Maw5595 Paper 1
Maw5595 Paper 1
Uploaded by
Michael WilsonCopyright:
Available Formats
Maw5595 Paper 1
Maw5595 Paper 1
Uploaded by
Michael WilsonOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Maw5595 Paper 1
Maw5595 Paper 1
Uploaded by
Michael WilsonCopyright:
Available Formats
LOW-TEMPERATURE PLASMA NEEDLE FOR BIOMEDICAL TREATMENTS
Michael A. Wilson,1 Timothy R. Brubaker,2 Andrea M. Mastro,3
Michael M. Micci,4 Sven G. Biln,5 and Sean D. Knecht 6
1
Undergraduate Student, Department of Electrical Engineering; 2Ph.D. Student,
Department of Electrical Engineering; 3Professor of Microbiology and Cell Biology,
Department of Biochemistry and Molecular Biology; 4Professor of Aerospace Engineering,
Department of Aerospace Engineering; 5Assoc. Prof. of Engineering Design, Electrical
Engineering, and Aerospace Engineering, Department of Electrical Engineering; 6Research
Faculty, Applied Research Laboratory
ABSTRACT
An overview of the design methodology of a lowtemperature plasma needle and preliminary results
investigating its efficacy in treating metastatic human
breast cancer epithelial cells is reported. Low-temperature
plasma is created by flowing gas past a high-voltage
surface. This process produces ions and generates an
electrically conductive state of matter (plasma) at room
temperature. High-energy collisions of electrons with
neutral particles create reactive chemical species such as
NO, O3, H2O2 and others which have biomedical
applications. Current cancer treatment options, such as
surgery and chemotherapy, may not be sufficient to treat
metastatic cancer. Initial experiments have been conducted
in which a line of cultured metastatic human breast cancer
epithelial cells (MDA-MB-231) are exposed to the lowtemperature plasma needle. The plasma needle is lowered
into cell culture dishes and the cells are exposed to plasma
at different dosages. Cell detachment was observed for
plasma and helium-exposed cultures with a greater effect
observed for plasma-exposed cultures. This is attributed to
reactive chemical species generation in the plasma plume.
Experiments are continuing to optimize the treatment
conditions and further this research.
1. INTRODUCTION
The number of women in the U.S. with a history of breast
cancer was estimated to be more than 3.1 million as of
January 1, 2014 with an additional 232,670 women
expected to be diagnosed in 2014 [1]. Approximately 43%
of women diagnosed with breast cancer are 65 years and
older, 20% are under the age of 50, and 37% are between
50 and 65 years old [1], with an average age of 61 [1]. This
form of cancer, unless treated early, generally metastasizes
to areas such as bone, ovaries, skin, and pericardium [2].
Approximately 2030% of breast cancer victims will later
find out that their breast cancer has become metastatic and
the average survival period after this diagnosis is three
years [3]. The average 5-year survival rate for this disease
has increased from 75% between 1975 and 1977, to 90%
between 2003 and 2009 [1]. While the survival rate has
increased significantly, the methods that are currently used
to treat cancer still have limitations. Any new methods of
eradicating the areas that are affected by the breast cancer
cells without harming the adjacent healthy cells would
benefit cancer patients. This research group is working on
using low-temperature plasma as a possible therapy option
for breast cancer patients.
The term plasma was coined in 1928 by Irving
Langmuir because the substance reminded him of blood
plasma [4]. Plasma is the most common state of matter
found in the universe and finds many uses and applications
in a variety of fields. For example, the medical community
uses plasmas for disinfection and sterilization [512].
Scientists classify plasma into two main types: hightemperature (thermal) plasma, or HTP, and lowtemperature (non-thermal) plasma, or LTP. LTP remains
near room temperature making it easier to work with
compared to HTP. The generation of LTP is due to the
thermal equilibration of electron self-collisions occurring
faster than the equilibrium between electrons and ions. This
leads to high electron temperatures and very low gas
temperatures [5]. Researchers have realized that LTP can
be useful in many applications within the medical field, due
to the generation of reactive chemical species in the plasma
plume. Specifically, there have been many experiments
with plasmas in areas of cancer research and dentistry [13].
Scientists and engineers have been researching and
working to commercialize these therapies.
A dielectric barrier discharge (DBD), also known as a
barrier discharge or silent discharge, is an electrical
discharge that occurs between two electrodes that are
separated by a dielectric barrier. One of the electrodes is
connected to a high voltage (AC) power supply and the
other electrode is connected to ground. The DBD method
is beneficial because it provides a wide range of geometric
as indicated. Each well is circular with a diameter of 15.6
mm and holds a maximum volume of 3.4 mL
3. EXPERIMENTAL DESIGN
Figure 1. Schematic of an LTP dielectric barrier
discharge. The HV power supply is connected to the
syringe which is encased within the dielectric barrier
(PEEK). The gas flows through the back and out of the
tip of the syringe as plasma.
configuration options. With respect to biomedical
applications, configurations can include quartz plates
covering one or both electrodes; high-voltage insulated
wires plasma stamp; plasma stick; plasma comb; and
plasma roller [14], among many others. Rather than
generating a plasma plume within small discharge gaps,
plasma jets generate plasma in the open air (see Figure 1).
Due to the applications on living tissue, the current is kept
in the milliamp range to prevent electric shock. In terms of
the grounding electrode, an external or internal ground
configuration may be used. The external configuration is
required for plasma jets using noble gases. An internal
configuration can be used for air-plasma jets in which the
grounding electrode is within a metal cap. The high energy
collisions between the gases and neutral molecules create
the reactive species of interest for biomedical treatments.
This paper details the design of preliminary LTP
experiments with emphasis on breast cancer research. The
remainder of this paper is structured as follows. Section 2
introduces information about the cancer cell line used in the
experiments. Section 3 explains how the LTP needle was
designed and discusses the experiments and the methods
used in testing the plasma on breast cancer cultures. Section
4 discusses the results. Section 5 provides concluding
remarks and plans for future research.
The goal of the experiments is to investigate the effects of
LTP on metastatic BCs. A design methodology for the LTP
source was established such that it could eventually suit the
needs of doctors working with this equipment in a clinical
setting.
The syringe system includes two electrodes to generate
the plasma. The syringe itselfa 22-gauge needle that is 2
long serves as the high-voltage electrode. Helium flows
axially through the syringe (note: this configuration is
slightly different that that shown in Figure 1, but is
conceptually the same). The syringe is sheathed with PEEK
(polyether ether ketone) plastic tubing, which serves as the
dielectric barrier around the needle. PEEK has a high
dielectric strength and is used as a barrier to prevent arc
production. The overall diameter of the device is equivalent
to a 16-gauge needle.
The ground electrode is placed approximately 1/8
from the tip of the syringe. The placement of the ground is
important for generating plasma, as it can affect the electric
field that is formed on the needle. This electric field is
necessary for the formation of plasma because it accelerates
electrons, resulting in high energy collisions with neutral
particles (atoms, molecules) that are already flowing
axially. These collisions result in atomic excitation or
molecular dissociation processes which result in reactive
chemical species in the plasma plume. The operation of this
setup is demonstrated in Figure 2, which shows the
dielectric barrier discharge interface on a saline sample.
Since the device is exposed to very high voltage, it is
essential to make sure that the high voltage and ground
were encased safely in a polycarbonate clear tubing (1.5
inner diameter, 1.75 outer diameter). This arrangement
allows the operator to hold onto the syringe without being
2. CELL CULTURE
For these experiments human metastatic breast cancer cells
(MDA-MB-231, ATCC-HTB 26 presumptive equivalent)
that were genetically engineered to produce green
fluorescent protein (GFP) were utilized. Hereafter these are
referred to as BCs. Derived from a pleural effusion [15],
MDA-MB-23GFP cells are known to invade the murine
skeleton [16].
Before use, the cells were grown to confluency in
Dulbeccos Modified Eagles Medium (DMEM) with 5%
fetal bovine serum and 1 essential amino acids in 24- or
48-well standard tissue culture plates made of polystyrene
Figure 2. The interface between the LTP syringe
interacting with a saline sample. The visible plasma jet
has a diameter similar to the syringe.
exposed to the high voltage. It is also preferable to have
optical access to the device which is why clear
polycarbonate tubing was used. Holes were drilled within
the tubing to thread the voltage line through the device to
its respective input location.
An optical table is used to hold the syringe in place and
allows precise motion in the x, y, and z directions. This
optical table is able to hold the syringe at one spot in the
cell culture wells. As mentioned in Section 2, the cultures
were placed in 24- and 48-well cell culture plates. The
plasma jet is lowered into the cell culture wells to a height
at which the jet is visibly in contact with the surface of the
buffer solution in the wells.
Helium is used for plasma production during the
experiments. Additional gases will be mixed with the
helium as dopants in future experiments to increase reactive
species generation. The helium flow rate is controlled via a
mass flow controller (MFC) which is calibrated for gases at
70 F, 14.7 psia. The flow rate can be controlled over the
range of 15-775 mL/min.
The electric field is generated by the high voltage
applied to the metal syringe. An Agilent 33220A Function
Generator generates a 5-kHz, 2-Vpp sine wave which is
amplified 1000 to 2 kV by a Trek 10-40 amplifier.
Although the voltage amplifier has current-limiting
Figure 3. Full LTP setup. Helium is introduced to the
system using a mass flow controller. The voltage and
ground inputs are connected to the power supply and
threaded through the tube to their respective input
locations. The optical table is used for support and
measurement purposes.
capability, a secondary current limiter is included via a 500k resistor stack. Increasing the voltage or mass flow rate
of the helium results in an increasing length and visible
intensity of the plasma plume. Figure 3 shows the setup
used for these experiments.
4. RESULTS
Over several days, data were collected to determine how
the cells responded to treatment with LTP. Cell cultures
were observed with microscopy pre- and post-exposure.
For the first group of experiments, it was observed that
there was an equal amount of cell detachment from both the
plasma and helium exposure. This result suggests that there
was a physical effect of the flow velocity on the cell culture
medium. Specifically, it is likely that the kinetic energy of
the flowing helium was sufficient to damage the cultured
cells under these conditions. It was necessary to limit this
effect in the subsequent experiments in order to isolate
potential effects of reactive chemistry.
For the second group of experiments, the cells were
exposed to helium and plasma for 90 seconds with 200-L
of PBS (phosphate buffered saline). PBS provides a
physical buffer to the cell culture and also prevents the cells
from drying out and dying. This buffer was then
immediately removed after the treatment and cell culture
medium was re-introduced. No effect was observed for
both helium- and plasma-exposed cells indicating that jet
kinetic energy did not penetrate the PBS, which further
supports the conclusions from the first group of
experiments. However, the diffusion of reactive chemical
species was also likely prevented in this case.
For the third group of experiments, the growth medium
was removed from the cells and 200 L of PBS was added
to two sets of wells and 100 L of PBS to one set. The
plasma was then applied for 120 seconds to the 200- and
100-L samples. The other 200-L sample was also
exposed for 180 seconds. After exposure, the samples were
left alone for 5 minutes before the PBS was removed and
the growth medium re-introduced. The same procedure was
followed for the pure-helium exposure to the cells as a
control. The voltage was 2.5 kVpp at a frequency of 5 kHz.
It was observed that the cell cultures had large circular
holes in the areas that were exposed to both the plasma and
the helium. Critically, the holes left from the pure helium
were smaller in area.
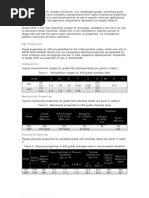
The final group of experiments utilized 50 L of PBS
in each of six total wells. Three cell culture wells were
exposed to the helium and three wells were exposed to the
plasma. Two of the six wells were exposed for 60 seconds,
whereas the other four were exposed for 180 seconds. The
mass flow rate was at its maximum of 775 mL/min. After
the experiments, it was observed that the plasma exposed
cultures had voids in the cell culture that were two to three
times the diameter of the voids in the helium-exposed
cultures, as shown in Figure 4. This result indicates an
(a)
(b)
(c)
(d)
Figure 4. Images of metastatic breast cancer culture MDA-MB-231 post treatment. Images are equivalent in scale. Each
culture was exposed to 3-minute dosages. (a) Helium-exposed culture, (b) Plasma-exposed culture, (c) Helium-exposed
culture, (d) Plasma-exposed culture. The voids in cell culture are larger for plasma-exposed culture.
additional mechanism of cell destruction is active in the
low-temperature plasma beyond the kinetic energy of the
jet molecules. The hypothesis is that reactive oxygen
species generated in the plasma plume are responsible for
the increased destructive effects due to increased oxidative
stress on the cells. These reactive species can diffuse
through the surrounding air and the PBS buffer, resulting in
a larger area of cell destruction compared to the helium jet.
Further experimentation is planned to quantify the
generation of reactive chemical species and evaluate this
hypothesis.
Further investigation is needed to determine why the
pure helium exposure can result in cell destruction.
Different gases will also be used in future experiments as
well as longer treatment times to the cultures themselves.
Larger diameter wells and a greater volume of PBS will
also be used. Further experiments will be executed in the
near future to investigate the role that low-temperature
plasma, and subsequent enhanced reactive chemistry in the
plasma plume, has in successfully treating cancer cells
without harming neighboring healthy tissue by expanding
upon the results from these preliminary tests.
Acknowledgments
5. CONCLUSIONS
In summary, a preliminary investigation of the effects of a
low-temperature plasma needle on metastatic breast cancer
cultures was undertaken. The results indicate that the
helium jet and the plasma jet both result in cell destruction
under certain conditions. Cell destruction was observed to
occur for a larger area in the case of the plasma jet
indicating an additional mechanism of cell destruction
beyond the kinetic energy of the jet molecules. The
generation of reactive oxygen species in the plasma plume
and the subsequent oxidative stress on the cells is the
proposed method of action. The results provide a solid basis
for continuing investigations regarding the mechanisms
and efficacy of low-temperature plasma on metastatic
breast cancer.
The authors wish to thank D. Sosnoski, for helping prepare
the cell cultures. The BC line (MDA-MB-231, ATCC-HTB
26 presumptive equivalent) was initially provided by Dr. D.
Welch, University of Alabama at Birmingham.
REFERENCES
[1] American Cancer Society. Cancer Treatment and
Survivorship Facts & Figures 20142015. Atlanta:
American Cancer Society; 2014.
[2] G. diSibio and S. French, Metastatic Patterns of Cancers:
Results from a Large Autopsy Study, Arch. Pathol. Lab.
Med., vol. 132, 2007.
[3] J. OShaughnessy, Extending Survival with Chemotherapy
in Metastatic Breast Cancer, The Oncologist, vol. 10, no. 3,
pp. 2029, 2005.
[4] W. Thornhill and D. Talbott, The Electric Universe.
Portland, OR: Mikamar Pub., 2007.
characterization, In Vitro, vol. 14, no. 11, pp. 911915,
1978.
[16] D. Rusciano, D. Welch and M. Burger, In vivo cancer
metastasis assays, in Cancer metastasis: experimental
approaches. Amsterdam: Elsevier, 2000, pp. 207242.
[5] M. Wang, B. Holmes, X. Cheng, W. Zhu, M. Keidar and L.
Zhang, Cold Atmospheric Plasma for Selectively Ablating
Metastatic Breast Cancer Cells, PLoS ONE, vol. 8, no. 9, p.
e73741, 2013.
[6] R. Walk, J. Snyder, P. Srinivasan, J. Kirsch, S. Diaz, F.
Blanco, A. Shashurin, M. Keidar, and A. Sandler, Cold
atmospheric plasma for the ablative treatment of
neuroblastoma, Journal of Pediatric Surgery, vol. 48, no. 1,
pp. 6773, 2013.
[7] M. Keidar, A. Shashurin, O. Volotskova, M. Ann Stepp, P.
Srinivasan, A. Sandler and B. Trink, Cold atmospheric
plasma in cancer therapy, Physics of Plasmas, vol. 20, no.
5, p. 057101, 2013.
[8] R. Guerrero-Preston, T. Ogawa, M. Uemura, G.
Shumulinsky, B. Valle, F. Pirini, R. Ravi, D. Sidransky, M.
Keidar and B. Trink, Cold atmospheric plasma treatment
selectively targets head and neck squamous cell carcinoma
cells, Int. J. Mol. Med., 2014.
[9] A. Hirst, F. Frame, N. Maitland and D. OConnell, Low
Temperature Plasma: A Novel Focal Therapy for Localized
Prostate Cancer? BioMed Research International, vol.
2014, pp. 115, 2014.
[10] O. Volotskova, T. Hawley, M. Stepp and M. Keidar,
Targeting the cancer cell cycle by cold atmospheric
plasma, Scientific Reports, vol. 2, 2012.
[11] X. Cheng, J. Sherman, W. Murphy, E. Ratovitski, J. Canady
and M. Keidar, The Effect of Tuning Cold Plasma
Composition on Glioblastoma Cell Viability, PLoS ONE,
vol. 9, no. 5, p. e98652, 2014.
[12] S. Mirpour, H. Ghomi, S. Piroozmand, M. Nikkhah, S.
Tavassoli and S. Azad, The Selective Characterization of
Nonthermal Atmospheric Pressure Plasma Jet on Treatment
of Human Breast Cancer and Normal Cells, IEEE
Transactions on Plasma Science, vol. 42, no. 2, pp. 315322,
2014.
[13] C. Hoffmann, C. Berganza and J. Zhang, Cold Atmospheric
Plasma: methods of production and application in dentistry
and oncology, Med Gas Res, vol. 3, no. 1, p. 21, 2013.
[14] Y. Kim, S. Jin, G. Han, G. Kwon, J. Choi, E. Choi, H.
Uhm and G. Cho, 'Plasma Apparatuses for Biomedical
Applications', IEEE Transactions on Plasma Science, pp. 11, 2015.
[15] R. Cailleau, M. Oliv and Q. Cruciger, Long-term human
breast carcinoma cell lines of metastatic origin: Preliminary
You might also like
- Electrophysiological Recording Techniques PDFNo ratings yetElectrophysiological Recording Techniques PDF7 pages
- Results: Michael A. Wilson, Timothy R. Brubaker, Andrea M. Mastro, Michael M. Micci, Sven G. Bilén, and Sean D. KnechtNo ratings yetResults: Michael A. Wilson, Timothy R. Brubaker, Andrea M. Mastro, Michael M. Micci, Sven G. Bilén, and Sean D. Knecht1 page
- Cancer Development and Damped Electromagnetic ActivityNo ratings yetCancer Development and Damped Electromagnetic Activity17 pages
- DR Royal R Rife - Pulsed Field Assisted ChemotherapyNo ratings yetDR Royal R Rife - Pulsed Field Assisted Chemotherapy11 pages
- Engineering A 3D Microfluidic Culture Platform For Tumor-Treating Field ApplicationNo ratings yetEngineering A 3D Microfluidic Culture Platform For Tumor-Treating Field Application10 pages
- Journal of Electrostatics: Sadhana Talele, Paul Gaynor, Michael J. Cree, Jethro Van EkeranNo ratings yetJournal of Electrostatics: Sadhana Talele, Paul Gaynor, Michael J. Cree, Jethro Van Ekeran14 pages
- A Statistical Model For Multidimensional Irreversible Electroporation Cell Death in TissueNo ratings yetA Statistical Model For Multidimensional Irreversible Electroporation Cell Death in Tissue13 pages
- Lin-Lymphocyte Electrotaxis in Vitro and in VivoNo ratings yetLin-Lymphocyte Electrotaxis in Vitro and in Vivo7 pages
- Antitumor Effect of Plasma Treatment On U87 Vandamme - Et - Al-2010-Plasma - Processes - and - PolymersNo ratings yetAntitumor Effect of Plasma Treatment On U87 Vandamme - Et - Al-2010-Plasma - Processes - and - Polymers10 pages
- Bioelectrochemistry: Janja Dermol, Damijan Miklav ČičNo ratings yetBioelectrochemistry: Janja Dermol, Damijan Miklav Čič10 pages
- Beebe-Diverse Effects Wideband Non Ionizing Radiation Cells Tissues-04216264No ratings yetBeebe-Diverse Effects Wideband Non Ionizing Radiation Cells Tissues-042162644 pages
- Bioimpedance, Measurement Techniques Applied To Human Skin.: NtroductionNo ratings yetBioimpedance, Measurement Techniques Applied To Human Skin.: Ntroduction3 pages
- Polymers: Electrospraying, A Reproducible Method For Production of Polymeric Microspheres For Biomedical ApplicationsNo ratings yetPolymers: Electrospraying, A Reproducible Method For Production of Polymeric Microspheres For Biomedical Applications19 pages
- Cardiac Electrophysiology Using Ls Dyna R PDFNo ratings yetCardiac Electrophysiology Using Ls Dyna R PDF15 pages
- Recent Trends On Micro-Nanofluidic Single Cell ElectroporationNo ratings yetRecent Trends On Micro-Nanofluidic Single Cell Electroporation25 pages
- Highly Sensitive and Selective Separation of Intact Parathyroid Hormone and Variants by Sheathless CE-ESI-MS/MSNo ratings yetHighly Sensitive and Selective Separation of Intact Parathyroid Hormone and Variants by Sheathless CE-ESI-MS/MS25 pages
- Electrochemotherapy in Veterinary OncologyNo ratings yetElectrochemotherapy in Veterinary Oncology6 pages
- Thermal Effects of Monopolar Electrosurgery Detected by Real-Time Infrard ThermalgraphyNo ratings yetThermal Effects of Monopolar Electrosurgery Detected by Real-Time Infrard Thermalgraphy12 pages
- Membrane Potentials in Living Systems, Tools To Measure: Biological BackgroundNo ratings yetMembrane Potentials in Living Systems, Tools To Measure: Biological Background10 pages
- Hetero-Nanojunctions With Atomic Size Control Using A Lab-On-Chip Electrochemical Approach With Integrated MicrofluidicsNo ratings yetHetero-Nanojunctions With Atomic Size Control Using A Lab-On-Chip Electrochemical Approach With Integrated Microfluidics14 pages
- SpringSim'12 Poster - Spatial Modeling of The Brain Tumor Perivascular NicheNo ratings yetSpringSim'12 Poster - Spatial Modeling of The Brain Tumor Perivascular Niche1 page
- 5d31924f02efa20190719Article_PDF_FilePrinciples of Electrosurgery in LaparoscopyNo ratings yet5d31924f02efa20190719Article_PDF_FilePrinciples of Electrosurgery in Laparoscopy8 pages
- Handout-For-Advanced Techniques in Food Processing - Pulse Electric FieldNo ratings yetHandout-For-Advanced Techniques in Food Processing - Pulse Electric Field33 pages
- Biotech Bioengineering - 2002 - Woolley - Electrochemical Monitoring of Cell Behaviour in Vitro A New TechnologyNo ratings yetBiotech Bioengineering - 2002 - Woolley - Electrochemical Monitoring of Cell Behaviour in Vitro A New Technology9 pages
- Microfluidic Transport in Microdevices For Rare Cell CaptureNo ratings yetMicrofluidic Transport in Microdevices For Rare Cell Capture10 pages
- An Overview of Capillary Electrophoresis Pharmaceutical Biopharmaceutical and Biotechnology Applicat PDFNo ratings yetAn Overview of Capillary Electrophoresis Pharmaceutical Biopharmaceutical and Biotechnology Applicat PDF35 pages
- The Healing Potency Of Pulsed Electromagnetic Field Therapy: Chronic Pain | Fibromyalgia | Arthritis | Multiple SclerosisFrom EverandThe Healing Potency Of Pulsed Electromagnetic Field Therapy: Chronic Pain | Fibromyalgia | Arthritis | Multiple Sclerosis4/5 (2)
- Case Studies in Advanced Skin Cancer Management: An Osce Viva ResourceFrom EverandCase Studies in Advanced Skin Cancer Management: An Osce Viva ResourceNo ratings yet
- Aurora Was Goddess of Dawn or The Morning Glow.No ratings yetAurora Was Goddess of Dawn or The Morning Glow.4 pages
- Uk Chemistry Olympiad Round 1 Examiners Report 2018No ratings yetUk Chemistry Olympiad Round 1 Examiners Report 20184 pages
- Bitumen and Bituminous Binders-Specification Framework For Polymer Amodified BitumensNo ratings yetBitumen and Bituminous Binders-Specification Framework For Polymer Amodified Bitumens8 pages
- Paper 2 Section A: Question 1: Form 4 (Chapter 9)No ratings yetPaper 2 Section A: Question 1: Form 4 (Chapter 9)4 pages
- 57:020 Mechanics of Fluids and Transport Processes Chapter 11 Professor Fred Stern Typed by Stephanie Schrader Fall 2005No ratings yet57:020 Mechanics of Fluids and Transport Processes Chapter 11 Professor Fred Stern Typed by Stephanie Schrader Fall 200516 pages
- Teacher PowerPoint_ Ionic Bonds and Ionic CompoundsNo ratings yetTeacher PowerPoint_ Ionic Bonds and Ionic Compounds23 pages
- 25 - 05 - 24 11 CBSE SH Chemistry Some Basic Concepts of Chemistry and Structure of Atom Weekly Test Question PaperNo ratings yet25 - 05 - 24 11 CBSE SH Chemistry Some Basic Concepts of Chemistry and Structure of Atom Weekly Test Question Paper3 pages
- Molykote Brochure For Chemicals Petrochemicals IndustriesNo ratings yetMolykote Brochure For Chemicals Petrochemicals Industries6 pages
- Optimization of Calcium Carbonate (Caco) Loading in Natural Rubber Latex Based Disposable GlovesNo ratings yetOptimization of Calcium Carbonate (Caco) Loading in Natural Rubber Latex Based Disposable Gloves4 pages
- 22020n MSS WAS BO Monitoring BE CH 2021 GeneralNo ratings yet22020n MSS WAS BO Monitoring BE CH 2021 General6 pages
- Application of The Transmission Line Model For Porous Electrodes To Analyse The Impedance Response of TiO2 Nanotubes in Physiological EnvironmentNo ratings yetApplication of The Transmission Line Model For Porous Electrodes To Analyse The Impedance Response of TiO2 Nanotubes in Physiological Environment34 pages
- Physical Science: Title: Formation of Heavy Elements in The UniverseNo ratings yetPhysical Science: Title: Formation of Heavy Elements in The Universe28 pages
- Results: Michael A. Wilson, Timothy R. Brubaker, Andrea M. Mastro, Michael M. Micci, Sven G. Bilén, and Sean D. KnechtResults: Michael A. Wilson, Timothy R. Brubaker, Andrea M. Mastro, Michael M. Micci, Sven G. Bilén, and Sean D. Knecht
- Cancer Development and Damped Electromagnetic ActivityCancer Development and Damped Electromagnetic Activity
- DR Royal R Rife - Pulsed Field Assisted ChemotherapyDR Royal R Rife - Pulsed Field Assisted Chemotherapy
- Engineering A 3D Microfluidic Culture Platform For Tumor-Treating Field ApplicationEngineering A 3D Microfluidic Culture Platform For Tumor-Treating Field Application
- Journal of Electrostatics: Sadhana Talele, Paul Gaynor, Michael J. Cree, Jethro Van EkeranJournal of Electrostatics: Sadhana Talele, Paul Gaynor, Michael J. Cree, Jethro Van Ekeran
- A Statistical Model For Multidimensional Irreversible Electroporation Cell Death in TissueA Statistical Model For Multidimensional Irreversible Electroporation Cell Death in Tissue
- Antitumor Effect of Plasma Treatment On U87 Vandamme - Et - Al-2010-Plasma - Processes - and - PolymersAntitumor Effect of Plasma Treatment On U87 Vandamme - Et - Al-2010-Plasma - Processes - and - Polymers
- Bioelectrochemistry: Janja Dermol, Damijan Miklav ČičBioelectrochemistry: Janja Dermol, Damijan Miklav Čič
- Beebe-Diverse Effects Wideband Non Ionizing Radiation Cells Tissues-04216264Beebe-Diverse Effects Wideband Non Ionizing Radiation Cells Tissues-04216264
- Bioimpedance, Measurement Techniques Applied To Human Skin.: NtroductionBioimpedance, Measurement Techniques Applied To Human Skin.: Ntroduction
- Polymers: Electrospraying, A Reproducible Method For Production of Polymeric Microspheres For Biomedical ApplicationsPolymers: Electrospraying, A Reproducible Method For Production of Polymeric Microspheres For Biomedical Applications
- Recent Trends On Micro-Nanofluidic Single Cell ElectroporationRecent Trends On Micro-Nanofluidic Single Cell Electroporation
- Highly Sensitive and Selective Separation of Intact Parathyroid Hormone and Variants by Sheathless CE-ESI-MS/MSHighly Sensitive and Selective Separation of Intact Parathyroid Hormone and Variants by Sheathless CE-ESI-MS/MS
- Thermal Effects of Monopolar Electrosurgery Detected by Real-Time Infrard ThermalgraphyThermal Effects of Monopolar Electrosurgery Detected by Real-Time Infrard Thermalgraphy
- Membrane Potentials in Living Systems, Tools To Measure: Biological BackgroundMembrane Potentials in Living Systems, Tools To Measure: Biological Background
- Hetero-Nanojunctions With Atomic Size Control Using A Lab-On-Chip Electrochemical Approach With Integrated MicrofluidicsHetero-Nanojunctions With Atomic Size Control Using A Lab-On-Chip Electrochemical Approach With Integrated Microfluidics
- SpringSim'12 Poster - Spatial Modeling of The Brain Tumor Perivascular NicheSpringSim'12 Poster - Spatial Modeling of The Brain Tumor Perivascular Niche
- 5d31924f02efa20190719Article_PDF_FilePrinciples of Electrosurgery in Laparoscopy5d31924f02efa20190719Article_PDF_FilePrinciples of Electrosurgery in Laparoscopy
- Handout-For-Advanced Techniques in Food Processing - Pulse Electric FieldHandout-For-Advanced Techniques in Food Processing - Pulse Electric Field
- Biotech Bioengineering - 2002 - Woolley - Electrochemical Monitoring of Cell Behaviour in Vitro A New TechnologyBiotech Bioengineering - 2002 - Woolley - Electrochemical Monitoring of Cell Behaviour in Vitro A New Technology
- Microfluidic Transport in Microdevices For Rare Cell CaptureMicrofluidic Transport in Microdevices For Rare Cell Capture
- An Overview of Capillary Electrophoresis Pharmaceutical Biopharmaceutical and Biotechnology Applicat PDFAn Overview of Capillary Electrophoresis Pharmaceutical Biopharmaceutical and Biotechnology Applicat PDF
- Bioenergetics: A Novel Theory for Atp SynthesisFrom EverandBioenergetics: A Novel Theory for Atp Synthesis
- The Healing Potency Of Pulsed Electromagnetic Field Therapy: Chronic Pain | Fibromyalgia | Arthritis | Multiple SclerosisFrom EverandThe Healing Potency Of Pulsed Electromagnetic Field Therapy: Chronic Pain | Fibromyalgia | Arthritis | Multiple Sclerosis
- Case Studies in Advanced Skin Cancer Management: An Osce Viva ResourceFrom EverandCase Studies in Advanced Skin Cancer Management: An Osce Viva Resource
- Uk Chemistry Olympiad Round 1 Examiners Report 2018Uk Chemistry Olympiad Round 1 Examiners Report 2018
- Bitumen and Bituminous Binders-Specification Framework For Polymer Amodified BitumensBitumen and Bituminous Binders-Specification Framework For Polymer Amodified Bitumens
- 57:020 Mechanics of Fluids and Transport Processes Chapter 11 Professor Fred Stern Typed by Stephanie Schrader Fall 200557:020 Mechanics of Fluids and Transport Processes Chapter 11 Professor Fred Stern Typed by Stephanie Schrader Fall 2005
- Teacher PowerPoint_ Ionic Bonds and Ionic CompoundsTeacher PowerPoint_ Ionic Bonds and Ionic Compounds
- 25 - 05 - 24 11 CBSE SH Chemistry Some Basic Concepts of Chemistry and Structure of Atom Weekly Test Question Paper25 - 05 - 24 11 CBSE SH Chemistry Some Basic Concepts of Chemistry and Structure of Atom Weekly Test Question Paper
- Molykote Brochure For Chemicals Petrochemicals IndustriesMolykote Brochure For Chemicals Petrochemicals Industries
- Optimization of Calcium Carbonate (Caco) Loading in Natural Rubber Latex Based Disposable GlovesOptimization of Calcium Carbonate (Caco) Loading in Natural Rubber Latex Based Disposable Gloves
- Application of The Transmission Line Model For Porous Electrodes To Analyse The Impedance Response of TiO2 Nanotubes in Physiological EnvironmentApplication of The Transmission Line Model For Porous Electrodes To Analyse The Impedance Response of TiO2 Nanotubes in Physiological Environment
- Physical Science: Title: Formation of Heavy Elements in The UniversePhysical Science: Title: Formation of Heavy Elements in The Universe