Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser.
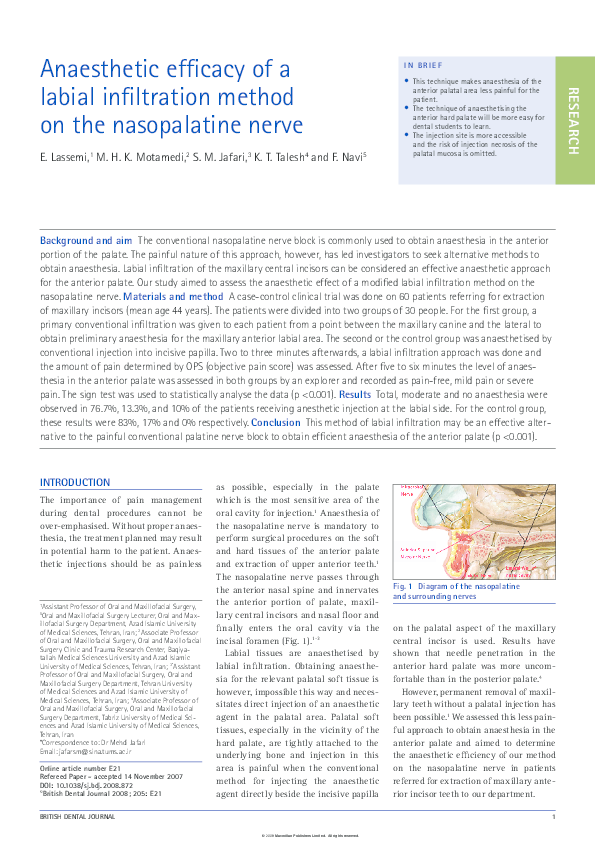
Anaesthetic efficacy of a labial infiltration method on the nasopalatine nerve
Anaesthetic efficacy of a labial infiltration method on the nasopalatine nerve
2008, BDJ
Related Papers
Dental Research Journal
Anterior and middle superior alveolar nerve block for anesthesia of maxillary teeth using conventional syringe2012 •
Brazilian Dental Journal
Effectiveness of nasopalatine nerve block for anesthesia of maxillary central incisors after failure of the anterior superior alveolar nerve block technique2007 •
The purpose of this study was to assess the effectiveness of nasopalatine nerve block for anesthesia of maxillary central incisors after failure of the anterior superior alveolar nerve (ASAN) block technique. Secondarily, the possible innervation of the maxillary central incisors by the nasopalatine nerve was also investigated. Twenty-seven healthy, young adult volunteers (age: 17-26 years; gender: 9 males and 18 females) were enrolled in this study. All participants were undergraduate dental students of the University of Vale do Rio Verde de Três Corações. The volunteers had the anterior superior alveolar nerves anesthetized and a thermal sensitivity test (cold) was performed on the maxillary central incisors. The volunteers that responded positively to cold stimulus received a nasopalatine nerve block and the thermal sensitivity test was repeated. All participants were anesthetized by a single operator. Three patients presented sensitivity after both types of bilateral blocks and ...
IP International Journal of Maxillofacial Imaging
Comparison of posterior superior alveolar and greater palatine nerve block with local infiltration for extraction of maxillary molars in oral surgery – A randomized controlled trialAdministration of local anesthetic drug that prevents pain during dental treatment is of absolute importance. Act of injecting local anesthetic should be nonpainful and atraumatic. The maxilla is very porous and highly vascular. Therefore, anesthesia of maxillary teeth can be accomplished more easily than with mandibular teeth. The aim of this study is to determine the anesthetic efficacy of the conventional technique of posterior superior alveolar (PSA) and greater palatine nerve(GP) block anesthesia as compared to the buccal and palatal technique in terms of pain during injection, after extraction, after 15mins of the procedure and quality of anesthesia during the extraction procedure. The study also intends to determine the incidence of positive aspiration in the infiltration technique. This randomized clinical study was carried out on 154 patients who reported to the Department of Oral and Maxillofacial Surgery, Sri Rajiv Gandhi College of Dental Sciences & Hospital Bangalore, r...
2016 •
Introduction: In this article, we present a modification of the conventional inferior alveolar nerve block technique which is simple, easy to master, has high success rate and comfortable to patients as multiple needle penetrations are avoided. In the standard technique, following anesthesia of inferior alveolar nerve, the needle is redirected for lingual nerve anesthesia leading to potential complications, which is avoided in single injection straight line technique. Materials and Methods: A clinical study of alternative inferior alveolar nerve block along with long buccal and lingual nerve blocks, by injecting local anesthesia into the pterygomandibular space by single penetration without redirecting the needle was performed on 207 patients undergoing simple extractions and surgical extractions of mandibular molars. The study was conducted over a period of 2 years. Results: Among 207 patients who underwent extraction, anesthesia was completely successful in 202 patients. The remai...
Journal of the Korean Association of Oral and Maxillofacial Surgeons
Single-insertion technique for anesthetizing the inferior alveolar nerve, lingual nerve, and long buccal nerve for extraction of mandibular first and second molars: a prospective study2020 •
This article reviews research and author experience behind Intraligamentary Local Anaesthesia (ILA) and Infiltration Local Anaesthesia (IFA) with Inferior Alveolar Nerve Block (IANB). In particular, the use of ILA with 4% articaine is discussed as an effective anaesthetic technique to replace both IANB and IFA for the purpose of tooth extraction in the posterior mandible. ILA also avoids the possible complications associated with IANB. Other advantages and some shortfalls of the ILA technique are described in relation to primary dental care. The technique for achieving ILA is described. CPD/Clinical Relevance: The ILA technique with articaine is a simple, swift and effective alternative to IANB and IFA for extraction of posterior teeth in the mandible in primary dental care. ILA has fewer potential debilitating complications than IANB and is likely to be more effective than IFA.
Egyptian Dental Journal
Extraction of Mandibular Posterior Teeth: Comparison between standard Inferior Alveolar Nerve Block and Local Infiltration anesthesia2020 •
Clinical Oral Investigations
RCT on the effectiveness of the intraligamentary anesthesia and inferior alveolar nerve block on pain during dental treatmentObjective To compare the effectiveness and complications of intraligamentary anesthesia (ILA) with conventional inferior alveolar nerve block (IANB) during injection and dental treatment of mandibular posterior teeth. Materials and methods In this randomized, prospective clinical trial, 72 patients (39 males, 33 females), scheduled for dental treatment of mandibular posterior teeth, were randomly allocated to ILA group (n = 35) received ILA injection or IANB group (n = 37) received the conventional IANB. Our primary outcome was to assess pain and stress (discomfort) during the injection and dental treatment, using the numeric rating scale (NRS) from 0 to 10 (0 = no pain, 10= the worst pain imaginable), whereas recording 24-h postoperative complications was our secondary outcomes. Results Patients in ILA group reported significantly less pain during injection when compared with IANB group (p = 0.03), while pain during dental treatment was similar in both groups (p = 0.2). Patients in...
RELATED PAPERS
La qualità totale applicata ai lubrificanti per motori di autoveicolo
La qualità totale applicata ai lubrificanti per motori di autoveicolo1992 •
Economic and Political Weekly
From Sairat to Jhund via Jai Bhim Caste and the Culture Industry of Hindi Cinema2022 •
European Journal of Cancer
The impact of organised screening programmes on the stage-specific incidence of breast cancer in some Italian areas2003 •
Revista de Investigación en Educación
Promoviendo el pensamiento creativo a través de las narrativas visuales y literarias: un estudio de caso en el Grado en Maestro/a de Educación Infantil2021 •
European Child & Adolescent Psychiatry
Understanding anhedonia: a qualitative study exploring loss of interest and pleasure in adolescent depression2019 •
The Medical journal of Malaysia
Radio-opacity of commonly consumed bony fish in kelantan, malaysia2012 •
1999 •
International Journal of Knowledge and Systems Science
Experience Sharing Service Value Co-Creation Model (ESSVC) and Its Application to Korean Language Service2013 •
Fonseca Journal of Communication
La mirada audiovisual sobre el mundo rural español2013 •
 MOHAMMAD MOTAMEDI
MOHAMMAD MOTAMEDI