Laboratory - Handbook - For - Clinicians Rearding HIV Testing SMS Medical College, Jaipur
Laboratory - Handbook - For - Clinicians Rearding HIV Testing SMS Medical College, Jaipur
Uploaded by
dileep2000Copyright:
Available Formats
Laboratory - Handbook - For - Clinicians Rearding HIV Testing SMS Medical College, Jaipur
Laboratory - Handbook - For - Clinicians Rearding HIV Testing SMS Medical College, Jaipur
Uploaded by
dileep2000Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Laboratory - Handbook - For - Clinicians Rearding HIV Testing SMS Medical College, Jaipur
Laboratory - Handbook - For - Clinicians Rearding HIV Testing SMS Medical College, Jaipur
Uploaded by
dileep2000Copyright:
Available Formats
HIV Test Laboratory, Department of Microbiology, SMS Medical College, Jaipur.
HIV TEST LABORATORY
DEPARTMENT OF MICROBIOLOGY
SAWAI MANSINGH MEDICAL COLLEGE, JAIPUR
HIV
Laboratory Handbook for Clinicians
Issue No.: 01
Issue Date: November 5th 2012
Prepared by: Dr. Babita Sharma
Approved & issued by: Dr. Nitya Vyas
Document Name: Laboratory Hand Book for Clinician
Document No.: SMS/MICRO/HIV/LHC/10
Page No.0 | 8
Amendment Number :
Amendment Date:
Version No.- 01
HIV Test Laboratory, Department of Microbiology, SMS Medical College, Jaipur.
Introduction
HIV/AIDS is not like other infectious diseases. It is far more complex because HIV infection
cannot be diagnosed clinically in asymptomatic as well as symptomatic individuals. Person is
infectious and infected for life. Outcome is invariable fatal and no cure or vaccine is available so far.
Commonly HIV/AIDS is acquired through sexual contact, individuals known to be HIV infected are
stigmatized and discriminated.
HIV testing is not mandatory and it should not be imposed for providing healthcare services and
facilities. Any HIV testing must be accompanied by pre test and post test counseling services and
informed consent. Confidentiality of the results should be maintained1.
In 50-93% of cases primary HIV infection is asymptomatic. Laboratory diagnosis is the only
method for determining HIV status of such individuals. A number of tests and diagnostic kits are
available to assess the HIV status of individuals. Serological tests are most commonly performed
Objectives of HIV testing
Diagnosis of HIV infection in clinically suspected individuals.
To Diagnose asymptomatic individuals (practicing high risk behavior)
Prevention of parent to child transmission
For tissue transfusion safety (blood, sperms, organs etc)
Sentinel surveillance to monitor epidemiological trends.
Research
Services Offered
All the services offered at the HIV Test Laboratory are free of cost. Services being provided at HIV
Test Laboratory are
Counseling about HIV/AIDS
Testing of HIV antibody: Walk inpatient, Provider initiated referred patients.
CD4+ T Lymphocyte count for patients referred from ART Center.
Dried blood spot (DBS) collection for HIV exposed child.
Clinical Sample Required
Document Name: Laboratory Hand Book for Clinician
Document No.: SMS/MICRO/HIV/LHC/10
Page No.1 | 8
Amendment Number :
Amendment Date:
Version No.- 01
HIV Test Laboratory, Department of Microbiology, SMS Medical College, Jaipur.
We prefer to collect sample at our center:
For HIV antibody Testing: 3-5 ml blood/ 1ml serum in sterile plain vial.
For CD4+ T Lymphocyte count: 2 ml blood in K2/K3 EDTA vial.
Dried blood spot (DBS) is collected at HIV Test Laboratory
Sample collection
1st April to 30th September
From 8.00 am to 11 am & 11.30 am to 12.30 pm.
1st October to 31st March
From 9.00 am to12 noon & 12.30 pm to 1.30 pm
Report Distribution
1st April to 30th September:
Samples received from 8.00 am to 11.00 am are reported on same day between 1-2 pm.
Samples received between 11.30 am to 12.30 pm are reported on next working day between
11.30 am to 12 noon.
1st October to 31st March:
Samples received from 9.00 am to 12.00 noon are reported on same day between 2- 3 pm.
Samples received between 12.30 noon to 1.30 pm are reported on next working day between
12.30 pm -1 pm.
Reports are available with Counselors.
Laboratory diagnosis during window period
The window period is the period of time between initial infection with HIV and the time when HIV
antibodies can be detected in the blood (3-12 weeks). A blood test performed during the window
period may yield negative test result for HIV antibodies. HIV infection during window period can be
detected by demonstrating the presence of virus and virus components. Detection of p24 antigen and
PCR for viral products may be helpful during window period.
Counseling
Document Name: Laboratory Hand Book for Clinician
Document No.: SMS/MICRO/HIV/LHC/10
Page No.2 | 8
Amendment Number :
Amendment Date:
Version No.- 01
HIV Test Laboratory, Department of Microbiology, SMS Medical College, Jaipur.
Counseling is a confidential dialogue between client and a counselor to provide information on
HIV/AIDS and bringing about behavior change in the client. It is also aimed at enabling the client to
take the decision regarding HIV testing and to understand the implication of the test results.2
HIV testing is accompanied with pre and post test counseling. The pre test counseling involves
provision of basic information on HIV/ AIDS and risk assessment to direct walk in client while in post
test counseling the client is helped to understand and cope with the HIV test results.
In case of a negative test result the counselor reiterates basic information on HIV and assists the
client to adopt behaviors that reduces the risk of getting infected with HIV in future. In case the client
is in the window period as per history a repeat test is recommended.
In case of a positive test result the counselor assists the client to understand the implication of the
positive test results and help in coping with the test results. With this counselor also refer the patient to
ART, and other services for care and support.
Samples are collected after pre test counseling and informed consent of the patients.
Collected samples are accepted only when they are accompanied with completely filled requisition
forms and informed consent of patient.
HIV Testing
In HIV Test Laboratory HIV antibodies are detected by Rapid and ELISA method as per kits
available.
CD4 T+ lymphocytes count is done by BD FACS Calibur through flow cytometery.
The DBS samples are sent to All India Institute of Medical Sciences, Delhi (AIIMS) for DNA
PCR test.
In HIV test laboratory diagnosis of HIV is done according to NACO strategies.
For diagnosis of HIV, the laboratory performs 3 tests with different principle or different
antigen. The kits for these are supplied by RSACS, which are approved by NACO.
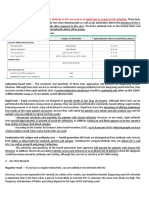
Strategy IIB
Document Name: Laboratory Hand Book for Clinician
Document No.: SMS/MICRO/HIV/LHC/10
Page No.3 | 8
Amendment Number :
Amendment Date:
Version No.- 01
HIV Test Laboratory, Department of Microbiology, SMS Medical College, Jaipur.
For patients with AIDS defining diseases
I Test (HIV antibody Test)
Non Reactive
Reactive
Report Negative for HIV antibody
II Test different in principle or antigen from first test
____________________________________________________
Non Reactive
Reactive
Report Positive for HIV antibody
III Test different in principle or antigen from I & II test
____________________________________________
Non Reactive
Reactive
Report Negative for HIV antibody
Indeterminate
Sample is send for conformation
to NRL, NCDC Delhi
Patient is advised to repeat test after
4 weeks and
Document Name: Laboratory Hand Book for Clinician
Document No.: SMS/MICRO/HIV/LHC/10
Page No.4 | 8
Amendment Number :
Amendment Date:
Version No.- 01
HIV Test Laboratory, Department of Microbiology, SMS Medical College, Jaipur.
Strategy III
To detect HIV infection in asymptomatic individuals
3 Different Test kits required
I Test
Non Reactive
Reactive
Report Negative for HIV antibody
II test different in principle and antigen from I test
______________________________________________________
Non Reactive
Reactive
III test different in principle &
antigen from I and II test
III test different in principle &
antigen from I and II test
__________________________________
Non Reactive
_________________________________
Reactive
Non Reactive
Reactive
Report Negative for
HIV antibody
Report Positive for
HIV antibody
Indeterminate
Sample is send for conformation
to NRL, NCDC Delhi
Patient is advised to repeat test after
4 weeks and
Document Name: Laboratory Hand Book for Clinician
Document No.: SMS/MICRO/HIV/LHC/10
Page No.5 | 8
Amendment Number :
Amendment Date:
Version No.- 01
HIV Test Laboratory, Department of Microbiology, SMS Medical College, Jaipur.
Occupational Exposure and Post Exposure Prophylaxis
An exposure that may place a Health Care Provider (HCP) at risk of blood borne infection is
defined as percutaneous injury (e.g. needle stick or cut with a sharp instrument), contact with the
mucous membranes of the eye or mouth, contact with non-intact skin (particularly when the
exposed skin in chapped, abraded, or afflicted with dermatitis,) or contact with intact skin when the
duration of contact is prolonged (e.g. several minutes or more) with blood or other potentially
infectious body fluids. Body fluids that are potentially infectious include blood, semen, vaginal
secretions, cerebrospinal fluid, synovial, pleural, peritoneal, pericardial and amniotic fluids or other
body fluids contaminated with visible blood.3 Exposure to tears, sweat, urine, faeces, saliva of an
infected person is normally not considered as an exposure unless these secretions contain visible
blood.
Average risk of HIV infection after occupational exposure to HIV infected blood4
Small amount of blood on intact skin
No risk
Needle Stick injury
0.3%
Exposure to eye, nose or mouth
0.09%
Management of Exposure:
Steps to be taken on accidental exposure to blood (or body fluid containing blood) are:
Wash wound immediately with running water and soap.
Inform the hospital management and document occupational accident.
Consult with nearest ART centre/resource for Post-Exposure prophylaxis, evaluation, and
follow-up (as per the national guidelines on PEP)
Whenever possible confidential counseling and testing of source for hepatitis, HIV etc must be
done. A history should be taken as well to ascertain likely risk of the source.
Counseling and collection of blood for testing from the exposed HCP with written informed
consent must be done. PEP should be provided to the exposed HCP until report of source is
available and confirmed negative. PEP should be started with in 1-2 hours of exposure.
Document Name: Laboratory Hand Book for Clinician
Document No.: SMS/MICRO/HIV/LHC/10
Page No.6 | 8
Amendment Number :
Amendment Date:
Version No.- 01
HIV Test Laboratory, Department of Microbiology, SMS Medical College, Jaipur.
Risk of infection and transmission must be evaluated.
PEP should be provided until result of the sources test is available and confirmed negative. If
source is positive or unknown PEP should be given for 4 weeks.
A repeat HIV test of the exposed individual should be performed at 6 weeks, 12 weeks and 6
months post- exposure.
All HCW who report exposure to HIV at work, whether given PEP or not, is to be followed up
for 6 months before a negative antibody test is used to reassure the individual that infection has
not occurred. On all the occasions HCW is provided with a pre test and post test counseling.
The HCW is advised to refuse from donating blood, semen or organ/ tissue and abstain from
sexual intercourse.
What to do after exposure
Donts:
Do not panic!
Do not put pricked finger into mouth.
Do not squeeze blood from wound, this causes trauma and inflammation, increasing risk of
transmission.
Do not use bleach, alcohol, betadine, or iodine, which may cause trauma.
Dos:
Remove gloves, if appropriate.
Wash site thoroughly with running water. Irrigate thoroughly with water or saline if splashes
have gone into the eye or mouth.
Quality Assurance
Quality assurance (QA) refers to planned, step by step activity that lets one know that the testing is
being carried out correctly, results are accurate and mistakes are found and corrected to avoid
adverse outcome. QA is an ongoing set of activities that help to ensure that the test results provided
are accurate and reliable as far as possible for all persons being tested. These activities are in place
during the entire testing process from when a person agrees to be tested until after the test results
are provided.
High quality HIV testing services are maintained at HIV Test Laboratory by:
Document Name: Laboratory Hand Book for Clinician
Document No.: SMS/MICRO/HIV/LHC/10
Page No.7 | 8
Amendment Number :
Amendment Date:
Version No.- 01
HIV Test Laboratory, Department of Microbiology, SMS Medical College, Jaipur.
Adherence to standard operating procedure.
Use of valid test kits.
Correct interpretation of results.
Internal quality control of laboratory.
Regular calibration, monitoring and maintenance of equipments
Proper documentation
References:
1. Manual for HIV testing laboratory: NACO March 2007.
2. Operational guideline for integrated testing and counseling centers NACO-2007
3. Bell DM. Occupation risk of human immune deficiency virus infection in healthcare workers.
An overview. AmJ. Med. 1997; 102. 9-15
4. Gerberdeny J L. Occupational exposure to HIV in healthcare setting.. N Engl J Med 2003; 348826-33.
5. CDC updates public health services guidelines for the management of occupational exposure
HBV, HCV, HIV and recommendation for post exposure
Document Name: Laboratory Hand Book for Clinician
Document No.: SMS/MICRO/HIV/LHC/10
Page No.8 | 8
Amendment Number :
Amendment Date:
Version No.- 01
You might also like
- 1001 Algebra ProblemsDocument292 pages1001 Algebra Problemsasokan8095% (63)
- Laboratory Total Quality Management for Practitioners and Students of Medical Laboratory ScienceFrom EverandLaboratory Total Quality Management for Practitioners and Students of Medical Laboratory ScienceRating: 5 out of 5 stars5/5 (4)
- Ao2019-0001 rHIVdaDocument15 pagesAo2019-0001 rHIVdaDreyden Halo75% (4)
- Safat Book English Spread PDFDocument49 pagesSafat Book English Spread PDFMadan Kumar100% (2)
- Laboratory Test For HIVDocument7 pagesLaboratory Test For HIVBayu Eko SaputroNo ratings yet
- HIV Antibody and HIV Antigen p24 Seminar PaperDocument4 pagesHIV Antibody and HIV Antigen p24 Seminar PaperAna ŠimunovićNo ratings yet
- Lecture SixDocument10 pagesLecture SixJohnNo ratings yet
- LECTURE 8 - Principles of HIV Prevention Control Cont. - Voluntary Counselling TestingDocument8 pagesLECTURE 8 - Principles of HIV Prevention Control Cont. - Voluntary Counselling TestingayubwasongaNo ratings yet
- Lecture VI DIAGNOSIS AND TREATMENT OF HIVDocument6 pagesLecture VI DIAGNOSIS AND TREATMENT OF HIVreginaamondi133No ratings yet
- HIV TestDocument5 pagesHIV TestMahesa NaraNo ratings yet
- Occupational Safety 6Document15 pagesOccupational Safety 6Amal ElnashartyNo ratings yet
- Post-Exposure Prophylaxis (PEP)Document2 pagesPost-Exposure Prophylaxis (PEP)Tati MaryatiNo ratings yet
- Hiv Testing Thesis StatementDocument8 pagesHiv Testing Thesis Statementtmexyhikd100% (2)
- Comparison Between Elisa and Ict Techniques For The Detection of AntiDocument6 pagesComparison Between Elisa and Ict Techniques For The Detection of Antimariam zameerNo ratings yet
- Hiv Tests at Lablink Medical Laboratory Edited 17032017 v2Document24 pagesHiv Tests at Lablink Medical Laboratory Edited 17032017 v2SangieethaNo ratings yet
- PROJECTDocument14 pagesPROJECTsouradipsingha35No ratings yet
- Maternal Blood Test Report: Name of Client: CrmnoDocument3 pagesMaternal Blood Test Report: Name of Client: CrmnoHemanth KumarNo ratings yet
- Makalah Bahasa Inggris Hiv-1Document17 pagesMakalah Bahasa Inggris Hiv-1amelia novita dewiNo ratings yet
- Types of HIV and HIV Testing (2) .PPT.XDocument19 pagesTypes of HIV and HIV Testing (2) .PPT.XronojerutomNo ratings yet
- DIAGNOSING HIV INFECTION AND EXPOSUREDocument24 pagesDIAGNOSING HIV INFECTION AND EXPOSUREBright KumwendaNo ratings yet
- Unit 4 Testing of Hiv/Aids: 4.0 ObjectivesDocument13 pagesUnit 4 Testing of Hiv/Aids: 4.0 ObjectivesandreiNo ratings yet
- Hiv Aids The BasicsDocument3 pagesHiv Aids The BasicsHyrum KamandeNo ratings yet
- Manajemen Hiv.1Document92 pagesManajemen Hiv.1Ariestha Teza AdipratamaNo ratings yet
- HIV AIDS SummaryDocument8 pagesHIV AIDS SummarymugpireNo ratings yet
- Case 06 - Lab Tests and Lab Results HIVDocument4 pagesCase 06 - Lab Tests and Lab Results HIVOmar RamadanNo ratings yet
- 1) Serology - IntroductionDocument5 pages1) Serology - IntroductionAssem AlmoughrabiNo ratings yet
- Test Result FormDocument1 pageTest Result FormJudy Anne Nicole PascuaNo ratings yet
- Who Evd His Emp 15.2 EngDocument9 pagesWho Evd His Emp 15.2 EngSergio Cabrera CalzadillaNo ratings yet
- HIV and Its TreatmentDocument24 pagesHIV and Its Treatmentaathira_kNo ratings yet
- Antibody-Only Tests - Elisas That Detect Antibody To Hiv Are Used As An Initial Test To Screen For Hiv InfectionDocument8 pagesAntibody-Only Tests - Elisas That Detect Antibody To Hiv Are Used As An Initial Test To Screen For Hiv InfectionLorina ApelacioNo ratings yet
- Retest Guidelines As Per WHODocument36 pagesRetest Guidelines As Per WHODevendra NiranjanNo ratings yet
- PSMID 2017 Guidelines For HIV Infected HCWsDocument17 pagesPSMID 2017 Guidelines For HIV Infected HCWsithran khoNo ratings yet
- Is Module 9Document41 pagesIs Module 9gladyskheyagamNo ratings yet
- Infant HIV TestsDocument5 pagesInfant HIV TestsProf Rakesh SharmaNo ratings yet
- HIVandItsTreatment Cbrochure enDocument15 pagesHIVandItsTreatment Cbrochure enCarlos Navarrete-PatinoNo ratings yet
- Oral BiologyDocument4 pagesOral BiologyDebby ApriliaNo ratings yet
- Hiv Viral LoadDocument6 pagesHiv Viral LoadPhiliplukaNo ratings yet
- Assessment of Hiv Aids Among Intending DonorsDocument48 pagesAssessment of Hiv Aids Among Intending DonorsmubarakNo ratings yet
- Bloodborne and Airborne Pathogens Exposure Protocol: Effective August 15, 2017Document4 pagesBloodborne and Airborne Pathogens Exposure Protocol: Effective August 15, 2017Dwight AvelinoNo ratings yet
- Rapid Hiv Tests:: Guidelines For Use in Hiv Testing and Counselling Services in Resource-Constrained SettingsDocument50 pagesRapid Hiv Tests:: Guidelines For Use in Hiv Testing and Counselling Services in Resource-Constrained SettingsMuhammad Hafidzul HairulNo ratings yet
- Ao2019 0001Document15 pagesAo2019 0001Don Christian DemecilloNo ratings yet
- INTEGRATED COUNSELLING & TESTING CENTRESDocument19 pagesINTEGRATED COUNSELLING & TESTING CENTRESLalit Kr YadavNo ratings yet
- EXP-10-HIV ConieDocument4 pagesEXP-10-HIV ConieNimfa GumiranNo ratings yet
- Advances and Trends in Sepsis Diagnostics PDFDocument12 pagesAdvances and Trends in Sepsis Diagnostics PDFGRAÇAS PERFUMARIANo ratings yet
- Immunochromatography Pada IDU (Infecting Drug User) : Uji Sensitivitas Dan Spesifitas Anti - HIV MetodeDocument9 pagesImmunochromatography Pada IDU (Infecting Drug User) : Uji Sensitivitas Dan Spesifitas Anti - HIV MetodeDewanto WicaksonoNo ratings yet
- ZOOL 143 Topic 7 Detection of HIV Infection 1Document10 pagesZOOL 143 Topic 7 Detection of HIV Infection 1nattydreadfathelahNo ratings yet
- Ramon Magsaysay Memorial Medical Center Inc.: College of NursingDocument3 pagesRamon Magsaysay Memorial Medical Center Inc.: College of NursingJona Joyce JunsayNo ratings yet
- L5 - Animal Cell BiotechDocument48 pagesL5 - Animal Cell Biotechtrieupg.22bi13431No ratings yet
- Management of Human Immunodeficiency Virus Infection (HIV)Document1 pageManagement of Human Immunodeficiency Virus Infection (HIV)zenagit123456No ratings yet
- Services Provided at Art CentersDocument4 pagesServices Provided at Art Centersprabha krishnanNo ratings yet
- Serological Testing of HIVDocument4 pagesSerological Testing of HIVOSAMA BAKHITNo ratings yet
- Hiv Seminar 2019Document49 pagesHiv Seminar 2019clarice_condeno100% (1)
- 1 - PPT Dr. Agnes R. Indrati KONAS 2022Document33 pages1 - PPT Dr. Agnes R. Indrati KONAS 2022Mustakim DuharingNo ratings yet
- Bio Inv Proj 2Document14 pagesBio Inv Proj 2Rishit KumarNo ratings yet
- International Journal of Gynecology and ObstetricsDocument5 pagesInternational Journal of Gynecology and ObstetricsWilliams Alejandro Choroco VillegasNo ratings yet
- Post Exposure Prophylaxis: Hepatitis B, Hepatitis C and HivDocument10 pagesPost Exposure Prophylaxis: Hepatitis B, Hepatitis C and HivQaiser ZamanNo ratings yet
- BHIVA/EAGA (UK) Position Statement On The Use of Antiretroviral Therapy To Reduce HIV Transmission Updated Sept 2014Document6 pagesBHIVA/EAGA (UK) Position Statement On The Use of Antiretroviral Therapy To Reduce HIV Transmission Updated Sept 2014HIV Justice NetworkNo ratings yet
- Bulletin of The World Health OrganizationDocument11 pagesBulletin of The World Health OrganizationJohn LewandowskiNo ratings yet
- JPAM Vol 14 Issue1 P 609-614Document6 pagesJPAM Vol 14 Issue1 P 609-614Tira Alfiani LaariyaNo ratings yet
- NHA Phlebotomy Exam 2022-2023: Study Guide with 400 Practice Questions and Answers for National Healthcareer Association Certified Phlebotomy Technician ExaminationFrom EverandNHA Phlebotomy Exam 2022-2023: Study Guide with 400 Practice Questions and Answers for National Healthcareer Association Certified Phlebotomy Technician ExaminationNo ratings yet
- Interview Questions And Answers For Band Five Biomedical Scientists: Continuing Professional Development in Pathology For Medical Laboratory ProfessionalsFrom EverandInterview Questions And Answers For Band Five Biomedical Scientists: Continuing Professional Development in Pathology For Medical Laboratory ProfessionalsNo ratings yet
- Pathology Laboratory Support Staff (Band Two to Four) Interview Questions and Answers For Biomedical Science Graduates without HCPC Registration: Continuing Professional Development in Pathology For Medical Laboratory ProfessionalsFrom EverandPathology Laboratory Support Staff (Band Two to Four) Interview Questions and Answers For Biomedical Science Graduates without HCPC Registration: Continuing Professional Development in Pathology For Medical Laboratory ProfessionalsNo ratings yet
- Submission To Procurement Review Committee: Building / Construction / Roads and Bridges Only (Otherwise Delete)Document3 pagesSubmission To Procurement Review Committee: Building / Construction / Roads and Bridges Only (Otherwise Delete)dileep2000100% (1)
- Employee Poster (Sample) Do You Know The New Emergency Codes?Document1 pageEmployee Poster (Sample) Do You Know The New Emergency Codes?dileep2000No ratings yet
- QIAGEN Autho & Price List of KitsDocument6 pagesQIAGEN Autho & Price List of Kitsdileep2000No ratings yet
- Central Civil Services RulesDocument37 pagesCentral Civil Services Rulesdileep2000No ratings yet
- Subtraction Grade 1 Single Digit Fill in The Blanks Exercises Worksheet Fruit ThemeDocument2 pagesSubtraction Grade 1 Single Digit Fill in The Blanks Exercises Worksheet Fruit Themedileep2000No ratings yet
- Hsbtc-Naco Guidelines For Renewal-Approval of BB License - 06092012Document2 pagesHsbtc-Naco Guidelines For Renewal-Approval of BB License - 06092012dileep2000No ratings yet
- Antibiotic List JMCDocument3 pagesAntibiotic List JMCdileep2000No ratings yet
- Puc QP May 2016Document1 pagePuc QP May 2016dileep2000No ratings yet
- National Guidelines Anaesthesiologists FeesDocument4 pagesNational Guidelines Anaesthesiologists Feesdileep2000No ratings yet
- Antibiotic Disc For PracticalDocument4 pagesAntibiotic Disc For Practicaldileep2000No ratings yet
- Laboratory - Handbook - For - Clinicians Rearding HIV Testing SMS Medical College, JaipurDocument9 pagesLaboratory - Handbook - For - Clinicians Rearding HIV Testing SMS Medical College, Jaipurdileep2000No ratings yet
- Noise PollutionDocument5 pagesNoise Pollutiondileep2000No ratings yet
- EXPERIMENTAL-RESEARCH-BIOPLASTIC-12-ABM-PDF (1)Document11 pagesEXPERIMENTAL-RESEARCH-BIOPLASTIC-12-ABM-PDF (1)hannahamodia74No ratings yet
- Prelim ReviewerDocument11 pagesPrelim ReviewerRuth Abegail de VeraNo ratings yet
- Make A Home Made Power PlantDocument117 pagesMake A Home Made Power PlantMoreMoseySpeed100% (3)
- Auburn Trader - July 20, 2011Document12 pagesAuburn Trader - July 20, 2011GCMediaNo ratings yet
- Doing Stuff With Web ThingsDocument102 pagesDoing Stuff With Web ThingsRamon Felipe Castaño SalgadoNo ratings yet
- Caravan Price List: New For 2018 New For 2018 New For 2018 New For 2018Document2 pagesCaravan Price List: New For 2018 New For 2018 New For 2018 New For 2018Danut TudoracheNo ratings yet
- KA 2020 2 Redox-PotentiometryDocument55 pagesKA 2020 2 Redox-PotentiometryNicolaus DedeoNo ratings yet
- CholeraDocument24 pagesCholeraLavanya Sivakumar100% (1)
- Phe Microproject ReportDocument20 pagesPhe Microproject ReportAbrar Khan100% (2)
- Dyna TecDocument226 pagesDyna Tecluke7670No ratings yet
- Direct Route To Phenol From Benzene PDFDocument316 pagesDirect Route To Phenol From Benzene PDFM Arslan AshrafNo ratings yet
- WaltonDocument22 pagesWaltontahmidur.rahman01No ratings yet
- Edexcel GCSE Physics Mind MapsDocument38 pagesEdexcel GCSE Physics Mind MapsDanmin YuNo ratings yet
- TST2601 - Minor Test 1 - Memo - 2022Document8 pagesTST2601 - Minor Test 1 - Memo - 2022Johan PienaarNo ratings yet
- OP Valeo Wiper Blades 1005Document4 pagesOP Valeo Wiper Blades 1005Sinead1990No ratings yet
- Young Robin Hood by Fenn, George Manville, 1831-1909Document44 pagesYoung Robin Hood by Fenn, George Manville, 1831-1909Gutenberg.orgNo ratings yet
- Gcse Art - Esa Guide For Grade 8 or 9Document6 pagesGcse Art - Esa Guide For Grade 8 or 9Selene KNo ratings yet
- Project Closure: Taking A TollDocument4 pagesProject Closure: Taking A TollDinesh RaghavendraNo ratings yet
- Porthole RecipeDocument20 pagesPorthole RecipeBill Murray100% (1)
- Techno-Economic Analysis Factsheet - ANLDocument2 pagesTechno-Economic Analysis Factsheet - ANLJAI SAHITHNo ratings yet
- The Best Managers Balance Analytical and Emotional IntelligenceDocument4 pagesThe Best Managers Balance Analytical and Emotional IntelligenceCristinaNo ratings yet
- TLE 1-Unit 3-4 Teaching Strategies and Assessment Methods in TLEDocument41 pagesTLE 1-Unit 3-4 Teaching Strategies and Assessment Methods in TLEMaisy Hope Vargas100% (3)
- Wilber Motor:: Wheel Chain Track Gear PulleyDocument6 pagesWilber Motor:: Wheel Chain Track Gear Pulleypramo_dassNo ratings yet
- 115 Syphilis-V3.0-en-EUDocument4 pages115 Syphilis-V3.0-en-EUPierina DonayreNo ratings yet
- Magnetic DipoleDocument4 pagesMagnetic DipoletechzonesNo ratings yet
- Project Report On RAYMONDDocument42 pagesProject Report On RAYMONDsantosh74% (38)
- XGB+Analog+English+Manual+V1 9+20140528Document617 pagesXGB+Analog+English+Manual+V1 9+20140528RodrigoAdur1No ratings yet
- Low Salinity Water and Polymer Flooding in Sandstone reservoirs-CMGDocument20 pagesLow Salinity Water and Polymer Flooding in Sandstone reservoirs-CMGNguyên LêNo ratings yet