(+) T-tubules
Shortens 2/3 of length
Prolonged contraction
(less ATPase)
4-6 kg/cm2
Location of T-tubules in Skeletal Ms: Z-disk
Location of T-tubules in Cardiac Ms: B ends of
myosin (2)
Curare – competes with Ach on receptors
Botulinum – decreases releases of Ach at nerve
terminal
RMPs
Skeletal Muscle: -90 mV
Large Nerve: -90 mV
Small Nerve: -40 - -60 mV
Smooth Muscle: -40 - -60 mV
Cardiac Muscle(ventricles): -80 - -90 mV
Sinus node: -55 - -60 mV (reduced negativity due to
leakiness to Na)
F-actin – Backbone of actin filament
G-actin – Active sites, (+) ADP
Positive Afterpotential
More negative than RMP due to slow closing
K channels
Hypertrophy – inc number of myofibrils
Hyperplasia – inc number of ms fibers
Maximal efficiency of muscle contraction
20-25% occurring at velocity of 30% of max
Staircase Effect (Treppe)
Strength of Ms contraction from long rest is
minimal, strength increases to a plateau 10-50
muscle contractions later
3000 : 1500
(+) Z-disk
(+) NMJ
(+) Caveoli
Shortens to 1/3 of length
Rapid contraction
3-4 kg/cm2
CARDIOVASCULAR SYSTEM
Heart muscles
A syncytium – interconnection of individual muscle
cells
Intercalated discs – cell membrane that separate
individual myocytes
Gap junctions – communicating junctions formed
by cell membrane fusion
RMP: -85- -95mV (N cardiocytes)
-90 - -100 mV Purkinje fibers
Plateau in depolarization of cardiac muscle:
1. opening of fast sodium channels
2. opening of slow calcium channels
Strength of contraction of cardiac muscle depends
on: ECF Ca++
Strength of contraction of skeletal muscles: Ca++
on sarcoplasmic reticulum
Duration of contraction:
Atrial muscle: 0.2 s
Ventricular muscle: 0.3s
Skeletal muscle: 1-5msec
ATRIA
Function as pump: increase ventricular pumping
effectiveness by 25%
Pressure changes in atria:
A wave: atrial contraction
C wave: bulging of AV valves during ventricular
contraction (with slight backflow)
V –wave: build-up of blood due to closed AV valves
during ventricular contraction
1
VENTRICLES
Period of rapid filling – 1st 1/3 of diastole
Atrial contraction - last 1/3 of diastole
Period of isovolumic or isometric contraction
(+) ventricular contraction (-) emptying
Period of ejection
1st 1/3 – period of rapid ejection; 70% of
emptying
last 2/3 – period of slow ejection; 30 %
Period of isovolumic or isometric relaxation
End Diastolic volume
ventricular filling during diastole; 110-120ml
Strove volume output – systole; 70ml
End-systolic volume
remaining volume in ventricles; 40-50ml
Ejection fraction
fraction of end-diastolic volume that is
ejected; 60%
Heart sounds:
S1 – A-V valve closure
S2 – semilunar valve closure
S3 – rumbling into almost filled ventricle
S4 – atrial contraction
Preload – volume of blood remaining in ventricle at
end of diastole
Afterload – pressure in artery leading from ventricle
Main energy source for cardiac contraction:
Fatty acids
Substances with (+) Inotropic effect
1. caffeine – increases formation of cAMP
2. xanthene – same
3. Digitalis – inhibits Na-K ATPase
4. Glucagon – inhibits breakdown of cAMP
(-) Inotropic Effect
Hypoxia
Acidosis
Hypercapnea
B – blockers (blocks NE)
Cause of self-excitation of Sinus nodal fibers:
Inherent leakiness to sodium ions
Location of RBB and LBB
- endocardium
Location of Purkinje fibers
- 1/3 myocardium
Stokes Adam Syndrome – Complete AV block
causing faintness or death
- AV block causes development of new
pacemaker within the purkinje fibers of
the ventricle, with a delay by 5-30 sec.
during this time, the ventricle does not
contract and blood flow to brain becomes
insufficient
Control of heart rhythmicity and conduction by ANS
Parasympathetic – Acetylcholine – increases
permeability to POTASSIUM
Sympathetic – Norepinephrine – increase
permeability to Na++ & Ca++
Efficiency of cardiac contraction – 20 -25%
Effect of POTTASIUM in cardiac function
Excess K – dilated, flaccid, slow heart rate
Effect of Calcium Ions:
Excess Ca++ - spastic contraction
Deficiency Ca++ - flaccidity
Inc Temp: Inc HR
Dec Temp: Dec HR
Laplace law
Myocardial tension = intracavitary pressure x
ventricular radius
Frank-Starling mechanism
strerch on heart muscles by increased venous
return causes increased force of contraction by
bringing the actin and myosin to optimal degree of
interdigitation
- stretch of atria increases heart rate by
10-20%
Parasympathetic – decreases rate of rhythm of
sinus node
- decreases excitability of AV junctional
fibers
- (main control of SA node during rest)
Sympathetic – increases sinus rate
- increase rate of conduction and
excitability
- increase force of contraction
ECG PHYSIO
P wave – immediately before the beginning of
contraction of atria
QRS wave – immediately before the beginning of
ventricular contraction
T wave – ventricular repolarization
2
P-Q Interval (P-R interval)
beginning of contraction of atrium and
beginning of contraction of ventricle
Q-T Interval
duration of ventricular contraction (0.35s)
Einthoven’s Triangle – 2 arms and the LEFT leg
Einthoven’s Law – electrical potentials of any 2 of
the 3 bipolar limb is known, the 3rd one can be
determined mathematically by summing up the 2.
Most common cause of high voltage QRS
complexes
Hypetrophy of cardiac muscle
Conditions causing DECREASED voltage
Old myocardial infarction (cardiomyopathies)
Fluid in the pericardium
Pleural effusion
Pulmonary emphysema
Current of injury
Damage or injury to heart muscle itself, charge is
always negative
Conditions causing current of injury
Mechanical trauma
Infectious process
Ischemia (most common)
CIRCULATION
Systemic circulation – supplies all the tissues of the
body except LUNGS
Arterioles – act as control valves
Veins - major reservoir of blood; most distensible
Capillaries – largest cross-sectional area
Volumes of blood in different parts of circulation
Systemic veins – 84% of entire blood volume
Heart – 7%
Pulmonary vessels – 9%
Characteristic of blood flow in blood vessels
streamline or laminar flow – each layer of blood
remains in the same distance away from the wall;
central part of blood stays in the center of the vessel
Conditions causing Turbulent flow (blood flows
crosswise, forming whorls or eddy currents)
Blood flow is great
Obstruction
Sharp turn
Rough surface
Reynolds number – measures the tendency for
turbulence to occur
Resistance – impediment to blood flow in a vessel
Conductance – a measure of blood flow thru a
vessel for a given pressure difference
- reciprocal of resistance
- increases in proportion to 4th power of
the diameter
Poiseuille’s law – rate of blood flow is directly
proportional to the pressure difference & 4th power
of the radius; inversely proportional to length &
viscosity of blood
Major determinant of blood flow = diameter
Factors affecting blood viscosity in blood
vessels:
1. Hematocrit
2. Plasma proteins
3. Fahraeus-Lindqvist effect (smaller blood vessels
causes less viscosity because blood cells line up
and move singly)
4. Decreased velocity
5. Constrictions in blood vessels
Windkessel Effect: recoil of arteries during diastole
Ohm’s Law
Blood is directly proportional to pressure difference,
inversely proportional to resistance
Q= ∆P/R
Vascular distensibility:
fractional increase in volume for each mmHg rise in
pressure
Vascular compliance(capacitance) –
quantity of blood that can be stored for each mmHg
rise
Compliance = Distensibility x volume
Greater the compliance, slower velocity of
pulse pressure transmission
Blood flow
Quantity of blood that passes in a certain
point in a given time
2 major factors affecting pulse pressure
1. stroke volume
2. compliance (total distensibility)
Main control of Cardiac Output – Local tissue flow
3
Pulsus Paradoxus
Decreased stroke volume and pulse strength during
INSPIRATION
Increase dunring EXPIRATION
LYMPHATICS
Ausculatatory BP determination:
Accuracy is within 10% of values obtained by direct
arterial measurement
Areas in the body without lymphatic drainage
1. superficial portion of skin
2. CNS
3. deeper portion peripheral nerves
4. endomysium (muscle)
5. bones
Mean Arterial Pressure
Average of all pressures measured over time
Nearer to diastolic pressure ( 60%DBP + 40% SBP)
SBP + 2DBP/3 or DBP + 1/3 PP
Histologic characteristic of Lymphatics:
1. No basement membrane
2. No smooth muscle
Endothelial layer only
Pressure Reference level for Pressure
Measurement
At the level of TRICUSPID valve
Area where hydrostatic pressure changes due to
body positional changes does not affect pressure
measurement
Rate of lymph flow: 120 mL/hr
Sites of blood reservoirs
1. spleen (100 mL)
2. liver (several hundred mL)
3. large abdominal veins (300 mL)
4. venous plexus beneath the skin (several
hundred mL)
5. heart and lungs
Pores in the Capillary Membranes = Intercellular
clefts
1. Brain – (+) tight junction (BBB)
2. Liver – wide open
3. Glomerular tufts of kidney – (+) oval
windows or fenestrae
Vasomotion
Intermittent contraction of metarterioles and
precapillary sphincters
Most important regulator of opening or
closure: Oxygen in tissues
Capillary pressure – Moves fluid outward thru
capillaries
Interstitial fluid pressure – Inward
Plasma colloid osmotic pressure – inward
Interstitial fluid colloid osmotic pressure –
outward
Arterial end of capillaries – 13 mmHg filtration
pressure (outward)
Venous end of capillaries – 7 mmHg reabsorptive
pressure
Local Blood Flow Regulation
Vasodilator Theory
(release of vasodilator substance in
response to O2 deficiency)
Oxygen Demand Theory
(inc utilization of O2 due to inc metabolism)
Vasodilator Substances
Carbon dioxide
Hydrogen
Histamine
Lactic Acid
Adenosine (most important)
Adenosine PO4 cmpds
Potassium ions
Examples of Metabolic control of local blood
flow
Reactive Hyperemia
– increased blood flow to tissues after short
periods of vascular occlusion to repay accrued
oxygen deficit
Active Hyperemia
– increase blood flow to tissues during inc
activity due to release of vasodilator substances
Maintenance of blood flow in response to
arterial pressure changes
Metabolic Theory
– increases pressure FLUSHES vasodilator
substances, causes blood vessels to constrict
Myogenic Theory
– STRETCH of small blood vessels causes
smooth ms to conract
- proposed mechanism which protects
capillaries vs excessively high blood
pressures
4
Mechanism of Long term regulation of Blood
Flow
Change in degree of Vascularity
- Inc in pressure: increase size and
number of blood vessel
- Dec in pressure: decrease in size &
number of blood vessel
Humoral regulation of the circulation
Vasoconstrictors:
1. Vasopressin – most potent vasoconstrictor
substance
2. Angiotensin
3. NE
4. Epi
5. Serotonin (both vasodilator and
vasoconstrictor, which depends on site of
action)
Vasodilators
1. Bradykinin – both arteriolar dilation &
increased capillary permeability
2. Prostaglandin
3. Histamine
4. Serotonin
Ions:
Vasoconstrictor:
Calcium
Vasodilator:
Potassium
Magnesium
Sodium
Glucose
Acetate
Citrate
Hydrogen
Carbon dioxide
Nervous Regulation Of Circulation
Vasomotor Center
Reticular substance of medulla & lower 1/3 of pons
Lateral portions: inc HR & contractility
Medial portions: decrease HR
Vaoconstrictor area (C1)
Anterolateral upper medulla
Secretes NE- the sympathetic VC transmitter
substance
Vasodilator area (A1)
Anterolateral lower medulla
MOA: inhibits vasoconstrictor area
Sensory area (A2)
Tractus Solitarius (posterolateral medulla &
lower pons)
CN 9 & 10
Reflex control of circulation (both constrict & dilate)
Vasomotor tone
continues firing of sympathetic Vonstrictor
fibers
Sympathetic Vasodilator System
Anterior hypothalamus
Allows an anticipatory increase in blood flow
even before muscle activity (exercise)
Vasovagal syncope
Intense emotion
Activation of vasodilator system in anterior
hypothalamus
Vagal cardioinhibitory center in medulla
HR slows, BP falls
Reduced blood flow to brain
Most rapid mechanism of pressure control
- Nervous control of arterial pressure
Baroreceptor relexes
Carotid sinus – CN 9 via hering N; stimulate by
pressures >60 mmhg
Aortic arch – CN 10; stimulated by pressures
>30mmHg
Baroreceptor signals enter tractus solitarius of
medulla, where secondary signals inhibit
vasoconstrictor center & stimulate vagal center
Effects:
1. vasodilation of veins & arterioles
2. Dec HR & contractility (decreasing arterial
pressure, TPR, CO)
Chemoreceptors
Sensitive to O2 deficiency; CO2 & H excess
Hering N & Vagus
Excites vasomotor center, elevating arterial
pressure
Baroreceptor reflex – Inc blood volume to LV, Inc
HR on EXP
Bainbridge Reflex – Inc venous return to RA, Inc
HR on INSP; mediated by vagus N stimulated by
atrial stretch; prevents damming of veins in atria,
veins, pulmo circulation
CNS Ischemic response
Insufficient blood flow to brain causes rise in CO2,
stimulating SNS, elevating arterial pressure
One of the MOST powerful activator of sympathetic
vasoconstrictor system
“Last Ditch Stand” of pressure control mechanism
5
Cushing’s Reaction
Special type of CNS ischemic response, a
reaction to increased ICP
Inc BP, Dec HR, Dec RR
Protective response to maintain nutrition on
brain vital centers
Kidney’s dominant role in Long term regulation of
Arterial Pressure
Main determinant of ECF volume
- salt in the body
3. Hyperthyroid (inc metabolism, increasing
vasodilator products)
4. Anemia (reduced viscosity, dec O2 causing
vasodilation)
Conditions with DEC CO
Heart conditions (MI, myocarditis, cardiac
tamponade, valvular dse)
Dec. venous return (dec blood volume, venous
dilatation, obstruction of large arteries)
CORONARY CIRCULATION
RAA system
Renin – “enzyme” from JG cells in AFFerent
arterioles
- converts rennin substrate
(angiotensinogen) to angiotensin I
AI – AII – converted in endothelium of lung vessels
Primary controller of coronary flow
Myocardial oxygen demand (mvO2)
[Metabolic Factors]
AII
Coronary sinus – where most of LV blood drain
into
Anterior cardiac veins – where most of RV drain
Thebesian veins – minute blood vessels where
drains directly in the chambers
1. acts directly on kidneys (H2O & Na
retention)
2. stim adrenals- aldosterone (H20 & Na
rebsorption)
Goldblatt Hypertension
“one kidney” HPN
1st phase: vasoconstrictor type of HPN ( renninangiotensin sys)
2nd phase: volume-loading HPN (fluid retention)
HPN in coarctation of aorta
Blood in lower body is carried by collateral lood
vessels in body wall with increased vascular
resistance
Higher BP in upper part of body
Mechanism of higher BP similar with Goldblatt HPN
Left coronary A – supplies Ant & Lat LV
Right coronary A – most of RV & post LV
Sympathetics – NE, inc HR & contractility,
DILATES coronary arteries
Parasympathetics – Ach, dec HR & contractility,
CONSTRICTS coronaries
Epicardial coronary vessels – mostly ALPHA
receptors (constrictors)
Intramuscular coronary vessels – mostly BETA
receptors (dilators)
Coronary Ischemia > 30 minutes
- duration where relief of ischemia may be too late to
save lives of cardiac cells
CO AND VR AND REGULATION
BP = CO x TPR
CO = SV x HR
SV = PL x MC x AL
Primary controller of CO
- Venous Return (Frank-Starling Mech)
Conditions with INC CO
MC cause of elevated CO
- DEC. TPR
Other causes:
1. Beriberi (thiamine deficiency with resultant
peripheral vasodilation)
2. AV fistula
3 known causes of reduced renal output of urine
during cardiac failure
1. Dec GFR (due to dec arterial pressure &
sympathetic constriction of afferent arterioles)
2. Activation of rennin-angiotensin sys (inc
reabsorption of H2O & Na)
3. Inc Aldosterone secretion
Excess POTASSIUM – most powerful stimulus for
aldosterone secretion
Atrial Natriuretic Factor (ANF)
Hormone released by stretch of atrial walls
Direct effect on kidneys to increase EXCRETION of
Na & H2O
Help prevent extreme congestive symptoms of HF
6
Type of shock with increased viscosity
- Hypovolemic shock caused by plasma
loss (intestinal obstruction & severe burns)
Type of shock with increased temperature
- Septic shock
BLOOD
Amount of Hgb / 100 mL of blood
- 15mg/100mL of blood
Binding capacity of Hgb
- 1.34mL O2 / 1g of Hgb ( 1.39 if pure
Hgb)
Amount of O2 released from hemoglobin in the
tissues
5mL O2 / 1 dL of blood is transported into
tissues
Also 4 mL CO2 / dL of blood
Heme – mitochondria (kreb’s cycle)
Globin – ribosomes
Immediate precursor of Heme
Acetic acid (+) glycine
Acetic acid forms succinyl-coA thru kreb’s cycle
Succinyl coA (+) Glycine = Pyrrole
4 Pyrrole à Protoporphyrin IX
Protoporphyrin IX (+) Fe = Heme
1gm Hgb
= 4 Fe
= 4 O2 molecule
= 8 O2 atoms
Heme (+) a polypeptide forms Hgb Chain
2 alpha chain (+) 2 Beta chain = Hgb A
Sickle cell
Valine substituted for glutamic acid
(+) Hgb S, (+) AbN B-globin
Pernicious Anemia – Vit B12 deficiency
Sprue – Pteroylglutamic acid deficiency (Folate
deficiency)
Proerythroblast à Basophilic erythrocyte à
polychroatophilic à Orthochromatophilic à
Reticulocyte à Erythrocyte
Possible sources of Erythropoietin
Mesangial cells
Tubular epithelial cells
Stim by NE, Epi & PG
Life span of Reticulocytes
1-2 days
Half-lives:
Granulocytes (B, E, N)
4-8 hrs in blood; 4-5 days in tissues
Monocytes
10-20 hrs in blood; mos – years in tissues as
macrophages
Lymphocytes
(+) Recirculation; mos – years
Platelets
10 days
Lipases – seen only in macrophages
Pseudopodia – commonly seen only in Neutrophils
1st Line of Defense
Tissue macrophages
2nd Line of Defense
Neutrophils
3rd Line of Defense
Monocyte – macrophage
th
4 Line of Defense
Granulocyte – monocyte by bone marrow
Larvicidal agent of eosinophils
Major Basic Protein
Substance secreted by macrophages to promote
growth & reproduction of Lymphocyte
- IL – 1
Promotes growth & reproduction of virtually all types
of stem cells
- IL – 3
Activation of a clone of Lymphocyte
B-Lymphocyte – by Antigens
T- Lymphocytes – by surface receptor proteins (Tcell markers)
Mechanism by which Antibodies inactivate invading
agents
Precipitation – insoluble (tetanus toxin)
Lysis – rupture
Agglutination – clump (large particles : bacteria or
RBC)
Neutralization – cover active site of toxin
IgG – Bivalent (2), most abundant (75%)
IgM – 10 binding sites, (+) primary response
IgE – 10 binding sites, allergic rxn
7
COMPLEMENT SYSTEM
Chemotaxis – C5a
Opsonization – C3b
Lysis – C5b 6789
Anaphylaxis – C3a, C4a, C5a
Classical Complement
Ag- Ab complex – activates C1
Alternative Complement
response to large polysaccharide of
microorganism
Reacts with complement factors B & D,
which activates factor C3
Major stimulant of cytotoxic & suppressor T-cells
- IL – 2
Major stimulant of B-cell, plasma cells
- IL -4,5,6
Major stimulant of T-helper cells
- IL-2
Mechanism of action of cytotoxic (killer)T-cells
- forms perforins
Major regulator of all immune functions
- T – helper cells
Madiator of Immune tolerance
- Suppressor T-cells
Erythroblastosis Fetalis
Mother – Rh (-)
Father – Rh (+)
Baby – Rh(+)
In mismatch transfusion rection
The donor blood is the one hemolyzed,
clumped & agglutinized
Most Important antigens causing graft rejection
Class I HLA antigens
Class I HLA – all cells
Class II HLA – Lymphocyte
Class III HLA – Complement
BLOOD COAGULATION
Rate-limiting factor in coagulation of blood
- Prtothrombin activator
Difference between serum & plasma
- Serum has NO fibrinogen or clotting
factors
Actual Protease that split Prothrombin to thrombin
Activated Factor X (stuart factor)
CLOTTING FACTORS
I - Fibrinogen
II – Prothrombin
III – Tissue thromboplastin, tissue factor
IV – Calcium
V – Proaccelerin, Labile factor, Ac-globulin
VII – Proconvertin, stable factor, serum prothrombin
conversion accelerator
VIII – antihemophilic factor A, AHF, AHG
IX – Antihemophilic factor B, Christmas factor, PTC
X – Stuart Factor
XI – Antihemophilic factor C, PTA
XII – Hageman Factor
XIII – Fibrin-stabilizing factor
Prekalikrein – Fletcher
HMWK – Fletzgerald
EXTRINSIC PATHWAY
Tissue trauma
à Tissue thromboplastin (Lipoprotein +
phospholipids)
à Thromboplastin (+) Factor 7
à F10 – F10a
à F10 + F5 + phospholipid of thromboplastin
à Prothrombin activation
INTRINSIC PATHWAY
Blood Trauma
à F12 – F12a (+) PF3
à F11 – F11a (HMWK & prekalikrein)
à F9 – F9a
à F9a (+) F8 (+) PF3 (+) platelet phospholipids
à F10 – F10a
à F10 (+) F5
à Prothrombin activation
ALL reactions in Both Extrinsic & Intrinsic Pathway
requires Calcium EXCEPT
F12 activation
F11 activation
Factors that prevent clotting in Normal Blood
vessels
Smooth blood vessels
Glycocalyx in endothelium
Thrombomodulin
Inactivators of coagulation factors (Anticoagulants)
Protein C - F5, F8
Heparin & Antithrombin III – F9,10,11,12
Plasmin – F1,2,5,8,12
8
Heparin – activates antithrombin III
Warfarin – blocks Vit K
Basement membrane – mesangial cells (increases
surface area for filtration by inc slit pores
Functions similarly with antithrombin III but not
accelerated by heparin
- Alpha2 macroglobulin
Electronegativity of glomerular BM
- due to proteoglycans & protein
- repulses protein molecules larger than
69,000 MW
PT – Extrinsic (N: 12 mins)
aPTT – Intrinsic
BT – No. of platelets (N: 1-6 mins)
CT – Function of platelets (N: 6-10mins)
KIDNEYS AND BODY FLUIDS
Total body water:
Adult: 57% (40L)
NB: 75%
Daily Loss of Body Water
Sensible:
1. sweat – 100 mL
2. feces – 100 mL
3. urine – 1400 mL
Insensible:
1. skin – 300-400 mL
2. lungs – 300-400 mL
Cold weather: cold temp decreases atmospheric
vapor pressure, causing GREATER water loss
Major Ions
ECF:
1. chloride
2. bicarbonate
3. sodium
ICF:
1. Potassium
2. Phosphate
3. Moderate Mg & Sulfate
No Calcium ions
Greatest amount of anion in ECF – Cl
Greatest amount of anion in ICF – Protein
Characteristic of Nephrons
Cortical Nephrons – short loops of Henle
Juxtamedullary Nephrons – Long loops of Henle
Peritubular Capillaries – cortex – reabsorbs most
fluid
Vasa Recta – branch of pertubular capillaries that
extend to Medulla – concentrates urine
Glomerular filtrate
Same composition with plasma except:
No glucose
No protein
No RBC
Higher Cl & HCO3
Lower (+) ions
GFR – 125 L/min
180 L/day
Filtration fraction
Fraction of renal plasma flow that becomes
glomerular filtrate
1/5 or 19%
Renal fraction
Portion of cardiac output that passes to
kidneys
21%
Dynamics of Filtration (glomerular membrane)
Glomerular Pressure (promotes filtration)
Bowman’s capsule P – opposes
Colloid osmotic pressure of plasma proteins –
opposes
Colloid osmotic pressure in Bowman’s capsule –
promotes
Juxtaglomerular complex
Macula Densa – epithelial cells of distal tubules
Juxtaglomerular cells – smooth muscle cells of both
afferent & efferent arterioles, (+) renin
Autoregulation of GFR
AFFerent arteriolar vasoDILATION
low Na & Cl conc due to low GFR stimulates
macula densa to dilate afferents
Most important mechanism for
autoregulation
EFFerent arteriolar vasoCONSTRICTION
Low Na & Cl at macula densa cause JG cells
to release rennin, constrictor the more sensitive
efferents
Glomerular membrane
Endothelium – fenestrae
Epithelium – slit pores
9
URINE FORMATION
3 primary processes involved in urine formation
Filtration
Secretion
Reabsorption
PRIMARY ACTIVE TRANSPORT OF SODIUM
Basolateral side of tubular epithelium
(+) Na-K ATPase (3Na/2K)
Brush Border
(+) Na-carrier proteins that provide
facilitated-diffusion of Na
SECONDARY ACTIVE REABSORPTION FROM
TUBULES (CO-TRANSPORT)
Substances co-transported with Na:
Proximal Tubules- glucose, amino acids,
organic subst (acetoacetate, H20-sol vit)
Thick ascending Loop of H – chloride
Others- PO4, Mg, Ca, H
SECONDARY ACTIVE SECRETION INTO
TUBULES (COUNTERTRANSPORT)
(Proximal Tubules)
Hydrogen
K
Urate
PASSIVE ABSORPTION OF H2O – Osmosis
PASSIVE ABSORPTION OF Cl& UREA – Diffusion
ABSORPTIVE CAPABILITIES OF DIFFERENT
TUBULE SEGMENTS
Proximal Tubule
Co-Transport & Countertransport, Majority of
reabsorption (65%)
Thin Loop
H2O permeable only
Thick Loop
H20 & Urea IMpermeable
Concentrating function
Early half of Distal Tubule
“Diluting Segment”
H20 & Urea IMpermeable
Late Distal Tubule & Cortical Collecting Duct
IMpermeable to Urea
Aldosterone Fxns (Na, K)
ADH Fxns (H20)
(+)Brown cells aka intercalated cells –
secretes H by 1o active secretion
(+) Acidification fxn
Collecting Duct
ADH fxns
H secretion
(+) Acidification fxn
Late Distal Tubule
(+) intercalated cells – H secretion
(+) Principal cells – Na reabsorption & K
secretion
Special Mechanism of Absorption of Protein in
Proximal Tubules
Pinocytosis
Inulin
Neither secreted nor reabsorbed
Measures GFR (125 mL/min)
Para-aminohippuric acid (PAH)
Secreted but not reabsorbed
Measures plasma flow thru kidneys (650mL)
Countercurrent multiplier
Repetitive reabsorption of NaCl by THICK
ascending limb
Contercurrent exchanger
Occurs in vasa recta
Mechanism of increasing permeability of Na &
H20
ADH
– at basolateral memb of epithelium – Inc
adenylyl cyclase (inc. cAMP)
Aldosterone
– at luminal border of epithelium – Nuclear
transcription (steroid)
Aldosterone
3 known factors that stimulate secretion from zona
glomerulosa
1. Inc AII
2. Inc K+ (most potent)
3. Dec Na+
ANF vs Aldosterone
ANF – H2O & Na secretion
Aldosterone – H2O & Na reabsorption
Both Aldosterone and principal cells act on Na-K
ATPase
Parathyroid Hormone sites of action
Kidney
Bone
GIT
MOA: Increase ECF Ca, Dec ECF PO4
Calcium Reabsorption
Late Distal Tubule – primary active transport
in basolateral memb
Proximal Tubule – Co-transport with Na
10
Phosphate concentration regulation
- mainly by “overflow” mechanism
ACID – BASE BALANCE
Bases:
Proteins, Hgb, HCO3, HPO4, NaHCO3, NaPO4
Metabolic acidosis – INC RR
Metabolic alkalosis – DEC RR
Acidosis – depress CNS
Alkalosis – excite CNS
PULMONARY VENTILATION
Defenses vs changes in H ion conc
1. buffer systems
a. bicarbonate buffer
b. PO4 buffer
c. Protein buffer – most abundant, most
powerful
2. Respiratory
3. Renal
Henderson-Hesselbach equation
pH = 6.1 + log HCO3/CO2
An increase in HCO3 increases pH
Isohydric principle
Hydrogen ion is common to chemical rxns of all
systems, any condition that changes H
concentration affects the balance of all buffer
systems
H secretion
Early tubules – countertransport
Distal tubules – intercalated discs
(H+ATPase)
Conditions causing Respi Alkalosis (a rare
condition)
Psychoneurosis (overbreathing)
High Altitude
Duration of inspiration = 2 sec
Duration of expirarion = 2-3sec
Accessory muscles of Inspiration (muscles that
raise rib cage)
SCM
Serratus anterior
Scalene
Accessosry muscles of Expiration
Rectus abdominis
Internal intercostals
Pleural Pressure
Pressure in the space bet pleura and chest
wall
-5 cmH2O at beginning of insp; 7.5 cmH2O
during inspiration
Alveolar Pressure
Pressure inside the alveoli
Equal to atmospheric pressure if glottis is
closed (0 cmH20)
-1 cmH20 during inspiration
Respiratory acidosis
Any condition that impairs gas exchange bet
blood & alveolar air
Transpulmonary Pressure
Pressure difference bet alveolar P & pleural P
Measure ELASTIC forces that tends to
collapse the lung (recoil pressure)
Compliance of Lungs
Extent by which lungs EXPAND for each unit
of increase in transpulmonary pressure
200mL/cm of H20
Metabolic acidosis
Diarrhea – lose NaHCO3
Vomiting – If from UGI – alkalosis; ifrom LGI
– acidosis
Uremia
DM –fats split into acetoacetic acid
Surfactant
Type II pneumocytes
Dipaylmitoyl Lecithin – decreases surface
tension;
Surfactant apoproteins & Lecithin –
increases the rate by which Lecithin spreads
Metabolic Alkalosis
Any condition that INC Na reabsorption increases H
secretion
Diuretics (except carbonic anhydrase
inhibitors)
Alkaline Drugs (drugs containg NaHCO3)
Pyloric stenosis
Excess Aldosterone
Interdependence Phenomenon
Large Alveolus cannot exist adjacent to a small
alveolus because they share common septal walls &
the presence of surfactant
First Generation Respiratory Passageway
- Trachea
11
Greatest amount of Resistance to airflow
- Bronchi (near trachea)
Histology of Bronchioles
No cartilage
Only smooth Ms
Volumes
TV – 500 mL
IRV - 3000 mL
ERV – 1100 mL
RV – 1200 mL
Capacities
IC = From beginning of N expiration then inhale
maximally; TV + IRV = 3500mL
FRC = Air remaining in lungs after N expiration;
ERV + RV 2300mL
VC = Max inhalation followed by Max Expiration;
IRV +ERV + TV 4600 mL
TLC = IRV + ERV + TV +RV = 5800 mL
Volumes and Capacities 20 -25% lower in WOMEN
Minute Respiratory Volume
RR x TV
6L/min
Normal dead space volume
150mL
Anatomic dead space
Part of respiratory system besides gas exchange
areas
Physiologic dead space
Alveolar dead space
Hering-Breuer Inflation Reflex
When lungs become overly inflated, stretch
receptors in bronchial & bronchiolar walls are
activated, this switches off the inspiratory ramp &
stops further inspiration
Activated only when TV >1.5L
BOHR EFFECT
Effect of CO2 & H on O2-Hgb dissociation
curve
Lungs: CO2 diffuses from blood to alveoli,
decreasing PCO2 & H
Shifts the curve LEFTward & Upward
Tissues: CO2 enters blood from tissues
Shifts the curve RIGHTward
Inc CO2 in blood promotes Hgb release of O2 into
tissues
Dec CO2 in blood promotes Hgb binding of O2 from
lungs
Chloride Shift
Venous blood has higher Cl- than arterial
blood
HALDANE EFFECT
Lungs: Increased release of CO2 because of O2
pick-up by Hgb
- More important for CO2 transport than
Bohr
Tissues: Inc pick-up of CO2 because of O2 removal
from hemoglobin
Afferents of cough reflex – Vagus
Afferents of sneeze reflex – CN 5
- (+) Uvular depression so air passes to
nose (not in the mouth as in coughing)
RLD – Dec FVC, N FEV1, ratio of FVC/FEV1
decreases
OLD – N FVC, Dec FEV1, ratio of FVC/FEV1
increase
Phonators – Larynx
Articulators – Mouth (lips, tongue, soft palate)
Resonators – Mouth, Nose with nasal sinuses,
pharynx & chest cavity
O2-Hgb Dissociation curve
Shift to the Right (release)
Inc CO2
Inc Temp
Inc 2,3 DPG
Inc Hydrogen
Dec pH
Pulmonary SBP – 25mmHg
Pulmonary DBP – 8 mmHg
Mean pulmonary arterial p – 15mmHg
Measures LEFT ATRIAL pressure
Pulmonary Wedge Pressure ( 5mmHg)
Shift to the Left
Inc fetal Hgb
12
RESPIRATORY CENTER
DORSAL RESPIRATORY GROUP
Nucleus of Tractus Solitarius on reticular
subst of Medulla
Control of INSP & RHYTHM
(+) Ramp signal
PNEUMOTAXIC CENTER
Nuleus Parabrachialis on dorsal upper pons
Limit duration of Inspiration (thereby
increasing RR)
“Switch-off” for inspiratory ramp
VENTRAL RESPIRATOR GROUP
Nucleus Ambiguus & Retroambisguus
Both INSP & EXP
“Overdrive” mechanism for high levels of
pulmo venti
Powerful EXP signals to abdominal muscles
APNEUSTIC CENTER
Lower pons
Prevent switch-off of Inspiratory ramp
Control RATE & PATTERN of breathing
Controls DEPTH of respi (like pneumotaxic)
Inspiratory “RAMP” signal
Nerous signals begins very weakly then increases
steadily for 2 sec then abruptly stops for 3 sec, then
begin again
Not instantaneous burst of signals which would
produce inspiratory gaps
Chemical Control of Respiration
The only important direct stimulus for
chemosensitive neurons
- Hydrogen
Hydrogen ions are impermeable to BBB &
Blood-CSF barrier
Major controller of respiration
- Carbon dioxide
Carbon dioxide
Very permeable to barriers
has an indirect effect by first combining with
H20
Forms Carbonic Acid (H2CO3) which then
dissociates into H & HCO3 upon passing the
barriers
Respiratory Centers affected MORE by
changes in CO2 level then hydrogen
Chemosensitive area
- 1mm beneath ventral surface of medulla
Chemoreceptors
Carotid bodies – Hering’s Nerve (CN9)
Aortic bodies – CN10
During Strenous Exercise
PO2, PCO2 & pH are WNL
The 2 factors causing inc RR during
exercise:
1. stimulatory signals to CNS
2. Proprioceptors
J – receptors
Stimulated by irritant chemicals in pulmo
blood
In juxtaposition to pulmo capillaries
FCN: gives the person a feeling of
DYSPNEA
Cheyne-Stokes
Periodic respiration seen in:
Heart failure
Brain damage
HIGHT ALTITUDE PHYSIOLOGY
Level of Arterial O2 saturation causing LOC
40-50%
12,000 ft = (+) HA, dizziness
18,000ft = (+) twitching, convulsions
23,000ft = (+) coma
Physiologic changes in ACCLIMITIZATION
Inc pulmo ventilation
Inc RBC
Inc Diffusing capacity of Lung
Inc Vascularity
Inc O2 utilization ability
Inc Hct (60-65)
Inc Hgb (22)
Inc blood volume (20-30%)
Inc cardiac output (30%)
Inc mitochondria
Physical changes seen in natives of high Altitudes
Inc chest size
Inc right side of heart
Dec body size
Factors decreased in high altitude
Dec Body size
Dec Work capacity
Accelerations = mv2/r
4-6G : (+) LOC
20G : (+) vertebral fracture
Negative 4-5G : (+) hyperemia of head
(+) psychosis
(+) brain edema
(+) redout eye
13
Function of nitrogen in sealed aircrafts
- prevent atelectasis
DEEP SEA
120ft : (+) joviality (lose many of his cares)
150 – 200ft : drowsy
200-250ft : strength wanes; clumsy
Observed effects of prolonged stay in space
1. decrease in blood volume
2. dec RBC mass
3. dec strength & ork capacity
4. dec cardiac output
5. loss of Ca & PO4
Effects are NOT progressive after a few weeks
EXCEPT for BONE LOSS (continues for many
months)
Oxygen toxicity manifestation
(+) visual disturbance & disorientation
Chronic O2 poisoning (exposure to 100% O2 >
12hrs)
Pulmo congestion
Pulmo edema
Atelectasis
Mechanism of Nitrogen narcosis
Dec excitability of membranes due to high fat
affinity
PCO2 toxicity level for respiratory depression
>80mmHg
Effect of EXERCISE on decompression sickness
Hastens formation of nitrogen bubbles due to
increased agitation of tissues and fluids
Inc susceptibility to O2 toxicity
Gas used in deep-sea diving as a gas mixture
HELIUM (instead of nitrogen as in high altitudes)
- has only 1/5 narcotic effect than N2
- only ½ dissolves in body fluids than N2
- low density, less airway resistance for
breathing
To prevent EMBOLISM during ascend
Exhale continually
Uses of Hyperbaric O2 Therapy
Gas gangrene
Leprosy
MI
Osteomyelitis
Arterial gas embolism
CO poisoning
WEIGHTLESSNESS
Physiologic problems of weightlessness is related to
3 known effects:
1. motion sickness
2. translocation of fluid
3. dec physical activity
GIT PHSYIOLOGY
Myeneteric (Auerbach’s Plexus) – bet longitudinal &
circular muscle layers
Fcns
1. Inc tone of gut wall
2. inc intensity of rhythmical contraction
3. inc rate of rhythm
4. inc velocity of conduction for rapid peristalsis
- Inhibits contracted intestinal sphincter that
impedes food mov’t thru VIP
Submucosal (Meissner’s Plexus) – submucosa
Fcns
1. intestinal secretion
2. local absorption
3. contraction of submucosal muscle causing
infolding of stomach muosa
Law of the gut
Peristaltic reflex plus the analward direction
of movement of peristalsis
Usual stimulus for peristalsis
- Distention
Storage capacity of stomach
1.5L
Promoters of stomach emptying
1. gastric distention
2. gastrin
Both increase pyloric pumping force & inhibit
pylorus
Most potent inhibitor of Gastric Emptying
CCK (stimulated by FATS)
Movements of small intestine
1. Mixing or segmentation contractions
2. Propulsive movements (peristalsis)
Movements of the Colon
1. haustral contraction
2. mass movements
14
Tubular glands in stomach mucosa
Oxyntic (or gastric) glands (body or fundus)
Secretes: HCl, Intrinsic factor, mucus,
pepsinogen
Pyloric glands (antrum)
Secretes: gastrin, mucus, pepsinogen
Stimulators of gastric gland secretion:
Histamine
Ach
Gastrin
H2O absorption
Diffusion (Osmosis) at tight junctions of
apical epithelial cells
Na absorption
Active transport at basolateral walls of
epithelial cells
Chloride
Passively Co-transported with Na
Active absorption of HCO3
Indirectly absorbed by Na-H countertransport
H binds with HCO3 forming carbonic acid,
which then dissociates to form CO2 & H2O
Gastrin
-
stimulates parietal cell to increase HCl
secretion
released by G-cells
G17 – more abundant, longer t ½
G34 – more active, shorter t ½
Stimulus of Pepsinogen secretion
1. Ach released from vagus
2. acid in stomach
Stimulators of Pancreatic Enzyme secretion
1. Ach
2. Gastrin
3. CCK
4. Secretin
Secretin
-
stimulated by acids from stomach
released by S-cells of duodenum &
jejunum
stimulates the pancreas to secrete large
quantities of HCO3
bicarbonate secretion lower duodenal pH
to optimal activity of pancreatic enzymes
CCK
-
stimulated by fats & AA
released by I-cells in duodenum
ABSORPTION
Absorption by Na-cotransport
Glucose
Galactose (most rapidly transported
monosaccharide)
Amino acids
Absorption by facilitated diffusion
Fructose (only monosaccharide with this
mech of absorption)
15
RELATED PAPERS
Gentes e paisagens luso brasileiras
Livro organizado Gentes e paisagens luso brasileiras Completo2023 •
The CoESPU Magazine
Cultural heritage and ideological discourse. The cases of Afghanistan, Syria and Iraq2022 •
Cankaya University Journal of Humanities and Social Sciences
Designing Telecollaboration Projects for Developing Intercultural Communicative Competence2021 •
2020 •
Frontiers in plant science
Grapevine Grafting: Scion Transcript Profiling and Defense-Related Metabolites Induced by Rootstocks2017 •
Jurnal RISET Geologi dan Pertambangan
Kesesuaian Lahan Untuk Komoditas Teh DI Wilayah Sagalaherang, Subang, Jawa Barat2011 •
2008 Symposium on VLSI Technology
A cost effective 32nm high-K/ metal gate CMOS technology for low power applications with single-metal/gate-first process2008 •
International Journal of Engineering Science
Absorbing boundary conditions for a 3D non-Newtonian fluid–structure interaction model for blood flow in arteries2010 •
2001 •
2009 •
Systems, Man and Cybernetics
On amount and quality of bias in reinforcement learning1999 •
 Alyanna Lacorte
Alyanna Lacorte