Relationship Between Premorbid Functioning and Symptom Severity As Assessed at First Episode of Psychosis
Relationship Between Premorbid Functioning and Symptom Severity As Assessed at First Episode of Psychosis
Uploaded by
aldrin19Copyright:
Available Formats
Relationship Between Premorbid Functioning and Symptom Severity As Assessed at First Episode of Psychosis
Relationship Between Premorbid Functioning and Symptom Severity As Assessed at First Episode of Psychosis
Uploaded by
aldrin19Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Relationship Between Premorbid Functioning and Symptom Severity As Assessed at First Episode of Psychosis
Relationship Between Premorbid Functioning and Symptom Severity As Assessed at First Episode of Psychosis
Uploaded by
aldrin19Copyright:
Available Formats
Article
Relationship Between Premorbid Functioning
and Symptom Severity as Assessed
at First Episode of Psychosis
Jonathan Rabinowitz, Ph.D.
Goedele De Smedt, M.D.
Philip D. Harvey, Ph.D.
Michael Davidson, M.D.
Objective: Investigating the relationship
between premorbid and prodromal status and the clinical manifestations of the
first psychotic episode is relevant for understanding the pathophysiology of psychosis and for improving management of
the disease. This study examined patterns
of premorbid functioning of persons interviewed during their first episode of
psychotic illness and examined the relationship of premorbid characteristics with
symptom severity and cognitive functioning during the first illness episode.
Method: The data were derived from the
baseline assessments of a multicenter international drug trial that enrolled 535
patients in their first episode of psychosis.
Subjects scores on the Premorbid Adjustment Scale were used to assign them to
groups according to whether their premorbid functioning was stablegood, stablepoor, or deteriorating. The three
groups scores on the Positive and Negative Syndrome Scale, Clinical Global Impression (CGI) severity scale, and a cognitive battery were compared.
Results: Almost half of the patients (47.5%)
had stablegood premorbid functioning,
37.3% had stablepoor premorbid functioning, and 15.1% had initially good, but
later deteriorating, premorbid functioning. Compared to the stablepoor and deteriorating groups, the stablegood group
had lower (better) negative syndrome
and general psychopathology scores on
the Positive and Negative Syndrome Scale
and a lower CGI severity scale score. Differences between the stablepoor and
stablegood groups were also found on
some cognitive measures and on the positive syndrome subscale of the Positive
and Negative Syndrome Scale.
Conclusions: More than half of the subjects, who were interviewed during their
first episode of psychotic disorder, had evident premorbid behavioral disturbances.
Poor premorbid functioning before onset
of psychosis was associated with more severe symptoms and more severe cognitive manifestations of illness during the
first illness episode.
(Am J Psychiatry 2002; 159:20212026)
here is consistent evidence that many, but not all,
persons affected by schizophrenia and schizophrenia-like
psychosis manifest poor social adjustment and subtle deviations from cognitive norms much before the illness is
formally diagnosed. However, despite the many studies on
this topic (14), the prevalence, course, characteristics,
and correlates of the premorbid and prodromal impairments are far from clear. By studying the events preceding
the first episode of psychosis and the multiple domains of
psychosocial and educational functioning, it may be possible to detect protective or vulnerability factors and perhaps to devise interventions aimed at secondary prevention such as supplementary educational and vocational
programs and other supportive measures. The goal of this
study was to describe the patterns of premorbid functioning of a large cohort interviewed during their first episode
of psychotic illness and to examine the relationship of premorbid functioning with symptom severity and cognitive
functioning.
Am J Psychiatry 159:12, December 2002
Method
The data presented here were derived from a retrospective premorbid assessment and the baseline assessment of subjects enrolled in a multicenter double-blind, randomized, controlled trial
comparing a typical and a novel antipsychotic drug in the treatment of first-episode psychosis.
Subjects
The trial is being conducted in 11 countries and has enrolled
psychotic patients between the ages of 16 and 45 years who have
had a DSM-IV diagnosis, based on the Structured Clinical Interview for DSM-IV (5), of schizophrenia, schizophreniform disorder, or schizoaffective disorder for less than 12 months and have
had a maximum of two lifetime psychiatric hospitalizations for
psychosis. The cumulative exposure to neuroleptics could not
have exceeded 12 weeks. The study was conducted according to
Good Clinical Practice guidelines and was approved by local institutional review boards. All subjects gave written informed consent before participating in the study.
The final study group included 535 persons (155 female subjects, median age=25.0 years; 380 male subjects, median age=23.8
years). Two persons left the trial before treatment but after random assignment, and 21 patients were excluded because the cen-
2021
PREMORBID FUNCTIONING AND PSYCHOSIS
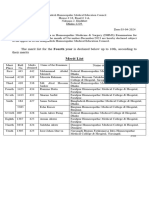
TABLE 1. Retrospectively Rated Premorbid Adjustment Scale Scores for Four Life Stages of Patients With a First Episode of
Psychosis and Healthy Comparison Subjectsa
Patients (N=531)
Life Stage
Childhood (11 years)
Early adolescence (1215 years)
Late adolescence (1618 years)
Adulthood (>18 years)
Most recent life stage
All life stages
Mean
0.28
0.32
0.39
0.42
0.41
0.36
SD
0.18
0.17
0.20
0.24
0.19
0.15
Comparison Subjects
(N=76)b
Mean
0.23
0.21
0.17
0.12
0.09
0.16
SE
0.01
0.01
0.01
0.01
0.01
0.01
Patients With Scores Equal to
or Less Than the Mean Score
for Comparison Subjects
%
42.4
30.5
15.8
13.6
2.8
9.4
Cumulative %
42.4
25.6
10.7
5.2
a Higher scores indicate worse premorbid functioning.
b Means and standard errors resulted from assessment of
the healthy comparison subjects by Cannon-Spoor et al. (6). The comparison subjects
provided the normative data used to validate the Premorbid Adjustment Scale.
ter where they were treated was removed from the trial owing to
inconsistent data reporting. Patients were assigned the following
DSM-IV diagnoses: schizophrenia (N=264), schizophreniform
disorder (N=231), and schizoaffective disorder (N=40). Threequarters of the study group were white (N=400), 12% (N=64) were
black, 3% (N=17) were Hispanic, 2% (N=11) were Oriental, and 8%
(N=43) were from assorted other groups. Fourteen percent (N=76)
of the study group had no high school education, 27% (N=141)
had some high school education, 21% (N=114) completed high
school, 30% (N=159) completed some posthigh school education, and 8% (N=41) completed college. (Data on education were
missing for four subjects.) Female subjects were significantly
older than male subjects at the time they first experienced psychotic symptoms (median=23.9 versus 22.6 years, Mann-Whitney
U=24154, z=2.89, p=0.004). Eighty-eight percent of the patients
(N=471) were 18 or older at the time of onset of first psychotic
symptoms.
Assessments
The current analysis included data from a cognitive assessment and administration of the Premorbid Adjustment Scale (6),
the Positive and Negative Syndrome Scale (7), and the Clinical
Global Impression (CGI) severity scale (8). All measures were applied at baseline before administration of the trial drug.
The Premorbid Adjustment Scale is a 28-item rating scale that
assesses sociability and withdrawal, peer relationships, adaptation to school, and scholastic performance for four life stages
(childhood, 11 years and younger; early adolescence, 1215 years;
late adolescence, 1618 years; and adulthood, older than 18
years), as well as social-sexual aspects of life after age 15. The Premorbid Adjustment Scale also includes a section of nine general
items relating to educational and job achievement, work and
school performance immediately preceding onset of psychosis,
highest level of independence from family, highest level of social
personal adjustment, degree of interest in life, and energy level.
The Premorbid Adjustment Scale was completed on the basis of
all available data, including data from interviews with the patient
and with collateral informants, if they were available.
The cognitive assessment, which is described in greater detail
elsewhere (9), included the 1) Wechsler Memory ScaleRevised
visual reproduction subtest I and II (10), a test of learning memory for nonverbal stimuli; 2) Rey Auditory Verbal Learning Test
(11), a test of verbal learning and memory; 3) Continuous Performance Test, Identical Pairs Version (12), a test of vigilance; 4) verbal fluency examinations, including tests of category and phonological fluency (13), a test of verbal productivity and intactness of
the lexical system; 5) Wechsler Adult Intelligence ScaleRevised,
digit symbol subtest (14), a test of psychomotor speed and attention; and 6) Wisconsin Card Sorting Test (15), a measure of executive functioning (e.g., cognitive flexibility, maintenance of a cognitive set, working memory). The tests, which were carefully
2022
chosen to be adaptable across cultures (9), were translated from
standard English versions into French, Finnish, German, Hebrew,
and Afrikaans and administered to patients in their spoken
language. A central monitoring facility evaluated case record
forms, and all forms with errors were returned for correction. If
the problems were the results of errors in administration, the cognitive testing data on those patients were not included in the
study database.
All investigators were college educated, had previous research
experience, and were fluent in English. Training in administering
the assessment instruments was given in small group sessions at
the local sites, as well as at regional meetings. At the meetings,
videotapes of patient interviews were shown and the investigators filled out a scoring sheet. Individual investigators scores
were then compared against a master scoring sheet developed
by the trainers/developers of the videos. The pass/fail criterion
for the rating examination was based on successfully meeting or
exceeding an 80% concordance with the total and subscale scores
designated on the master rating.
The Premorbid Adjustment Scale was completed for 531 of the
535 subjects, the Positive and Negative Syndrome Scale for 533,
and the cognitive assessment for 508. Complete data on all measures were available for 503 subjects. For the Premorbid Adjustment Scale, the main study measure, data on some items were
missing, as follows: one patient had missing data on one childhood item; two to six patients had missing data on any given early
adolescence item; two to 12 patients had missing data on any
given late adolescence item, with the most data missing on items
relating to social aspects of sexual life during and immediately after adolescence; and nine patients had missing data on two adulthood items, which were filled out only for persons age 19 or older.
On four of the six general items, the maximum number of patients with missing data per item was two. For the item measuring
change in school or work performance before onset, data were
missing for 20 patients. For a similar item measuring job change
and school attendance, data were missing for 18 patients.
Analytic Plan
Data for each of the five Premorbid Adjustment Scale dimensions across the four life stages were analyzed with a repeated
measures analysis of variance (ANOVA), controlling for gender
and diagnosis. A separate general linear model multivariate analysis of variance (GLM MANOVA) was done for each dimension
because all dimensions were not measured at every life stage (e.g.,
social-sexual aspects of life were not measured for childhood, and
adaptation to school was not measured for adults). By using the
scoring method developed by Cannon-Spoor et al. (6), average
scores for each life stage were computed by summing the scores
received for each item in a section and dividing them by the possible score. The sum of the maximum possible score for all items
completed indicates the highest score obtainable. Thus, for exAm J Psychiatry 159:12, December 2002
RABINOWITZ, DE SMEDT, HARVEY, ET AL.
For a normative comparison, we used the normative data provided by Cannon-Spoor et al. (6). The mean score of the normal
subjects was used to create a variable of normal functioning (versus below-normal functioning) in each of the four life stages. Premorbid functioning was described by using the classification
method of Haas and Sweeney (16), which included the following
categories: stablegood, stablepoor, and deteriorating premorbid functioning. Deteriorating premorbid functioning, in terms of
the Premorbid Adjustment Scale, was defined as a pattern of
worsening scores from childhood over the remaining premorbid
periods and the equivalent of a 2-point change over four premorbid stages (childhood, early adolescence, late adolescence, and
adulthood) or a proportional decline for cases in which illness onset was before late adolescence or adulthood. The remaining patients were regarded as stable, and the median value (0.36) of the
Premorbid Adjustment Scale total score was used as a cutoff point
to assign these patients to stablegood or stablepoor groups.
Data for patients were aggregated on this scale of premorbid
functioning, and the three groups were compared on symptom
and cognitive measures by using GLM MANOVA with diagnosis,
sex, and exposure to antipsychotics as factors. Bonferroni-corrected significance levels for between-group differences are reported. The Bonferroni correction consisted of multiplying each
p value by 3, since three comparisons were made (e.g., p=0.05
with Bonferroni correction is presented as p=0.15).
Results
Table 1 presents the subjects mean scores on the Premorbid Adjustment Scale for each life stage. The normative
data on healthy comparison subjects from the work of Cannon-Spoor et al. (6) are also shown in Table 1. The mean
score for childhood for the patients in this study was 0.28,
which was somewhat higher (reflecting worse functioning)
than that for the healthy comparison subjects, who had a
mean score of 0.23. Of the patients in this study, 42.4% had
scores for the childhood period that were no worse than the
mean score for the healthy comparison subjects. The mean
score differences between the patients and the comparison
subjects increased with each successive time period, and
concomitantly the percentage of patients with normal
functioning decreased during subsequent periods. The last
column of Table 1 shows the cumulative percentage of patients who functioned within the normal range for each life
stage and the preceding stages.
Figure 1 presents the patients mean scores on the Premorbid Adjustment Scale across the four life stages assessed. A repeated measures ANOVA comparing these
scores across the life stages found an overall significant
difference and a significant linear trend (decline) on all
five dimensions measured (sociability and withdrawal: F=
32.1, df=3, 1383, p<0.0001 and F=53.2, df=1, 461, p<0.0001;
peer relationships: F=29.6, df=3, 1383, p<0.0001 and F=
47.6, df=1, 461, p<0.0001; scholastic performance: F=35.7,
Am J Psychiatry 159:12, December 2002
FIGURE 1. Retrospectively Rated Scores on Subscales of the
Premorbid Adjustment Scale for Four Life Stages of Patients
With a First Episode of Psychosisa
3.5
Mean Score on Premorbid Adjustment Scale
ample, if a subject received ratings of 2, 3, 3, and 2 for the four
items in the childhood section, the total score for that section
would be 10. The total possible score was 24 (6+6+6+6), and the
total score divided by the possible score was 0.42. When no information was available for a particular item, the item was not
scored. The score for each section was expressed as total score divided by the possible score for the items rated.
Scholastic performance
Peer relationships
Sociability and withdrawal
Adaptation to school
Social-sexual aspects of life
3.0
2.5
2.0
1.5
1.0
011
1215
1618
>18
Age (years)
a
Higher scores indicate worse premorbid functioning.
df=2, 988, p<0.0001 and F=48.8, df=1, 494, p<0.0001; adaptation to school: F=51.5, df=2, 978, p<0.0001 and F=74.6,
df=1, 489, p<0.0001; and social-sexual aspects: F=32.7, df=
2, 878, p<0.0001 and F=47.5, df=1, 439, p<0.0001).
Using the method of Haas and Sweeney (16), 47.5% of
the subjects (N=252) were categorized as having stable
good premorbid functioning; 37.3% (N=198) as having stablepoor functioning; and 15.3% (N=81) as having deteriorating premorbid functioning. Although the Haas scale is
based on a different method of computation (described in
detail in the section on data analysis) than the method
used to compare the overall group of patients to the comparison subjects, the stablegood group had mean scores
that were similar to those of the comparison subjects (reported in Table 1) for childhood and early adolescence
(childhood: 0.19 and 0.23, respectively; early adolescence:
0.21 and 0.21, respectively) and different from those of the
comparison subjects for late adolescence and adulthood
scores (late adolescence: 0.24 versus 0.17; adulthood: 0.24
versus 0.12).
Female subjects had significantly better premorbid
functioning (stablegood: 57%, N=88; stablepoor: 34%,
N=53; deteriorating: 9%, N=14) than male subjects (stablegood: 44%, N=164; stablepoor: 18%, N=67; deteriorating 39%, N=145) (2=10.1, df=2, p=0.006). Patients with
a diagnosis of schizophreniform disorder had better premorbid functioning (stablegood: 62%, N=143; stable
poor: 27%, N=61; deteriorating: 11%, N=25) than those
2023
PREMORBID FUNCTIONING AND PSYCHOSIS
TABLE 2. Scores on Measures of Symptom Severity and Cognitive Functioning of Patients With a First Episode of Psychosis,
by Type of Premorbid Functioninga
Patients With Stable
Good Premorbid
Functioning (N=252)
Patients With
Deteriorating
Premorbid
Functioning (N=81)
Patients With Stable
Poor Premorbid
Functioning (N=198)
Mean
95% CI
Mean
95% CI
Mean
95% CI
Measure
Symptom severity c
Positive and Negative Syndrome Scale
Positive syndrome score
19.8
18.820.7
20.5
19.022.0
21.1
20.122.1
Negative syndrome score
19.9
18.821.0
24.0
22.325.6
23.0
22.024.2
General psychopathology score
39.2
37.540.8
42.4
39.945.0
42.7
41.044.5
Clinical Global Impression severity scale score
4.5
4.34.6
4.6
4.44.8
4.7
4.54.8
Cognitive functioning d
Wechsler Memory ScaleRevised visual reproduction
Immediate recall score
31.5
30.332.8
32.0
30.033.9
29.9
28.631.2
Delayed recall score
28.1
26.429.7
27.7
25.230.3
25.2
23.527.0
Rey Auditory Verbal Learning Test score
44.5
42.446.9
46.8
43.650.1
42.9
40.745.1
Continuous Performance Test
0.8
0.60.9
1.0
0.81.2
0.7
0.60.8
Verbal fluency examinations
Category total score
39.0
37.141.1
41.4
38.444.4
37.4
35.439.5
Letter total score
31.3
29.032.8
31.2
28.234.3
30.3
28.232.4
Wechsler Adult Intelligence Scale-Revised digit symbol test score
45.6
43.247.9
49.0
45.452.7
44.9
42.447.3
Wisconsin Card Sorting Test
Categories
4.3
3.94.7
4.3
3.74.9
3.7
3.34.0
41.2
36.945.4
38.5
32.045.0
48.1
43.752.5
Total errors
a Premorbid functioning was defined in terms of Premorbid Adjustment Scale scores, according to the typology of Haas and Sweeney (16).
Deteriorating functioning was a pattern of worsening Premorbid Adjustment Scale scores from childhood over the remaining premorbid life
stages and the equivalent of a 2-point change over the four premorbid life stages or a proportional decline for patients whose illness onset
was before late adolescence or adulthood. Patients without this pattern were regarded as stable; the median value (0.36) of the Premorbid
Adjustment Scale total score was used as a cutoff point to assign these patients to the stablegood or the stablepoor group.
b Bonferroni correction done by multiplying t test significance level by 3, since three comparisons were made.
c Significant difference between groups in overall symptom severity (F=4.0, df=8, 1038, p<0.0001).
d Significant difference between groups in overall cognitive functioning (F=1.7, df=18, 850, p=0.03).
with schizoaffective disorder (stablegood: 40%, N=16;
stablepoor: 48%, N=19; deteriorating: 13%, N=5) or
schizophrenia (stablegood: 36%, N=93; stablepoor:
45%, N=118; deteriorating 19%, N=51) ( 2 =37.6, df=4,
p<0.006).
Table 2 presents mean scores on the Positive and Negative Syndrome Scale and cognitive measures for the patients with stablepoor, stablegood, and deteriorating
premorbid functioning. Overall there were significant differences in both symptoms and cognition (multivariate
tests presented in footnotes c and d of Table 2). Significant differences were found in the Positive and Negative
Syndrome Scale negative syndrome and general psychopathology scores. Nearly significant differences were
found in the Positive and Negative Syndrome Scale positive syndrome score and the CGI severity scale score. Significant differences were found on six of the nine cognitive
measures, and the difference between groups for one
more cognitive measure was nearly significant. The patients classified as having stablegood premorbid functioning had significantly better scores on the Positive and
Negative Syndrome Scale negative syndrome, positive
syndrome, and general psychopathology subscales, on the
CGI severity scale, and on three cognitive measures, compared to the stablepoor group. Similarly, the stablegood
group had significantly better scores than the deteriorating group on the Positive and Negative Syndrome Scale
negative and general psychopathology subscales and the
2024
CGI, and significantly worse scores on one cognitive measure. The stablepoor group had significantly worse performance on three cognitive measures, compared to the
deteriorating group, but the scores on the CGI and Positive
and Negative Syndrome Scale were not different between
those groups.
Discriminant function analysis with the stepwise procedure based on Wilkss lambda was conducted to examine
the relative importance of scores on the Positive and Negative Syndrome Scale subscales, the CGI, and the cognitive
variables in discriminating between the three types of premorbid adjustment. The two variables that significantly
discriminated between the groups were the Positive and
Negative Syndrome Scale negative subscale score, which
was the first variable entered in the model (F=18.9, df=2,
434, p<0.0001), and the score on the category test of the
verbal fluency examinations, which was the second variable added to the model (F=12.3, df=4, 866, p<0.0001).
Discussion
More than half of the subjects in this study, who were experiencing a first episode of psychosis, had some disturbances long before the episode. Although 88% of the patients had onset of psychosis after age 18, 84% showed a
disturbance in functioning, relative to the functioning of
normal comparison subjects, before age 18, almost 70%
before age 15, and 58% before age 11. Poorer premorbid
Am J Psychiatry 159:12, December 2002
RABINOWITZ, DE SMEDT, HARVEY, ET AL.
Analysis
Between-Group Differences (p)b
2.6
15.4
7.0
2.6
df
0.003
<0.0001
<0.0001
0.001
0.23
<0.0001
0.008
0.06
1.00
0.76
1.00
1.00
0.05
0.02
0.08
0.007
0.10
0.04
0.51
1.00
1.00
1.00
0.77
0.01
0.14
0.22
0.11
0.004
3.0 2, 439
0.4 2, 439
2.2 2, 439
0.05
0.68
0.11
0.94
1.00
1.00
0.28
1.00
0.4
0.06
1.00
0.20
4.9 2, 439
5.1 2, 439
0.008
0.006
0.02
0.05
1.00
1.00
0.10
0.02
3.0
4.1
2.6
5.0
2, 528 0.08
2, 528 <0.0001
2, 528 <0.0001
2, 528 0.07
StableGood StableGood Deteriorating
Versus
Versus
Versus
StablePoor Deteriorating StablePoor
2, 439
2, 439
2, 439
2, 439
functioning long before onset of psychosis was associated
with more severe manifestations of illness at the first psychotic episode, both in terms of symptoms and cognitive
functioning. The results presented here are consistent
with reports indicating that deviations in functioning, particularly in social adjustment, are present in many, but not
all, individuals affected by psychosis and schizophrenia
long before the psychotic illness is formally diagnosed or
even manifested (14). The deviations can take the form of
poor interpersonal relationships, withdrawal behavior, eccentricity, or even attenuated psychotic symptoms. For
some individuals, these deviations might manifest as shyness and poor scholastic achievement during childhood,
continuing as a crescendo of progressive deterioration
during adolescence. For others, the deviations may be
barely detectable, manifesting as few putative behavioral
abnormalities shortly before the diagnosis of the first psychotic episode.
Furthermore, the transitions from premorbid to prodromal manifestations and then to the emergence of the
symptoms that define the first episode of psychosis and the
subsequent diagnosis are not always clearly distinct points
in time or distinctive illness-related events. Family structure and education or access to care might affect when the
diagnosis occurs (1719), hence determining the length of
the premorbid and prodromal manifestations as well as
determining which manifestations are classified as premorbid, prodromal, or part of the first psychotic episode.
Am J Psychiatry 159:12, December 2002
The results presented here indicate that, as a group, individuals affected by psychosis are likely to show continuous deterioration of social functioning from childhood
through adolescence, as the first episode of psychosis approaches. However, only 15% of the subjects (those with
deteriorating premorbid functioning) showed a clear transition from a higher to a lower level of social functioning.
Hence the data lend tentative support to the existence of a
subgroup of patients with gradual premorbid social deterioration and a subgroup who lack developmental progress.
Limitations of the data in this study and previous studies may account for the variation in findings about the
quality and timing of premorbid manifestations. The data
were limited in part because they were derived from crosssectional assessments conducted at the patients first contact with a mental health professional (20). In addition,
the data were based on the subjective recollections of a variety of sources, including the patient, family members,
and other collateral informants. It is conceivable that a
true prospective follow-up study, specifically designed to
detect signs of premorbid psychosis and schizophrenia
and conducted from birth through age of risk, would reveal a specific trajectory of social maladjustment for the
majority of individuals destined to be affected by psychosis. Alternately, the premorbid and prodromal manifestations may be obligatory precursors of the illness for only
some individuals or for only a subgroup of the schizophrenias. Another limitation of this study is the potential for a
selection bias, given that the data were obtained from patients who agreed to be enrolled in a medication trial.
However, it is not obvious how such a bias might affect the
conclusions that can be drawn from the study.
In this study, approximately half of a group of subjects
with a first episode of psychosis retrospectively reported
poor premorbid social adjustment. This finding is consistent with data that have been collected prospectively. In a
prospective historical study in which social adjustment
was assessed in apparently healthy adolescents, poor social adjustment was reported regarding as many as 44% of
subjects assigned a diagnosis of schizophrenia 1 or more
years (mean=4 years), compared to only 7% of the subjects
of the same age who remained healthy (21). This finding
supports the accuracy of the prevalence of premorbid
maladjustment reported in this study.
The results of this study are consistent with previous reports about first-episode schizophrenia. Most studies in
this area have found that individuals with poorer (as opposed to better) premorbid functioning also have more severe symptoms, as reflected by the negative syndrome
subscale of the Positive and Negative Syndrome Scale and
the CGI, as well as worse cognitive performance, as measured with standard neuropsychological tests. The relationships between the Premorbid Adjustment Scale scores
and the Positive and Negative Syndrome Scale, CGI, and
cognitive scores can be interpreted in a number of ways.
The different scales may assess similar domains, or there
2025
PREMORBID FUNCTIONING AND PSYCHOSIS
may be overlap between scales in the content of individual
scale items. Scoring on one scale could be affected by
scoring on another scale, particularly if the two scales are
scored during the same session by the same rater.
Alternatively, a particular subgroup of schizophrenic
disorders may be defined by an early pathophysiological
process that manifests as poor social adjustment during
childhood and adolescence. This process may then evolve
into more severe negative and general symptoms, as well
as poorer cognitive performance in early adulthood and at
the onset of psychosis. A number of scenarios could be responsible for these pathophysiological processes. An accumulation of genetic and environmental risk factors (or
lack of environmental protective factors), consistent with
a multiple-hit hypothesis, may lead to the premorbid
manifestations, and an environmental insult or a gene expressed later in life may be necessary for the full syndrome
of schizophrenia to develop. Depending on the nature of
the additional, later insults, the same early-life manifestations (e.g., marginal social adjustment) might remain stable through life, evolve into milder mental disorders such
as schizotypal personality disorder, or lead to schizophrenia. If indeed the phenotype of schizophrenia reflects the
consequences of an accumulation of genetic and environmental risk factors, research examining the course of the
disease from birth through the age of risk may be required
to identify specific etiological patterns.
Received Dec. 6, 2001; revision received May 16, 2002; accepted
May 23, 2002. From the Department of Social Work, Bar-Ilan University; Janssen Research Foundation, Beerse, Belgium; Mt. Sinai School
of Medicine, New York; and Chaim Sheba Medical Center, Tel
Hashomer, Israel. Address reprint requests to Dr. Rabinowitz, Department of Social Work, Bar-Ilan University, Ramat Gan, Israel;
rabinowz@mail.biu.ac.il (e-mail).
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
References
1. Mohamed S, Paulsen JS, OLeary D, Arndt S, Andreasen N: Generalized cognitive deficits in schizophrenia: a study of first-episode patients. Arch Gen Psychiatry 1999; 56:749754
19.
2. Russell AJ, Munro JC, Jones PB, Hemsley DR, Murray RM: Schizophrenia and the myth of intellectual decline. Am J Psychiatry
1997; 154:635639
20.
3. David AS, Malmberg A, Brandt GL, Allenbeck P, Lewis G: IQ and
risk for schizophrenia: a population-based cohort study. Psychol Med 1997; 27:13111323
21.
4. Rabinowitz J, Reichenberg A, Weiser M, Mark M, Kaplan Z,
Davidson M: Cognitive and personality functioning during the
2026
decade prior to first hospitalization and early course of psychotic illness. Br J Psychiatry 2000; 177:2632
First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders (SCID), Clinician Version. Washington, DC, American Psychiatric Press, 1996
Cannon-Spoor H, Potkin G, Wyatt J: Measurement of premorbid
adjustment in chronic schizophrenia. Schizophr Bull 1982; 8:
470484
Kay SR, Singh MM: The positive-negative distinction in drugfree schizophrenic patients: stability, response to neuroleptics,
and prognostic significance. Arch Gen Psychiatry 1989; 46:
711718
Guy W (ed): ECDEU Assessment Manual for Psychopharmacology: Publication ADM 76-338. Washington, DC, US Department
of Health, Education, and Welfare, 1976, pp 218222
Harvey PD, Artiola L, DeSmedt G: Cross national cognitive assessment in schizophrenia clinical trials: a feasibility study.
Schizophr Res 2002 (in press)
Wechsler D: The Wechsler Memory ScaleRevised. San Antonio, Tex, Psychological Corp, 1987
Spreen O, Strauss E: A Compendium of Neuropsychological
Tests and Norms. New York, Oxford University Press, 1998
Cornblatt BA, Lenzenweger MF, Erlenmeyer-Kimling L: The
Continuous Performance Test, Identical Pairs Version, II: contrasting attentional profiles in schizophrenic and depressed
patients. Psychiatry Res 1989; 29:6585
Lezak MD: Neuropsychological Assessment. New York, Oxford
University Press, 1997
Wechsler D: The Wechsler Adult Intelligence ScaleRevised.
New York, Psychological Corp, 1978
Heaton R, Chelune C, Talley J, Kay G, Curtiss G: Wisconsin Card
Sorting Test ManualRevised and Expanded. Odessa, Fla, Psychological Assessment Resources, 1993
Haas GL, Sweeney JA: Premorbid and onset features of first-episode schizophrenia. Schizophr Bull 1992; 18:373386
Bhugra D, Hilwig M, Mallett R, Corridan B, Leff J, Neehall J,
Rudge S: Factors in the onset of schizophrenia: a comparison
between London and Trinidad samples. Acta Psychiatr Scand
2000; 101:135141
Hinrichsen GA, Lieberman JA: Family attributions and coping
in the prediction of emotional adjustment in family members
of patients with first-episode schizophrenia. Acta Psychiatr
Scand 1999; 100:359366
Varma VK, Wig NN, Phookun HR, Misra AK, Khare CB, Tripathi
BM, Behere PB, Yoo ES, Susser ES: First-onset schizophrenia in
the community: relationship of urbanization with onset, early
manifestations and typology. Acta Psychiatr Scand 1997; 96:
431438
McGlashan TH: A selective review of recent North American
long-term follow-up studies of schizophrenia. Schizophr Bull
1988; 14:515542
Davidson M, Reichenberg A, Rabinowitz J, Weiser M, Kaplan Z,
Mark M: Behavioral and intellectual markers for schizophrenia
in apparently healthy male adolescents. Am J Psychiatry 1999;
156:13281335
Am J Psychiatry 159:12, December 2002
You might also like
- LSP 16Document3 pagesLSP 16Ching OBNo ratings yet
- Psych Consult TemplateDocument4 pagesPsych Consult TemplateJagdishVankarNo ratings yet
- Test Bank For Medical Surgical Nursing Critical Thinking in Client Care 4th Edition Priscilla LeMonDocument307 pagesTest Bank For Medical Surgical Nursing Critical Thinking in Client Care 4th Edition Priscilla LeMonkanooj khan100% (1)
- Organization and Presentation of Psychiatric InformationDocument6 pagesOrganization and Presentation of Psychiatric InformationRoci ArceNo ratings yet
- Altman Self Rating ScaleDocument2 pagesAltman Self Rating ScaleRifkiNo ratings yet
- Developmental History FormDocument2 pagesDevelopmental History FormocramusNo ratings yet
- Clinical Interview and ObservationDocument47 pagesClinical Interview and Observationmlssmnn100% (2)
- Challenging Behaviours (Power Point)Document17 pagesChallenging Behaviours (Power Point)tamNo ratings yet
- CV ChescklostDocument31 pagesCV ChescklostMahendra BandsodeNo ratings yet
- Child and Adolescent Behavioral Health: A Resource for Advanced Practice Psychiatric and Primary Care Practitioners in NursingFrom EverandChild and Adolescent Behavioral Health: A Resource for Advanced Practice Psychiatric and Primary Care Practitioners in NursingEdilma L. YearwoodNo ratings yet
- Assessment Questionnaire GuideDocument7 pagesAssessment Questionnaire GuideKasandra Dawn Beriso100% (1)
- Violence Risk Assessment NotesDocument7 pagesViolence Risk Assessment NotesTalib9876No ratings yet
- Columbia Suicide Severity Rating Scale Screen VersionDocument2 pagesColumbia Suicide Severity Rating Scale Screen VersionPaul SmithNo ratings yet
- Suicide Risk Assessment Summary.08Document1 pageSuicide Risk Assessment Summary.08Pintiliciuc-aga MihaiNo ratings yet
- 326 Mental - Status - Examination Directions and RubricDocument4 pages326 Mental - Status - Examination Directions and RubricTommieNo ratings yet
- Chapter 2 Conceptualizing Abnormal Psychology PDFDocument67 pagesChapter 2 Conceptualizing Abnormal Psychology PDFGabriel Jeremy Ortega100% (1)
- G CBT For DelusionDocument23 pagesG CBT For DelusionIoana DarjanNo ratings yet
- Symptoms: Following SignsDocument3 pagesSymptoms: Following SignsAhmed FaidNo ratings yet
- Clinical Manifestations, Differential Diagnosis, and Initial Management of Psychosis in AdultsDocument16 pagesClinical Manifestations, Differential Diagnosis, and Initial Management of Psychosis in AdultsJohan ValderramaNo ratings yet
- Malingering On The Personality Assessment Inventory: Identification of Specific Feigned DisordersDocument7 pagesMalingering On The Personality Assessment Inventory: Identification of Specific Feigned DisordersMissDSKNo ratings yet
- CDI Patient VersionDocument9 pagesCDI Patient VersionalotfyaNo ratings yet
- Intervention, Management of HallucinationDocument52 pagesIntervention, Management of HallucinationAshish_Singh_5126100% (1)
- Carlat, Daniel J. - The Psychiatric Interview-Wolters Kluwer (2017) Cap 1 A 6. Páginas 20 - 54Document35 pagesCarlat, Daniel J. - The Psychiatric Interview-Wolters Kluwer (2017) Cap 1 A 6. Páginas 20 - 54Juan PabloNo ratings yet
- (MMPI) : The Minnesota Multiphasic Personality InventoryDocument22 pages(MMPI) : The Minnesota Multiphasic Personality InventoryKate BumatayNo ratings yet
- Lecture 5-Mood disordersPDF - 240228 - 203457Document47 pagesLecture 5-Mood disordersPDF - 240228 - 203457hui xin ng100% (1)
- Assessment and Evaluation: 2008 Edition Rhoda K Hahn, MD Lawrence J. Albers, MDDocument85 pagesAssessment and Evaluation: 2008 Edition Rhoda K Hahn, MD Lawrence J. Albers, MDAlbghdadi CristianNo ratings yet
- Malingering Clinical PresentationDocument5 pagesMalingering Clinical Presentationbuckley12120850% (1)
- Defense Mechanisms and Personality DisordersDocument32 pagesDefense Mechanisms and Personality DisordersHigo100% (2)
- Provisional Diagnosis: Differential DiagnosesDocument7 pagesProvisional Diagnosis: Differential Diagnoseshernandez2812No ratings yet
- Chapter 5 Anxiety Trauma and Stressor Related and Obsessive Compulsive and Related DisorderDocument43 pagesChapter 5 Anxiety Trauma and Stressor Related and Obsessive Compulsive and Related DisorderGabriel Jeremy OrtegaNo ratings yet
- Template For History in PsychiatryDocument3 pagesTemplate For History in PsychiatryDeedz01100% (1)
- Antisocial PersonalitiesDocument20 pagesAntisocial PersonalitiesTiberiu CutitNo ratings yet
- Somatoform DisordersDocument57 pagesSomatoform Disorderscoolblue89No ratings yet
- The Clinical Assessment Interview For Negative SymDocument9 pagesThe Clinical Assessment Interview For Negative SymJohanes DavidNo ratings yet
- Parwhitepaper-Spectra 19Document21 pagesParwhitepaper-Spectra 19Samuel BallouNo ratings yet
- Psychiatric Rating Scales-RRFINALDocument45 pagesPsychiatric Rating Scales-RRFINALnkivc100% (2)
- Mental Health Plan Assessment Form: Relationship PhoneDocument6 pagesMental Health Plan Assessment Form: Relationship Phonealotfya100% (1)
- 21.cpsy.034 Icd-10&dsm-5Document8 pages21.cpsy.034 Icd-10&dsm-5Victor YanafNo ratings yet
- Clinical Psychology, Nature, Development and Activities of Clinical Psychologist (MAPSY 202)Document12 pagesClinical Psychology, Nature, Development and Activities of Clinical Psychologist (MAPSY 202)Sandhya Choudhary0% (1)
- Clinical Case FormulationDocument5 pagesClinical Case FormulationLaura GomezNo ratings yet
- Psych Case StudyDocument14 pagesPsych Case StudySmridhi Seth100% (1)
- Comorbidity of Borderline 2018Document11 pagesComorbidity of Borderline 2018Dhino Armand Quispe SánchezNo ratings yet
- Early Maladaptive SchemasDocument4 pagesEarly Maladaptive SchemasRoberto SzenczukNo ratings yet
- Personality Disorder English 2011 EditDocument31 pagesPersonality Disorder English 2011 EditNyoman Dianita CandradewiNo ratings yet
- Modified Mini ScreenDocument5 pagesModified Mini ScreenPriya PuriNo ratings yet
- PSYCH 001 Psychiatric Interview of The Medically Ill PDFDocument10 pagesPSYCH 001 Psychiatric Interview of The Medically Ill PDFKaye Nee100% (1)
- Provisional DiagnosisDocument10 pagesProvisional DiagnosisVanessa DiazNo ratings yet
- The Management of Acute DystonicDocument2 pagesThe Management of Acute DystonictaqinosNo ratings yet
- PintoOCPDtreatmentchapter PDFDocument16 pagesPintoOCPDtreatmentchapter PDFSabrina HortopanNo ratings yet
- Child DisordersDocument111 pagesChild Disorderspriyanka raj100% (1)
- Psychodynamic Psychiatry, 6-Minute 2018Document13 pagesPsychodynamic Psychiatry, 6-Minute 2018Dhino Armand Quispe SánchezNo ratings yet
- Schizophrenia Spectrumand Other Psychotic Disorders MINDMAPSDocument5 pagesSchizophrenia Spectrumand Other Psychotic Disorders MINDMAPSecheers.csflNo ratings yet
- Adjustment DisorderDocument4 pagesAdjustment DisorderRosalba GiovannelliNo ratings yet
- Early PsychosisDocument118 pagesEarly Psychosissolomon1234567100% (2)
- Mental Status Exam (Adult) - JMCDocument35 pagesMental Status Exam (Adult) - JMCMohamad Faizul Abu HanifaNo ratings yet
- Chapter 1 Developmental PsychopathologyDocument30 pagesChapter 1 Developmental PsychopathologyLAVANYA M PSYCHOLOGY-COUNSELLINGNo ratings yet
- 3.psychiatric HX and MSE (1) According To DSM-5Document96 pages3.psychiatric HX and MSE (1) According To DSM-5sopsychaNo ratings yet
- Psych History TemplateDocument4 pagesPsych History TemplateChloe Gotera100% (1)
- Psychiatric Diagnosis: Challenges and ProspectsFrom EverandPsychiatric Diagnosis: Challenges and ProspectsIhsan M. SalloumRating: 5 out of 5 stars5/5 (1)
- Comprehensive Handbook of Psychological Assessment, Volume 1: Intellectual and Neuropsychological AssessmentFrom EverandComprehensive Handbook of Psychological Assessment, Volume 1: Intellectual and Neuropsychological AssessmentNo ratings yet
- Ethical Issues in Clinical Forensic PsychiatryFrom EverandEthical Issues in Clinical Forensic PsychiatryArtemis IgoumenouNo ratings yet
- Untitled DocumentDocument16 pagesUntitled Documentrobymuiruri42No ratings yet
- Introduction R&ADocument12 pagesIntroduction R&AMyasser SoubNo ratings yet
- Surgical Pearl: Ligation of The Base of Pyogenic Granuloma-An Atraumatic, Simple, and Cost-Effective ProcedureDocument2 pagesSurgical Pearl: Ligation of The Base of Pyogenic Granuloma-An Atraumatic, Simple, and Cost-Effective ProceduregabbynengNo ratings yet
- First Aid For Common InjuriesDocument1 pageFirst Aid For Common InjuriesMohammed MinhajNo ratings yet
- 18 - First Aid in Electrical InjuriesDocument39 pages18 - First Aid in Electrical InjuriesIsael sierraNo ratings yet
- WHO EURO 2023 7452 47219 69202 EngDocument60 pagesWHO EURO 2023 7452 47219 69202 EnglegalegawatiNo ratings yet
- Stainless Steel Crowns SSC-Primary and Permanent: Shan Lal, Dds Director, Pre-Clinical Programs Pediatric DentistryDocument4 pagesStainless Steel Crowns SSC-Primary and Permanent: Shan Lal, Dds Director, Pre-Clinical Programs Pediatric DentistryfradmardNo ratings yet
- Ischemic Heart DiseaseDocument55 pagesIschemic Heart DiseaseAndrassy Twinkle AlineaNo ratings yet
- Treatment of Obesity: Strategies For Weight LossDocument3 pagesTreatment of Obesity: Strategies For Weight LossHumanyu KabeerNo ratings yet
- Nutrients and Botanicals For Erectile Dysfunction: Examining The EvidenceDocument13 pagesNutrients and Botanicals For Erectile Dysfunction: Examining The EvidencefinaNo ratings yet
- Alzheimers Disease Power Point Presentation FileDocument10 pagesAlzheimers Disease Power Point Presentation Filejoseph ndung'uNo ratings yet
- Laminitis - Prevention, Diagnosis and Treatment PDFDocument10 pagesLaminitis - Prevention, Diagnosis and Treatment PDFfrankyNo ratings yet
- Identify Etiology of Morbidity Events of Earlier Children Among Multigravida Women.Document11 pagesIdentify Etiology of Morbidity Events of Earlier Children Among Multigravida Women.snehal DharmadhikariNo ratings yet
- D5W (Dextrose 5%) ClassDocument4 pagesD5W (Dextrose 5%) ClassHanilyn ArdinaNo ratings yet
- UpchaarDocument3 pagesUpchaarresh_jagdaleNo ratings yet
- IHU - Company Profile (Update Oct 2022)Document10 pagesIHU - Company Profile (Update Oct 2022)Sherly ThendianNo ratings yet
- DextroseDocument1 pageDextroseAdrianne BazoNo ratings yet
- Humphery and FDT InterpretationDocument46 pagesHumphery and FDT Interpretationhenok birukNo ratings yet
- Survival CancerDocument96 pagesSurvival CancerIva Jelić StanojevićNo ratings yet
- AF (CHADSVASC-HASbled)Document1 pageAF (CHADSVASC-HASbled)Giorgi NanetashviliNo ratings yet
- Essential Messages - 2023 ACSDocument16 pagesEssential Messages - 2023 ACSimran karimNo ratings yet
- Kuesioner MrsDocument1 pageKuesioner MrsAyu WeningNo ratings yet
- Diagnostic Approach To and Treatment of Thyroid Nodules - UpToDate PDFDocument36 pagesDiagnostic Approach To and Treatment of Thyroid Nodules - UpToDate PDFDANIEL SANTAMARIANo ratings yet
- JURNAL RS KELOMPOK - YOLLA ANDRIANI - 2243700044 Revisi 11 Juli 2023Document6 pagesJURNAL RS KELOMPOK - YOLLA ANDRIANI - 2243700044 Revisi 11 Juli 2023Dini Permata SariNo ratings yet
- Notification NLC Recruitment Executive VacanciesDocument4 pagesNotification NLC Recruitment Executive VacanciesYogesh DagarNo ratings yet
- 4th Year 2022Document26 pages4th Year 2022Mehedi HasanNo ratings yet
- Individual Application Form For Registration of Dependants V302 20220302 InteractiveDocument8 pagesIndividual Application Form For Registration of Dependants V302 20220302 InteractiveTsundzuka KhosaNo ratings yet
- Members Application Form: Name & Surname ID NumberDocument8 pagesMembers Application Form: Name & Surname ID NumberJacques MorrisonNo ratings yet