1 s2.0 S0264410X1501470X Main
1 s2.0 S0264410X1501470X Main
Uploaded by
Sheron Jude SeneviratneCopyright:
Available Formats
1 s2.0 S0264410X1501470X Main
1 s2.0 S0264410X1501470X Main
Uploaded by
Sheron Jude SeneviratneOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
1 s2.0 S0264410X1501470X Main
1 s2.0 S0264410X1501470X Main
Uploaded by
Sheron Jude SeneviratneCopyright:
Available Formats
Vaccine 33 (2015) 65296536
Contents lists available at ScienceDirect
Vaccine
journal homepage: www.elsevier.com/locate/vaccine
Review
The current situation of meningococcal disease in Latin America and
updated Global Meningococcal Initiative (GMI) recommendations
Marco Aurlio P. Sfadi a, , Miguel ORyan b , Maria Teresa Valenzuela Bravo c ,
Maria Cristina C. Brandileone d , Maria Ceclia O. Gorla d , Ana Paula S. de Lemos d ,
Gabriela Moreno e , Julio A. Vazquez f , Eduardo L. Lpez g , Muhamed-Kheir Taha h ,
Ray Borrow i , On behalf of the Global Meningococcal Initiative
a
FCM da Santa Casa de So Paulo, Alameda dos Indigenas, 228, 04059 060 So Paulo, Brazil
Faculty of Medicine, University of Chile, Independencia 1027, Santiago, Chile
c
Department of Public Health and Epidemiology, Universidad de los Andes, Santiago, Chile
d
Instituto Adolfo Lutz, Centro de Bacteriologia, Av. Dr. Arnaldo 355, So Paulo, SP 01246-902, Brazil
e
Jefa de la Divisin de Planicacin Sanitaria, Ministerio de Salud, Santiago, Chile
f
Reference Laboratory for Neisserias, National Center for Microbiology, Institute of Health Carlos III, Madrid, Spain
g
Sociedad Argentina de Infectologa Peditrica and Departamento de Medicina del Hospital de Ni
nos Dr Ricardo Gutirrez, Buenos Aires, Argentina
h
Institut Pasteur, National Reference Center for Meningococci, Unite Invasive Bacterial Infections, 28 rue du Dr Roux, Paris Cedex 15 75724, France
i
Vaccine Evaluation Unit, Public Health England, Clinical Sciences Building, Manchester Royal Inrmary, Manchester M13 9WZ, UK
b
a r t i c l e
i n f o
Article history:
Received 6 May 2015
Received in revised form 8 September 2015
Accepted 9 October 2015
Available online 25 October 2015
Keywords:
Epidemiology
Global Meningococcal Initiative
Meningococcal disease
Serogroup W
Surveillance
Vaccination
a b s t r a c t
The Global Meningococcal Initiative (GMI) was established in 2009 and comprises an international team of
scientists, clinicians, and public health ofcials with expertise in meningococcal disease (MD). Its primary
goal is to promote global prevention of MD through education, research, international cooperation, and
developing recommendations that include decreasing the burden of severe disease. The group held its rst
roundtable meeting with experts from Latin American countries in 2011, and subsequently proposed several recommendations to reduce the regional burden of MD. A second roundtable meeting was convened
with Latin American representatives in June 2013 to reassess MD epidemiology, vaccination strategies,
and unmet needs in the region, as well as to update the earlier recommendations. Special emphasis was
placed on the emergence and spread of serogroup W disease in Argentina and Chile, and the control measures put in place in Chile were a particular focus of discussions. The impact of routine meningococcal
vaccination programs, notably in Brazil, was also evaluated. There have been considerable improvements
in MD surveillance systems and diagnostic techniques in some countries (e.g., Brazil and Chile), but the
lack of adequate infrastructure, trained personnel, and equipment/reagents remains a major barrier to
progress in resource-poor countries. The Pan American Health Organizations Revolving Fund is likely to
play an important role in improving access to meningococcal vaccines in Latin America. Additional innovative approaches are needed to redress the imbalance in expertise and resources between countries,
and thereby improve the control of MD. In Latin America, the GMI recommends establishment of a
detailed and comprehensive national/regional surveillance system, standardization of laboratory procedures, adoption of a uniform MD case denition, maintaining laboratory-based surveillance, replacement
of polysaccharide vaccines with conjugate formulations (wherever possible), monitoring and evaluating implemented vaccination strategies, conducting cost-effectiveness studies, and developing specic
recommendations for vaccination of high-risk groups.
2015 Elsevier Ltd. All rights reserved.
Abbreviations: ANLIS, Administracin Nacional de Laboratorios e Institutos de Salud (Argentina); CFR, case fatality rate; GMI, Global Meningococcal Initiative; MCC,
meningococcal C conjugate; MD, meningococcal disease; MoH, Ministry of Health; NIP, National Immunization Program; PAHO, Pan American Health Organization; PCR,
polymerase chain reaction; RT-PCR, real-time polymerase chain reaction; SIREVA, Sistema Regional de Vacunas; SIREVA II, Sistema de Redes de Vigilancia de Agentes
Bacterianos Causantes de Meningitis y Neumonas.
Corresponding author at: FCM da Santa Casa de So Paulo, Alameda dos Indigenas, 228, 04059 060 So Paulo, Brazil. Tel.: +55 11 999842584; fax: +55 11 55947579.
E-mail addresses: masafadi@uol.com.br (M.A.P. Sfadi), moryan@med.uchile.cl (M. ORyan), mtvalenzuela@uandes.cl (M.T. Valenzuela Bravo), brandi@ial.sp.gov.br
(M.C.C. Brandileone), mcgorla@ial.sp.gov.br (M.C.O. Gorla), apaula@ial.sp.gov.br (A.P.S. de Lemos), gabrielabmorenom@gmail.com (G. Moreno), jvazquez@isciii.es
(J.A. Vazquez), eduardoluislopez@bertel.com.ar (E.L. Lpez), muhamed-kheir.taha@pasteur.fr (M.-K. Taha), Ray.Borrow@phe.gov.uk (R. Borrow).
http://dx.doi.org/10.1016/j.vaccine.2015.10.055
0264-410X/ 2015 Elsevier Ltd. All rights reserved.
6530
M.A.P. Sfadi et al. / Vaccine 33 (2015) 65296536
1. Introduction
Neisseria meningitidis remains a major cause of invasive bacterial disease worldwide and is associated with substantial morbidity
and overall case fatality rates (CFRs) of around 10% (overall CFRs
as high as 20% have been reported in some countries [14]). Disease caused by serogroup W alone has been associated with CFRs of
>30% [5]. In Latin America, incidence rates and serogroup distribution of meningococcal disease (MD) are highly variable (from <0.1
to almost 2 cases per 100,000 inhabitants), with the highest burden of disease reported in Brazil and the Southern Cone countries
(Argentina, Chile, and Uruguay); very limited data are available
from the Andean region, Mexico, and Central America [6].
The Global Meningococcal Initiative (GMI), established in 2009,
is a multidisciplinary group with expertise in areas such as public health, epidemiology/seroepidemiology, pediatrics, infectious
disease, microbiology, immunology, and vaccinology. It aims to
help prevent MD worldwide through education, research, international cooperation, and to develop recommendations that include
decreasing the burden of severe disease [7] through promotion of
prevention strategies, early diagnosis and treatment, and disease
awareness.
At the rst GMI regional Latin American roundtable meeting
in 2011, the epidemiology of MD in the region was reviewed and
several recommendations were proposed to reduce the burden
of MD (Table 1) [6]. It was concluded that MD burden in Latin
America is largely underestimated, and it was stressed that control
efforts should focus on educating physicians and regulators on the
importance of the disease, its diagnosis, improving meningococcal
surveillance in the region, and the need for uniform, good-quality
data. To improve surveillance in the region and facilitate data
comparisons, a uniform case denition was proposed that supplemented Pan American Health Organization (PAHO) criteria with
conrmation by polymerase chain reaction (PCR; where available)
[6]. It was felt that end-point PCR and real-time PCR (RT-PCR) could
make a difference in the region in terms of recognition of the disease (especially given the increasing early use of antibiotics, which
leads to culture-negative results) [6]. While countries should use
Table 1
Global Meningococcal Initiative recommendations for reducing the global burden
of meningococcal disease in Latin America (as described in Safadi et al. [6]).
1.
2.
3.
4.
5.
6.
7.
8.
The supplementation of culture with standardized nucleic acid
amplication techniques for disease conrmation and
implementation of molecular genotype characterization
techniques as a routine in national and regional reference
laboratories
The introduction of quality controls so that data from different
laboratories can be harmonized
Consistent and universal use of standardized diagnostic protocols,
such as those set out by SIREVA II or PAHO
The forging of partnerships between resource-rich and
resource-constrained regions to improve laboratory capacity (and
the quality and quantity of the epidemiologic data available)
The implementation of active population- and laboratory-based
surveillance for invasive MD at selected sites to assist in early
outbreak detection and estimation of age-specic incidence rates
and serogroup distribution
Replacement of polysaccharide vaccines with conjugate
formulationswherever possible
Proposed vaccination policies against MD should be
country-specic and based on local disease dynamics and health
priorities
Novel nancing arrangements should be considered, such as:
Technology transfer agreements
The PAHO Revolving Fund
Advanced market commitments
MD, meningococcal disease; PAHO, Pan American Health Organization; SIREVA II,
Sistema de Redes de Vigilancia de Agentes Bacterianos Causantes de Meningitis y
Neumonas.
whichever PCR method is available to them, it is well accepted that
RT-PCR is more sensitive and precise than end-point PCR, and is
less time consuming [8]. RT-PCR uses a uorescent dye system that
provides a higher sensitivity and specicity than end-point PCR,
which uses ethidium bromide and UV light to visualize bands in
the agarose gel medium.
In June 2013, a second GMI Latin American meeting was held
to provide an update on the epidemiology of MD, with an emphasis on the recent emergence of serogroup W disease in Argentina
and Chile. The experience with recent meningococcal vaccination
programs implemented in the region (i.e., routine meningococcal C
conjugate [MCC] vaccination for infants and toddlers in Brazil and
reactive quadrivalent [serogroups A, C, W, and Y] meningococcal
conjugate vaccination in Chile) was discussed. In addition, recommendations for the control and prevention of MD in Latin America
were updated. This article summarizes the discussions that took
place at the meeting.
2. Epidemiology of meningococcal disease in Latin America
Informed decisions about appropriate vaccination strategies to
control MD depend upon a thorough understanding of the epidemiology of the disease in the various countries. The reported annual
incidence of MD in Latin America varies widely, ranging from <0.1
cases per 100,000 inhabitants in countries such as Bolivia, Cuba,
Mexico, Paraguay, and Peru to nearly two cases per 100,000 inhabitants in Brazil [6,7,9]. The reporting of MD is mandatory in Latin
America, but surveillance systems and reporting are not standardized across countries [9,10]. In addition, there is limited access to
hospital care in some countries, as well as differences in the diagnostic methods/conditions and MD case denitions [6,10]. These
differences may contribute to the variability in disease incidence;
caution should therefore be exercised when interpreting epidemiologic data from the region.
Despite MD being a mandatory notiable disease in all Latin
American countries, reports are likely to represent underestimates
of the true disease burden [7]. In Latin America, laboratory-based
diagnosis of suspected cases of MD is based principally on culture methods, and inadequate microbiologic services and previous
antibiotic use (risk factors for culture negativity) may contribute
to disease underreporting [11]. Restrictive case denitions of MD
in some countries, such as Mexico, may also contribute to low
reporting rates [6]. The highest rates of MD in Latin America are
reported for Argentina, Brazil, Chile, and Uruguay, but this is probably because these countries have more advanced surveillance
systems and laboratory services than some others [6]. Indeed, the
introduction of multiplex RT-PCR testing for N. meningitidis in hospitals in So Paulo, Brazil, increased the diagnostic yield for MD by
85% over culture-based methods [11]. In addition to this, in 2013
and 2014 in Chile, after the implementation of PCR by the Instituto
de Salud Pblica, approximately 15% of the cases reported were
identied by this methodology [12].
A Latin American, laboratory-based surveillance network (Sistema Regional de Vacunas [SIREVA]) was introduced in 1993 by the
PAHO, to collect laboratory and epidemiologic data on specic bacterial diseases [12]. SIREVA II (Sistema de Redes de Vigilancia de
Agentes Bacterianos Causantes de Meningitis y Neumonas) currently performs a systematic analysis of N. meningitidis isolates
recovered by the epidemiologic survey network from countries in
Latin America and the Caribbean, and 20 countries/areas in Latin
America are participating in the surveillance program (Table 2)
[6,12,13]. Strengthening surveillance systems for MD and establishing a closer link between epidemiology, laboratory testing, and
clinical aspects of the disease are challenges and key goals of the
Latin America and Caribbean network.
M.A.P. Sfadi et al. / Vaccine 33 (2015) 65296536
Table 2
Number of Neisseria meningitidis isolates, from invasive MD cases, reported by
SIREVA II during 20062012 [13].
Country
Number
Country
Number
Argentina
Bolivia
Brazil
CAREC
Chile
Colombia
Costa Rica
Cuba
Ecuador
El Salvador
935
3
4416
8
507
189
41
41
29
29
Guatemala
Honduras
Mexico
Nicaragua
Panama
Paraguay
Peru
Dominican Republic
Uruguay
Venezuela
Total
0
5
66
6
73
61
4
57
209
167
6846
CAREC, the Caribbean Epidemiology Center/Pan American Health Organization (Barbados, and Trinidad and Tobago); SIREVA II, Sistema de Redes de Vigilancia de
Agentes Bacterianos Causantes de Meningitis y Neumonas.
The GMI has proposed a number of recommendations to help
improve and standardize reporting of MD in Latin America. These
recommendations include a clear denition of a suspected case,
the use of molecular diagnostic techniques (e.g., PCR/RT-PCR) in
routine surveillance, expanding the use of culture methods, establishing well-equipped sentinel and reference laboratories with
highly trained staff, and adopting a single case denition for use
in all Latin American countries (Table 3) [6,14]. This denition
includes molecular diagnostic techniques (where available and for
countries that have resolved the issue of prompt sample collection and testing, which is the rst step toward improving diagnosis
capacity). RT-PCR has high sensitivity and specicity for N. meningitidis versus culture methods, and even when bacteria are nonviable
after antibiotic treatment, PCR is able to detect N. meningitidis
deoxyribonucleic acid [11]. The GMI recommends an integrated
surveillance approach of laboratory and clinical notications, as
conducted in Chile, where the Department of Epidemiology of the
Ministry of Health manages all of the countrys MD information and
the Public Health Institute coordinates the activities of a network
of centers trained in RT-PCR. Nevertheless, the GMI recognizes that
some countries have resource and nancial constraints, which prevent them from taking up all recommendations, and it therefore
encourages alliances to be formed with other supportive organizations [6].
As elsewhere, the highest incidence of sporadic MD in Latin
America occurs in infants and young children [7,9], but data on
Table 3
Case denition for meningococcal disease (MD) proposed by the Global Meningococcal Initiative for use in Latin America (PAHO case denition plus conrmatory
diagnosis by PCR) [6], copyright 2013, Informa Healthcare. Reproduced with permission of Informa Healthcare.
Suspected MD (clinical case denition) [14]
An illness with sudden onset of fever (>38.5 C rectal or >38.0 C axillary)
and one or more of the following:
Neck stiffness
Altered consciousness
Other meningeal sign or petechial or purpuric rash
In patients <1 year old, MD should be suspected when fever is
accompanied by bulging fontanel
Conrmed (suspected MD plus at least one of the following laboratory
criteria):
Detection of bacterial antigen(s) in CSF
Positive bacterial culture in normally sterile body site (such as CSF
and/or blood and/or skin lesion)
Detection of bacterial DNA by PCR or RT-PCR in normally sterile body
site (such as CSF and/or blood and/or skin lesion)
CSF, cerebrospinal uid; DNA, deoxyribonucleic acid; PAHO, Pan American Health
Organization; PCR, polymerase chain reaction; RT-PCR, real-time PCR.
6531
outbreaks have shown an increased number of cases in adolescents
and young adults [15,16]. This peak among adolescents and young
adults during outbreaks may be related to behavioral risk factors
(e.g., kissing, smoking, or frequenting nightclubs) [17,18] and the
introduction of new clones [19].
Monitoring phenotypic and genotypic characteristics of circulating N. meningitidis strains is of fundamental importance in
understanding MD in each country. Six serogroups (A, B, C, W, X,
and Y) cause nearly all cases of MD globally [20]. Most cases of MD in
Latin America are sporadic and caused by serogroups B and C, with
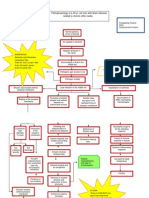
emergence of serogroup W in Southern Cone countries, particularly Argentina and Chile (Fig. 1) [7,13,21]. In contrast, serogroup
A has virtually disappeared from Latin America [6,13]. Molecular
typing is also of importance given that control and management of
MD are predicated upon understanding current epidemiology (see
Supplementary Material).
Information about the carriage of N. meningitidis is essential in
understanding the transmission dynamics of meningococcal infection [22], and for assessing the extent and potential that exists
for vaccination strategies to induce herd protection [10]. Although
there are limited published data on carriage of N. meningitidis
in Latin America [10,23], four carriage studies (Brazil, Argentina,
Colombia, and Paraguay) are ongoing or have been completed
recently. A study among adolescents (n = 1208, age 1119 years) in
Campinas, Brazil, showed an overall carriage rate of 9.9%, with dominance of serogroup C (1.3%) and the highest prevalence (12%) in
older adolescents (age 1719 years). In addition, a study of healthy
Chilean university students, using only culture, found an overall
carriage rate of 4% [25].
3. Importance of serogroup W
3.1. The spread and rise of serogroup W
Outbreaks due to serogroup W (formerly W-135) were rst
reported in pilgrims attending the Hajj in Mecca, Saudi Arabia.
Following this, W outbreaks (many travel-related) were detected
in countries and regions across the globe (including the United
States, Turkey, Europe, and sub-Saharan Africa; see Supplementary
Material).
3.2. The emergence of serogroup W in Latin America
Currently in Latin America, serogroups B and C are dominant, but
increases in the proportion of MD cases attributable to serogroup
W, and W outbreaks, have been reported in several countries
[12,26]. Since 1990, cases of W:2a:P1.5,2:ST-11 complex MD were
detected in the region [27]. One recent study analyzed laboratory data for 4735 isolates collected by the national reference
laboratories in 19 Latin American countries and the Caribbean
Epidemiology Center from 2006 to 2010 [12]. In Brazil and the
Andean region, a small percent of isolates were serogroup W (5.2%
and 1.2%, respectively), while none were isolated in Venezuela.
Similarly, in Mexico, Central America, and the Caribbean region,
a very small percent (0.4%) of isolates were serogroup W, while
a considerably larger percent (19.6%) of isolates in the Southern Cone region belonged to serogroup W (this percent will be
higher currently, given the marked increase in W in the region).
The largest increase in prevalence of serogroup W in the region
was observed in Argentina, where in 2006 it represented 6.3%
of the isolates, increasing to 52% by 2012. Moreover, in 2006,
there were only four invasive serogroup W isolates detected in
Argentina, which dramatically increased to 96 isolates in 2012
[28,29]. SIREVA II data also revealed that specic age groups were
affected disproportionately by serogroup W and changed over
6532
M.A.P. Sfadi et al. / Vaccine 33 (2015) 65296536
Fig. 1. Meningococcal serogroup distribution in selected countries in Latin America (20062012), for all age groups [13,21].
time. In 2006, serogroup W affected older individuals primarily, but from 2008 onward, younger individuals were impacted
more oftena situation similar to that observed in the sub-Saharan
region [30]. Other research shows that during the past 6 years
in Brazil, MD caused by serogroup W has mainly been connected to local strains from the ST-11 clonal complex, as has been
reported in other countries [31]. Whole genomic sequencing analysis recently demonstrated that the MenW:cc11 strain, which is
currently endemic in Brazil and Argentina is distinct from the Hajj
outbreak strain [32].
3.3. The Chilean experience
The Chilean experience provides a unique opportunity to learn
more about serogroup W disease due to the in-depth data that have
been amassed to date. Indeed, we now understand that serogroup
W is a hypervirulent strain often belonging to sequence type 11
clonal complex, and has been associated with very high CFR. We
also have enhanced knowledge regarding its dynamics, and how it
acts on carriers at different ages, as cases are rare in adolescents
compared with infants, young children, and the elderly. The events
can also be used to evaluate the effectiveness of surveillance and
the implementation of a reactive quadrivalent (serogroups A, C, W,
and Y) meningococcal conjugate vaccination against serogroup W
disease.
Serogroup W emerged in Argentina and Brazil around 2001, and
the number of W cases has since increased (three invasive isolates
were recorded in 2001 rising to 96 in 2012 in Argentina, and 17
invasive isolates were detected in Brazil in 2001 rising to 28 in
2012) [13,28,29,33]. Likewise, cases due to serogroup W belonging
to the clonal complex ST-11 were identied in Chile in 2001, and
in 2010 and 2011 most of the serogroup W strains that were characterized were shown to belong to clonal complex ST-11 (6/6 in
2010 and 19/23 in 2011) [34,35]. In 2010, 9% of the isolates in Chile
were serogroup W [12]. By 2012, this serogroup accounted for 58%
of all cases, surpassing serogroup B (37%) for the rst time [26].
Meanwhile, the overall incidence rate of invasive MD was 0.7 per
100,000 population, and almost 50% of cases occurred in children <5
years old [26]. As expected, the incidence rate was highest (19 per
100,000) in very young infants (34 months old). A peak was also
observed in persons >60 years old, whereas the number of cases in
adolescents was very low [26]. In 2013, more serogroup W cases
were identied versus 2012 [36]. In 2012, the CFR for MD caused
by serogroup W was high (31.7%), probably due to the high rates
of meningococcemia observed [5]. A high CFR was also observed in
2013. Most cases in 2012 and 2013 were reported in the Santiago
Metropolitan Region [37], the likely reason for this being its higher
population density versus other regions of the country. A study is
ongoing to identify factors that increase the risk for serogroup W
infection.
M.A.P. Sfadi et al. / Vaccine 33 (2015) 65296536
3.4. Control measures to manage serogroup W outbreaks
In response to the increase in CFR associated with serogroup W
in Chile, the Ministry of Health (MoH) implemented a serogroup
W action plan [26]. This plan required the MoH and public health
centers to work together to improve surveillance, and included
integrated epidemiologic surveillance; antimicrobial chemoprophylaxis of close contacts; a communicative media plan; an
immunization plan; partnerships with the Ministry of Education;
proposals for epidemiologic studies; and the involvement of the
Immunization Advisory Committee and the scientic societies.
In Chile, it is now mandatory to report all suspected clinical cases
of MD. Patients and results are referred locally, and at the same
time the information is sent to the health ministry and regional
ministerial center.
Previously, routine vaccination was not used for prevention of
meningococcal disease, and local vaccination was conducted during outbreaks due to N. meningitidis serogroup C in some places
to prevent further infection. All close contacts of infected patients
were treated with chemoprophylaxis within 24 h of notication of
index cases. In response to the increased number of serogroup W
cases and the associated CFR observed, strategic vaccination of children aged 9 months to 5 years was initiated in October 2012 using
the tetravalent conjugate vaccine. This approach has been successful in this age group, as no further cases due to serogroup W have
been identied in this vaccinated cohort.
Several articles on the Chilean experience have been, or are in
the process of being, published [26,35,38]. In addition, the Web
pages of the Public Health Institute and the Department of Epidemiology of the MoH include weekly updates so that the effectiveness
of the Chilean strategies can be evaluated [37]. Currently, there is
a need to strengthen integrated surveillance (epidemiologic, laboratory, and clinical) to assess the effectiveness of vaccination in
the short term and to evaluate the epidemiologic behavior of the
disease and the risk groups periodically. The impact of the interventions used in Chile is of great importance globally, as lessons
learned here could be applied in other countries. It is also of interest to determine if the interventions will affect other age groups,
although this has not been observed to date. New potential strategies, including immunization of young infants and a catch-up
campaign targeting adolescents and young adults, are being discussed to optimize the impact of the vaccination program in Chile.
In summary, much has been learned from the Chilean experience, such as the importance of an integrated surveillance system,
a rapid response, and transparent dissemination of data to the public. Chile has a legal and organizational structure in place to control
and manage MD, as well as technical resources. As serogroup W disease is appearing/rising in other countries, what has been learned
in Chile will be of great importance not only regionally, but also
globally.
4. Impact of routine meningococcal vaccination programs
in Latin America
4.1. Brazil: experience of routine immunization against MD
In late 2010, Brazil became the rst Latin American country to
introduce MCC vaccination into the routine National Immunization Program (NIP) [39,40]. The decision by the Brazilian MoH was
based on the epidemiologic situation and the serogroup C outbreaks reported across the country. During the period immediately
before the introduction of the MCC vaccination program, annual
incidence rates of MD were stable, with approximately 1.6 cases per
100,000 inhabitants, varying in 2010 from <1 case per 100,000 in
the northern region to 3.5 cases per 100,000 in So Paulothe state
6533
with the most well-established meningitis surveillance system
[40]. The highest age-specic incidence of MD occurred in children <5 years old [12]. However, during outbreaks and epidemics,
increased numbers of cases were often observed in adolescents and
young adults [10]. The overall CFR was consistently high in the past
decade (around 20%). From 2002 onward, a signicant increase in
the proportion of cases attributed to serogroup C (ST-103 complex)
was observed [10], and by 2010, serogroup C was responsible for
approximately 80% of identied MD cases [12,40].
The MCC vaccine was introduced into the routine immunization
schedule of infants (two doses, at 3 and 5 months, and a booster
dose at 12 months) [10]. Toddlers aged 1223 months received
one vaccine dose, with no catch-up campaign for older age groups
[9,10]. Coverage for the two primary doses was 85% in late 2011,
rising to 9095% in 2012 [41]. The introduction of the MCC vaccine
into the NIP provided an immediate reduction in incidence rates of
MD in children aged <2 years, the age group targeted for vaccination
(Table 4) [41]. However, no early impact was observed in unvaccinated age groups (Table 4), probably reecting the lack of a catch-up
program targeting adolescents and young adultsthe age groups
primarily responsible for carriage and transmission [22]. Interestingly, Brazil is the rst country in the world to provide experience
with MCC vaccines against non-ST-11 N. meningitidis [42].
5. Achievements and unmet needs in Latin America in
recent years
5.1. Achievements
5.1.1. Surveillance of meningococcal disease
As discussed, although notication of MD is compulsory in
Latin America, surveillance is inconsistent. Recent improvements
have included implementation of more reliable population-based
surveillance systems and inclusion of accurate detection techniques (e.g., standardized culture techniques and PCR applied to
blood, cerebrospinal, and other sterile uids) [12]. These improvements, however, have been implemented to varying degrees.
Although tremendous efforts have been made in Latin America
to improve surveillance systems and the diagnostic methodology
for MD, the only countries where there is evidence of routine use
of PCR are Brazil and Chile; only a limited level of PCR use occurs in
Argentina, Mexico, and Paraguay. In Chile, since 2009, RT-PCR has
been incorporated into the nal conrmation process for samples
received and processed in the Institute of Public Health. Similarly,
in Brazil, all suspected cases of MD occurring in the public and
private healthcare systems are reported to a national case-based
information system for notiable diseases (Sistema de Informaco
de Agravos de Noticaco) [43]. This system, managed by the Brazilian MoH, was implemented in 1994 and has undergone a number
of improvements over the years, the most recent occurring in 2007
when an Internet-based data transfer system was implemented
[43,44]. In Mexico, PCR conrmation has been implemented in a
limited number of hospitals since 2011, and this might lead to
increases in disease detection rates and the reliability of disease
burden information [45]. In Argentina, since 1960, it has been compulsory for provincial public hospitals to report cases of MD to the
Argentinian National Surveillance System [9]. In recent years, some
improvements have been made and laboratory-based surveillance
of invasive MD has been carried out by a national surveillance network, comprising 74 laboratories covering 23 provinces, and the
National Reference Laboratory (Administracin Nacional de Laboratorios e Institutos de Salud [ANLIS]) [46]. ANLIS is part of the
SIREVA II surveillance network. Paraguay (also part of SIREVA II) has
a surveillance system that includes molecular techniques. Most of
the molecular techniques are performed at a central public health
6534
M.A.P. Sfadi et al. / Vaccine 33 (2015) 65296536
Table 4
Incidence rates of meningococcal disease before and after meningococcal C conjugate vaccination in Brazil, 20082012 [41], copyright 2014 Oxford University Press,
reproduced by permission of Oxford University Press on behalf of the Pediatric Infectious Diseases Society.
Age groups (years)
<1
1
2
3
4
59
1014
1519
2029
3039
4049
5059
60
Total
Incidence rates (cases/100,000 population)
20082010
2011
Reduction (95% CI)
2012
Reduction (95% CI)
13.5
7.2
5.8
5.5
4.2
2.7
1.9
1.4
0.8
0.6
0.6
0.5
0.4
1.52
10.8
4.2
5.1
5.6
5.1
2.9
1.8
1.7
0.9
0.6
0.7
0.7
0.6
1.47
20% (1427)
42% (3151)
12% (221)
7.9
2.9
2.5
4.0
4.5
2.7
1.8
1.6
0.8
0.7
0.8
0.6
0.5
1.3
42% (3449)
60% (4871)
57% (4469)
27% (1738)
15% (1217)
CI, condence interval.
laboratory where all samples are sent for typing, however, PCR is
currently performed in three centers.
5.1.2. Vaccine introduction and nancing
The introduction of meningococcal vaccines into NIPs across
Latin America in the past few years can be seen as an important
achievement in the control of MD. However, there remain signicant challenges in ensuring that the best strategies, both in
terms of public health impact and cost-effectiveness, are being
implemented. For most countries, the high cost of novel vaccines, including meningococcal vaccines, signicantly increases the
cost of the NIPs. In some countries, such as Chile, meningococcal vaccines cost more than all the other vaccines in the NIPs
altogether, which is why appropriate justications for inclusion
of meningococcal vaccines have become mandatory. However,
cost-effectiveness studies are uncommon in the decision-making
process in the majority of Latin American countries. Currently,
inclusion of meningococcal vaccines in NIPs in countries with relatively good surveillance, such as Brazil and Chile, is providing
good-quality information from which other similar countries may
be able to extrapolate and learn. For example, it is becoming quite
clear that the control of meningococcal serogroup C in Brazil will
require implementation of catch-up vaccination strategies in the
adolescent population (specic age groups will need to be dened
and vaccinated, and the impact well monitored). Also in Brazil, all
outbreak-reactive vaccinations against serogroup C disease occurring are being carried out with conjugate formulations rather than
polysaccharides for all targeted age groups [47], and depending on
the outcome, this may become the recommendation for the whole
region. In Chile, the control of serogroup W will require additional
strategies aimed at decreasing the number of cases in young infants
and the elderly, as the strategy of vaccinating 15-year-olds has
had a marked impact in this age group only [39,41]. Several new
challenges are arising that will require evidence-based approaches
generated through progressively improved surveillance systems,
which will be key for improved policy decision-making processes.
Another key issue for improved vaccine use in Latin America is
vaccine affordability, and consequently, access. The PAHO Revolving Fund is a strategic mechanism [4850] that has played an
important role in improving access to available vaccines at lower
prices in Latin American (and Caribbean) countries. It works by
allowing several countries with the same vaccine needs to apply
for vaccine supplies together, increasing the overall order and
resulting in a decreased vaccine cost. Indeed, in July 2013, during
the XXI Meeting of PAHOs Technical Advisory Group on VaccinePreventable Diseases, several important recommendations were
made (see http://www.who.int/immunization/sage/meetings/
2013/november/3 PAHO TAG2013 FINAL-report.pdf) [51]. Based
on these recommendations, it is likely that the PAHO Revolving
Fund will now assist with increasing the implementation of
meningococcal vaccination. Other novel nancing arrangements
allowing more affordable vaccines have also been implemented
in some Latin American countries; in Argentina, for example, a
national company has entered into joint ventures with foreign
vaccine manufacturers able to provide technical expertise, so that
vaccines can be produced at a lower cost.
5.2. Partially met and unmet needs
Although surveillance systems are in place in Latin America,
a marked imbalance exists in the infrastructures and available
resources. This imbalance continues to be a major barrier to adoption of the best preventative strategies, especially in the regions
resource-deprived countries. The lack of sharing of surveillance
data between local and national health authorities also remains an
unmet need in many countries, such that it should be implemented
in the areas where it is lacking and strengthened where already in
place. Further improvements to the surveillance systems include
the development of infrastructures that involve both clinical case
detection as well as laboratory capacity to conrm and characterize
N. meningitidis. Even though the SIREVA II network has assisted in
this area, more work is required.
As mentioned, there is a lack of cost-effectiveness studies for the
decision-making process in medicine regarding vaccines in Latin
America. This lack of data is a major unmet need, and addressing
this might bring more balance to the way vaccination is considered
and carried out in the region. However, it should be recognized
that it may be difcult to establish a cost-effectiveness argument
for vaccination against a serious disease that has low prevalence,
such as MD.
A number of other issues that need to be considered have
been highlighted in the recent Joint Committee on Vaccination and
Immunization position statement on meningococcal B vaccine in
the United Kingdom [52]. These include the value society places on
preventing disease in its youngest members, and potential litigation costs to health authorities associated with MD.
6. Recommendations for the control and prevention of
meningococcal disease in Latin America
During its second Latin America Regional meeting, the GMI
revisited the 2011 recommendations [6]. However, additional
M.A.P. Sfadi et al. / Vaccine 33 (2015) 65296536
Table 5
Updated Global Meningococcal Initiative recommendations for reducing the global
burden of meningococcal disease (MD) in Latin America.
The establishment of a detailed and comprehensive national or regional
surveillance system is critical to assess the epidemiology and the true
disease burden of MD. In countries where limited information on the
epidemiology of MD is available, the group recommends that active
surveillance should be performed at selected sentinel sites. The data
obtained can be used to estimate incidence rates of MD once the population
under surveillance is characterized, and also provide more complete,
detailed, and accurate data on serogroup distribution, sequelae, and CFR
The group supports standardization of laboratory procedures, including
implementing molecular methods in routine testing, and reinforces the
importance of establishing well-equipped sentinel and reference
laboratories with properly trained personnel
The group recommends adoption of a uniform case denition for MD.
Supplementing PAHO criteria with diagnosis by PCR (where available) is
necessary to improve surveillance in the region and facilitate data
comparisons
The group strongly supports the importance of maintaining laboratory-based
surveillance relying on culture of CSF, blood, or other normally sterile body
uids from invasive MD cases. The use of molecular methods e.g., PCR and
RT-PCR, provides results more rapidly than culture and improves detection
rates from antibiotic-containing samples, and should supplement, not
replace, culture methods. The availability of a representative proportion of
isolates from invasive disease cases allows the determination of serogroup,
and phenotypic and genotypic characterization of the strains, including
antimicrobial resistance, and is of paramount importance in obtaining
reliable information on the circulating strains in the region
Replacement of polysaccharide vaccines with conjugate formulations
(wherever possible) for outbreak control is still relevant. Recent experience
in Brazil showed that the use of polysaccharide A/C vaccination was effective
in controlling an outbreak of serogroup C disease that occurred among
workers from an oil renery [36]. However, the polysaccharide A/C vaccine
had no effect on carriage and did not interrupt transmission to susceptible
contacts. New cases of MD continued to occur in household contacts of
vaccinated workers. These results represent a challenge to the previous
policy of using the meningococcal polysaccharide A/C vaccine to control
outbreaks of serogroup C MD, emphasizing the need to consider using MCC
vaccines rather than meningococcal polysaccharide A/C vaccines to control
serogroup C MD outbreaks
Specic recommendations for vaccination of high-risk groups should be
developed (where possible) that can be used throughout Latin America. For
these high-risk groups, the quadrivalent (ACWY) conjugate vaccines should
be the preferred vaccine. Once new protein-recombinant meningococcal
vaccines become available, they should also be recommended for these
patients. High-risk groups include those with complement deciency,
immunodeciency (including functional and anatomic asplenia and HIV),
and those at occupational risk, such as those working with microbiologic
samples or in the military
The group supports the conduct of cost-effectiveness studies in Latin America.
Ideally, cost-effectiveness analyses would be based on US or European
models, populated using data for the Latin American countries, and funded
by organizations such as PAHO
The group recommends closely monitoring and evaluating vaccination
strategies implemented in selected countries in order to determine their
impact and limitations. Sharing information can lead to the adoption of
similar or improved strategies in countries confronting new epidemiologic
situations
Vaccination should be provided, whenever possible, free of charge to those
traveling to endemic areas
CFR, case fatality rate; CSF, cerebrospinal uid; HIV, human immunodeciency virus;
MCC, meningococcal C conjugate; PAHO, Pan American Health Organization; PCR,
polymerase chain reaction; RT-PCR, real-time polymerase chain reaction.
issues were addressed during the meeting and updated recommendations were proposed, not only to improve our understanding of
the epidemiology of MD but also to reduce its public health impact
in Latin America (Table 5) [47].
Author contributions
MAPS and MO wrote the initial draft of the manuscript. All
authors have revised and reviewed the manuscript, and approved
the nal version.
6535
Conict of interest
The authors are all members of the Global Meningococcal Initiative (GMI). The GMI is funded by an educational grant from Sano
Pasteur; however, the group is not led in any way by the company.
GMI members determine meeting agenda items and lead the discussions and outputs. Sano Pasteur representatives may attend
the meetings, but in the role of observers only, and they do not
inuence the ndings of the group.
MAPS has received grants to support research projects and
speakers honoraria from GlaxoSmithKline (GSK), Novartis, Sano
Pasteur, and Pzer. MO has received a grant from Novartis to study
4CMenB in adolescents. MTVB has no further conicts or nancial
interests to declare. MCCB has received lecture fees from Pzer and
GSK. MCOG has received consultancy fees from Novartis. APSL has
received lecture fees from Novartis and Sano Pasteur. GM has no
further conicts or nancial interests to declare. JAV has received
grants to support research projects and speakers and/or consultant fees from GSK, Novartis, Sano Pasteur, Baxter BioSciences, and
Pzer. ELL has received honoraria to act as a speaker and/or consultant from Novartis, Pzer, MSD, and Sano Pasteur. M-KT performs
contract research and expertise on behalf of the Institut Pasteur
for GSK, Novartis, Pzer, and Sano Pasteur. RB performs contract
research on behalf of Public Health England for Baxter Biosciences,
GSK, Novartis, Pzer, Sano Pasteur, and Sano Pasteur MSD.
Acknowledgments
We thank the members of the GMI for reviewing and providing
input into this manuscript; in particular, Stanley Plotkin, Amando
Martin, Sarbelio Moreno Espinosa, Luz Elena Espinosa de los Monteros Perez, and Enrique Chacon-Cruz.
Medical writing support was provided by Shelley Lindley, PhD,
of PAREXEL, which was funded by Sano Pasteur.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in
the online version, at http://dx.doi.org/10.1016/j.vaccine.2015.10.
055.
References
[1] Centers for Disease Control and Prevention. Meningococcal disease. In:
Hamborsky J, Kroger A, Wolfe S, editors. Epidemiology and prevention of
vaccine-preventable diseases. Washington, DC: Public Health Foundation;
2015. http://www.cdc.gov/vaccines/pubs/pinkbook/downloads/mening.pdf.
[2] Erickson L, De Wals P. Complications and sequelae of meningococcal disease in
Quebec, Canada, 19901994. Clin Infect Dis 1998;26(5):115964.
[3] Jafri RZ, Ali A, Messonnier NE, Tevi-Benissan C, Durrheim D, Eskola J, et al.
Global epidemiology of invasive meningococcal disease. Popul Health Metr
2013;11(1):17.
[4] Masuda ET, Carvalhanas TR, Fernandes RM, Casagrande ST, Okada PS, Waldman EA. Mortality from meningococcal disease in the city of Sao Paulo, Brazil:
characteristics and predictors. Cad Saude Publica 2015;31(2):40516.
[5] Moreno G, Lopez D, Vergara N, Gallegos D, Advis MF, Loayza S. Clinical characterization of cases with meningococcal disease by W135 group in Chile, 2012.
Rev Chilena Infectol 2013;30(4):35060.
[6] Safadi MA, de Los Monteros LE, Lopez EL, Saez-Llorens X, Lemos AP, MorenoEspinosa S, et al. The current situation of meningococcal disease in Latin
America and recommendations for a new case denition from the Global
Meningococcal Initiative. Expert Rev Vaccines 2013;12(8):90315.
[7] Harrison LH, Pelton SI, Wilder-Smith A, Holst J, Safadi MA, Vazquez JA, et al.
The Global Meningococcal Initiative: recommendations for reducing the global
burden of meningococcal disease. Vaccine 2011;29(18):336371.
[8] Smith CJ, Osborn AM. Advantages and limitations of quantitative PCR (Q-PCR)based approaches in microbial ecology. FEMS Microbiol Ecol 2009;67(1):620.
[9] Safadi MA, Cintra OA. Epidemiology of meningococcal disease in Latin
America: current situation and opportunities for prevention. Neurol Res
2010;32(3):26371.
6536
M.A.P. Sfadi et al. / Vaccine 33 (2015) 65296536
[10] Safadi MA, Gonzalez-Ayala S, Jakel A, Wieffer H, Moreno C, Vyse A. The epidemiology of meningococcal disease in Latin America 19452010: an unpredictable
and changing landscape. Epidemiol Infect 2013;141(3):44758.
[11] Sacchi CT, Fukasawa LO, Goncalves MG, Salgado MM, Shutt KA, Carvalhanas
TR, et al. Incorporation of real-time PCR into routine public health surveillance of culture negative bacterial meningitis in Sao Paulo, Brazil. PLoS ONE
2011;6(6):e20675.
[12] Ibarz-Pavon AB, Lemos AP, Gorla MC, Regueira M, Gabastou JM. Laboratorybased surveillance of Neisseria meningitidis isolates from disease cases in
Latin American and Caribbean countries, SIREVA II 20062010. PLOS ONE
2012;7(8):e44102.
[13] Pan American Health Organization (PAHO). SIREVA II (Sistema de Redes
de Vigilancia de los Agentes Responsables de Neumonias y Meningitis
Bacterianas). Pan American Health Organization; 2013. http://www.paho.
org/hq/index.php?option=com content&view=article&id=5461:sireva-iisistema-de-redes-de-vigilancia-de-los-agentes-responsables-de-neumoniasy-meningitis-bacterianas-&Itemid=3953&lang=en [accessed 29.08.14].
[14] Pan American Health Organization. Case denitions: meningococcal disease.
Pan American Health Organization; 2001. http://www.paho.org/english/dd/
ais/eb v22n4.pdf [accessed 04.09.12].
[15] de Lemos AP, Yara TY, Gorla MC, de Paiva MV, de Souza AL, Goncalves MI,
et al. Clonal distribution of invasive Neisseria meningitidis serogroup C strains
circulating from 1976 to 2005 in greater Sao Paulo, Brazil. J Clin Microbiol
2007;45(4):126673.
[16] Gorla MC, de Lemos AP, Quaresma M, Vilasboas R, Marques O, de Sa MU, et al.
Phenotypic and molecular characterization of serogroup C Neisseria meningitidis associated with an outbreak in Bahia, Brazil. Enferm Infecc Microbiol Clin
2012;30(2):569.
[17] Harrison LH, Kreiner CJ, Shutt KA, Messonnier NE, OLeary M, Stefonek KR, et al.
Risk factors for meningococcal disease in students in grades 912. Pediatr Infect
Dis J 2008;27(3):1939.
[18] MacLennan J, Kafatos G, Neal K, Andrews N, Cameron JC, Roberts R, et al. Social
behavior and meningococcal carriage in British teenagers. Emerg Infect Dis
2006;12(6):9507.
[19] Harrison LH, Jolley KA, Shutt KA, Marsh JW, OLeary M, Sanza LT, et al. Antigenic shift and increased incidence of meningococcal disease. J Infect Dis
2006;193(9):126674.
[20] Kimmel SR. Prevention of meningococcal disease. Am Fam Physician
2005;72(10):204956.
[21] Borrow R, Vazquez JA, Safadi MA, Taha MK. Epidemiology and recommendations for control and prevention of meningococcal disease in Latin America:
outcomes of the Global Meningococcal Initiative meeting. In: 8th World
Congress of the World Society for Pediatric Infectious Disease (WSPID). 2013.
[22] Christensen H, May M, Bowen L, Hickman M, Trotter CL. Meningococcal
carriage by age: a systematic review and meta-analysis. Lancet Infect Dis
2010;10(12):85361.
[23] Espinosa de los Monteros LE, Aguilar-Ituarte F, Jimenez-Rojas LV, Kuri P,
Rodriguez-Suarez RS, Gomez-Barreto D. Prevalence of Neisseria meningitidis
carriers in children under ve years of age and teenagers in certain populations
of Mexico City. Salud Publica Mex 2009;51(2):1148.
[25] Rodriguez P, Alvarez I, Torres MT, Diaz J, Bertoglia MP, Carcamo M, et al.
Meningococcal carriage prevalence in university students, 1824 years of age
in Santiago, Chile. Vaccine 2014;32(43):567780.
[26] Valenzuela MT, Moreno G, Vaquero A, Seoane M, Hormazabal JC, Bertoglia MP,
et al. Emergence of W135 meningococcal serogroup in Chile during 2012. Rev
Med Chil 2013;141(8):95967.
[27] Lemos AP, Harrison LH, Lenser M, Sacchi CT. Phenotypic and molecular characterization of invasive serogroup W135 Neisseria meningitidis strains from 1990
to 2005 in Brazil. J Infect 2010;60(3):20917.
[28] Organizacin Panamericana de la Salud. Informe Regional de SIREVA II, 2006.
Datos por pas y por grupos de edad sobre las caractersticas de los aislamientos
de Streptococcus pneumoniae, Haemophilus inuenzae y Neisseria meningitidis en
procesos invasores. Pan American Health Organization; 2008. http://www1.
paho.org/Spanish/AD/THS/EV/labs Sireva II 2006.pdf [accessed 30.07.15].
[29] Organizacin Panamericana de la Salud. Informe Regional de SIREVA II.
Datos por pas y por grupos de edad sobre las caractersticas de los aislamientos de Streptococcus pneumoniae, Haemophilus inuenzae y Neisseria
meningitidis, en procesos invasores. Pan American Health Organization;
http://www.paho.org/hq/index.php?option=com docman&task=doc
2013.
download&gid=22372&Itemid=270&lang=en [accessed 30.07.15].
[30] Traore Y, Njanpop-Lafourcade BM, Adjogble KL, Lourd M, Yaro S, Nacro B, et al.
The rise and fall of epidemic Neisseria meningitidis serogroup W135 meningitis
in Burkina Faso, 20022005. Clin Infect Dis 2006;43(7):81722.
[31] Gorla MC, Grando I, de Moraes C, de Oliveira Portela C, Zanelato C, Galhardo
M, et al. Epidemiology of serogroup W135 meningococcal disease in Brazil. In:
International Pathogenic Neisseria Conference, IPNC. 2012.
[32] Lucidarme J, Hill DM, Bratcher HB, Gray SJ, du PM, Tsang RS, et al. Genomic
resolution of an aggressive, widespread, diverse and expanding meningococcal
serogroup B, C and W lineage. J Infect 2015;71(November (5)):54452.
[33] Organizacin Panamericana de la Salud. Informe Regional de SIREVA II: datos
por pas y por grupos de edad sobre las caractersticas de los aislamientos
de Streptococcus pneumoniae, Haemophilus inuenzae y Neisseria meningitidis en procesos invasores, 20002005. Pan American Health Organization;
2007. http://www1.paho.org/Spanish/AD/THS/EV/LABS-Sireva.pdf [accessed
30.07.15].
[34] Barra GN, Araya PA, Fernandez JO, Gabastou JM, Hormazabal JC, Seoane M, et al.
Molecular characterization of invasive Neisseria meningitidis strains isolated in
Chile during 20102011. PLoS ONE 2013;8(6):e66006.
[35] Abad R, Lopez EL, Debbag R, Vazquez JA. Serogroup W meningococcal disease: global spread and current affect on the Southern Cone in Latin America.
Epidemiol Infect 2014;142(12):246170.
[36] Ministerio de Salud Gobierno de Chile. Plan daccin hanta 20132014. Ministerio de Salud Gobierno de Chile; 2014. http://web.minsal.cl/node/586 [accessed
4.11.14].
[37] Ministerio de Salud Gobierno de Chile. Situacin enfermedad meningoccica.
Semana epidemiolgica 1 a 52 (01/01/2013 al 24/12/2013). Plan accin W135. Ministerio de Salud Gobierno de Chile; 2014. http://epi.minsal.cl/epi/html/
bolets/reportes/Meningitis/W135 SE522013.pdf [accessed 30.07.15].
[38] Araya P, Diaz J, Seoane M, Fernandez J, Terrazas S, Canals A, et al. Laboratory surveillance for invasive meningococcal disease in Chile, 20062012. Rev
Chilena Infectol 2014;31(4):37784.
[39] Ministrio da Sade. Meningococcal disease in Brazil. Ministrio da
Sade; 2015. http://portal.saude.gov.br/portal/saude/prossional/visualizar
texto.cfm?idtxt=3781 [accessed 30.07.15].
[40] Safadi MA, Berezin EN, Oselka GW. A critical appraisal of the recommendations for the use of meningococcal conjugate vaccines. J Pediatr (Rio J)
2012;88(3):195202.
[41] Safadi MA, Berezin EN, Ariant LH. Meningococcal disease: epidemiology and
early effects of immunization programs. J Pediatr Infect Dis 2014;3(2):913.
[42] Maiden MC, Ibarz-Pavon AB, Urwin R, Gray SJ, Andrews NJ, Clarke SC, et al.
Impact of meningococcal serogroup C conjugate vaccines on carriage and herd
immunity. J Infect Dis 2008;197(5):73743.
[43] Azevedo LC, Toscano CM, Bierrenbach AL. Bacterial meningitis in Brazil: baseline epidemiologic assessment of the decade prior to the introduction of
pneumococcal and meningococcal vaccines. PLoS ONE 2013;8(6):e64524.
[44] Galvao PR, Ferreira AT, Maciel MD, De Almeida RP, Hinders D, Schreuder
PA, et al. An evaluation of the Sinan health information system as used by
the Hansens disease control programme, Pernambuco State, Brazil. Lepr Rev
2008;79(2):17182.
[45] Espinosa de los Monteros L, Jimenez Rojas LV, Gomez Barreto D, Matias NA,
Vazquez JA, Abad R, et al. Unusual increase in meningococcal disease associated
with serogroup C ST11/ET37 in Mexico City. In: 52nd Interscience Conference
on Antimicrobial Agents and Chemotherapy. 2012.
[46] Sorhouet-Pereira C, Efron A, Gagetti P, Faccone D, Regueira M, Corso A, et al. Phenotypic and genotypic characteristics of Neisseria meningitidis disease-causing
strains in Argentina, 2010. PLoS ONE 2013;8(3):e58065.
[47] Safadi MA, Carvalhanas TR, Paula de LA, Gorla MC, Salgado M, Fukasawa LO, et al. Carriage rate and effects of vaccination after outbreaks of
serogroup C meningococcal disease, Brazil, 2010. Emerg Infect Dis 2014;20(5):
80611.
[48] Dellepiane N, Wood D. Twenty-ve years of the WHO vaccines prequalication
programme (19872012): lessons learned and future perspectives. Vaccine
2015;33(1):5261.
[49] Ministerio de Salud Gobierno de Chile, http://epi.minsal.cl/epi/html/
[accessed
30.07.15].
AtlasInteractivos/AtlasBET/ABET 01/BET 1 EM.pdf
Situacin enfermedad meningoccica por serogrupo W-135. Ministerio de
Salud Gobierno de Chile (2012). Ministerio de Salud Gobierno de Chile; 2012.
[50] Ministerio de Salud Gobierno de Chile. Situacin enfermedad meningoccica,
semana epidemiolgica (SE) 8 de 2014 (al 21/02/2014), plan accin W-135.
Ministerio de Salud Gobierno de Chile; 2014. http://epi.minsal.cl/epi/html/
bolets/reportes/Meningitis/W135 SE082014.pdf [accessed 30.07.15].
[51] Pan American Health Organization (PAHO), Accessed July 3, 2013 Vaccination:
a shared responsibility. Pan American Health Organization; 2013.
[52] Joint Committee on Vaccination and Immunisation (JCVI). JCVI position statement on use of Bexsero meningococcal B vaccine in the UK. England:
Department of Health and Public Health England; 2014.
You might also like
- WHO-PPL-Short Summary 25Feb-ET NM WHO PDFDocument7 pagesWHO-PPL-Short Summary 25Feb-ET NM WHO PDFRichard Caceda VizcondeNo ratings yet
- Nursing DelegationDocument4 pagesNursing Delegationarielsinco100% (1)
- Pathogens 11 01248Document13 pagesPathogens 11 01248Ngọc Minh Anh NguyễnNo ratings yet
- 2009guzman BlancoDocument5 pages2009guzman BlancoLuís Flávio Cozza VazNo ratings yet
- September CDC HAISDocument11 pagesSeptember CDC HAISnoval firdausNo ratings yet
- CDC Activities Initiatives For COVID 19 ResponseDocument60 pagesCDC Activities Initiatives For COVID 19 ResponseCNBC.com87% (23)
- J Rheumatol 2021 Jun 15 Fernandez-Avila DGDocument7 pagesJ Rheumatol 2021 Jun 15 Fernandez-Avila DGFernando SousaNo ratings yet
- WHO Policy Development Processes For A New Vaccine: Case Study of Malaria VaccinesDocument11 pagesWHO Policy Development Processes For A New Vaccine: Case Study of Malaria VaccinesAndi Dirhan TNo ratings yet
- Overview of Public Health Microbiology LaboratoryDocument10 pagesOverview of Public Health Microbiology LaboratoryedwineiouNo ratings yet
- Prevention of Gastric CancerDocument2 pagesPrevention of Gastric CancerAndhika Bintang MahardhikaNo ratings yet
- Antimicrobial UseDocument6 pagesAntimicrobial Usemaddy.nestebyNo ratings yet
- Current Issue DiseasesDocument14 pagesCurrent Issue Diseaseshye jinNo ratings yet
- 7057 24972 1 PBDocument133 pages7057 24972 1 PBDen NisNo ratings yet
- MN Zava 2014Document5 pagesMN Zava 2014ibrahima1968No ratings yet
- Standard Operating Procedure For ControlDocument31 pagesStandard Operating Procedure For ControlRizky PrakasaNo ratings yet
- CXG_096eDocument20 pagesCXG_096epphat8585No ratings yet
- Importance Surveillance and DetectionDocument6 pagesImportance Surveillance and Detectionsherog ahmedNo ratings yet
- Malaria Control ProgramDocument74 pagesMalaria Control ProgramMary Ruth Aujero Sanchez-Benzon100% (1)
- cdc_100571_DS1Document8 pagescdc_100571_DS15prwfqfqbmNo ratings yet
- Vaccines 12 00184Document10 pagesVaccines 12 00184Sabrina DescalzotaNo ratings yet
- Ch6 19rareDocument4 pagesCh6 19rareArmin BiparvaNo ratings yet
- 1-Introduction To PH EpidemiologyDocument33 pages1-Introduction To PH Epidemiologyrabiashoukat7888No ratings yet
- Analysis of Potential Impact of COVID-19 On Molecular Testing For Infectious Diseases MarketDocument3 pagesAnalysis of Potential Impact of COVID-19 On Molecular Testing For Infectious Diseases MarketPavan GongaleNo ratings yet
- Biological DiseasesDocument3 pagesBiological DiseasesWZ HakimNo ratings yet
- JCT 2013102511342874Document8 pagesJCT 2013102511342874RiestaKierantiNo ratings yet
- Risk of Tuberculosis Infection Among Community Health AgentsDocument6 pagesRisk of Tuberculosis Infection Among Community Health AgentsLuciana SaundersNo ratings yet
- Centers For Disease Control and Prevention's Sexually Transmitted Diseases Infection GuidelinesDocument6 pagesCenters For Disease Control and Prevention's Sexually Transmitted Diseases Infection GuidelinesabhinavrautNo ratings yet
- Propsal on Knowledge and Attitude on Hepatitis B Among Market Women in Gomoa Fetteh.Document5 pagesPropsal on Knowledge and Attitude on Hepatitis B Among Market Women in Gomoa Fetteh.emmanuelkwesizodiac1No ratings yet
- Machine Learning Model For Predicting Malaria Using Clinical Information.Document14 pagesMachine Learning Model For Predicting Malaria Using Clinical Information.xiongmao2389No ratings yet
- Developing The Next Generation of VaccinologistsDocument2 pagesDeveloping The Next Generation of VaccinologistsSukma DewiNo ratings yet
- vaccines-09-00084Document15 pagesvaccines-09-00084v2104161No ratings yet
- rr6202 PDFDocument32 pagesrr6202 PDFssami670No ratings yet
- Application of Traditional Vaccine Development Strategies To Sars-Cov-2Document41 pagesApplication of Traditional Vaccine Development Strategies To Sars-Cov-2DheerajNo ratings yet
- Enhancing Global Security Through Infectious Disease Threat ReductionDocument15 pagesEnhancing Global Security Through Infectious Disease Threat ReductionWai AbrahamNo ratings yet
- Staffing - Overview of Infection Prevention Programs - Table of Contents - APICDocument27 pagesStaffing - Overview of Infection Prevention Programs - Table of Contents - APICBassem DanielNo ratings yet
- Importance of Research Public HealthDocument12 pagesImportance of Research Public HealthConcepcion MpsNo ratings yet
- ICMR COVID 19 Call For Proposals V1Document5 pagesICMR COVID 19 Call For Proposals V1Rishabh AgarwalNo ratings yet
- 参考文献-宋老师推荐的作图风格3Document9 pages参考文献-宋老师推荐的作图风格315035689055liuhaiyangNo ratings yet
- MMWR HiB PDFDocument20 pagesMMWR HiB PDFworksheetbookNo ratings yet
- Prevention and Containment of Antimicrobial Resistance: Sixty-Third Session Bangkok, Thailand 7-10 September 2010Document17 pagesPrevention and Containment of Antimicrobial Resistance: Sixty-Third Session Bangkok, Thailand 7-10 September 2010gabriela_mariangela5929No ratings yet
- Roush Vaccine 2007Document9 pagesRoush Vaccine 2007YLNZNo ratings yet
- Gloves for COVID-19_ a Living Systematic ReviewDocument14 pagesGloves for COVID-19_ a Living Systematic ReviewAzucena Santillán GarcíaNo ratings yet
- Artigo Sobre AidsDocument7 pagesArtigo Sobre AidscamilatututNo ratings yet
- Patient Centred Surveillance of Drug Resistant PathogensDocument19 pagesPatient Centred Surveillance of Drug Resistant PathogensHanna alexanderNo ratings yet
- 2 SchistoDocument3 pages2 Schistoapi-281306164No ratings yet
- Healthcare: A Systematic Review of Healthcare-Associated Infectious Organisms in Medical Radiation Science DepartmentsDocument14 pagesHealthcare: A Systematic Review of Healthcare-Associated Infectious Organisms in Medical Radiation Science DepartmentsArina Al-KhaqNo ratings yet
- Med 1Document1 pageMed 1Roy Vincent OtienoNo ratings yet
- Standardization of Minimally Invasive Tissue Sampling Specimen Collection and Pathology Training For The Child Health and Mortality Prevention Surveillance NetworkDocument13 pagesStandardization of Minimally Invasive Tissue Sampling Specimen Collection and Pathology Training For The Child Health and Mortality Prevention Surveillance NetworkgranasamsaNo ratings yet
- A2 ModelosCOVID19Mariel22 Lerma12314Document8 pagesA2 ModelosCOVID19Mariel22 Lerma12314ALETA44No ratings yet
- World Health Organization: WHO/EMC/BAC/98.6Document5 pagesWorld Health Organization: WHO/EMC/BAC/98.6gabriela_mariangela5929No ratings yet
- SurvDocument17 pagesSurvligech195No ratings yet
- DownloadDocument14 pagesDownloadRenan de LimaNo ratings yet
- Chelsey (Chapter 2 RRL) LocalDocument3 pagesChelsey (Chapter 2 RRL) LocalChester ArenasNo ratings yet
- Cost Effectiveness of A Care Program For HIV AIDS Patients - 2016 - Value in HeDocument8 pagesCost Effectiveness of A Care Program For HIV AIDS Patients - 2016 - Value in HeSansa LauraNo ratings yet
- Uk Views On Priority Programmes For Promoting Capacity Building For Surveillance, Detection, Diagnosis and Containment of Infectious DiseasesDocument7 pagesUk Views On Priority Programmes For Promoting Capacity Building For Surveillance, Detection, Diagnosis and Containment of Infectious DiseasesDante DamiánNo ratings yet
- The Vaccine Handbook: A Practical Guide for Clinicians, Twelfth EditionFrom EverandThe Vaccine Handbook: A Practical Guide for Clinicians, Twelfth EditionNo ratings yet
- Hepatocellular Carcinoma: Translational Precision Medicine ApproachesFrom EverandHepatocellular Carcinoma: Translational Precision Medicine ApproachesYujin HoshidaNo ratings yet
- Understanding Multiple Myeloma: Recent Findings and Laboratory Investigation Updates for Biomedical Scientists: Continuing Professional Development in Pathology For Medical Laboratory ProfessionalsFrom EverandUnderstanding Multiple Myeloma: Recent Findings and Laboratory Investigation Updates for Biomedical Scientists: Continuing Professional Development in Pathology For Medical Laboratory ProfessionalsNo ratings yet
- Virologic Failure in HIV: An Updated Clinician’s Guide to Assessment and ManagementFrom EverandVirologic Failure in HIV: An Updated Clinician’s Guide to Assessment and ManagementNo ratings yet
- MJDF October 2017 New Questions & FeedbackDocument2 pagesMJDF October 2017 New Questions & Feedbacksajna1980No ratings yet
- English Asi PDFDocument3 pagesEnglish Asi PDFrujaklutisNo ratings yet
- 2018 Biotech Primer WEEKLY CompendiumDocument120 pages2018 Biotech Primer WEEKLY CompendiumAxelNo ratings yet
- Medicines in Health Systems Working Toward UHC: Presentation ScriptDocument21 pagesMedicines in Health Systems Working Toward UHC: Presentation ScriptHananAhmedNo ratings yet
- DME Assam Recruitment NoticeDocument2 pagesDME Assam Recruitment NoticekusharypragyaNo ratings yet
- STD TestsDocument1 pageSTD TestsSTDTestingNo ratings yet
- Foreword: A World-Class ICU OpensDocument6 pagesForeword: A World-Class ICU OpensAsiimwe ColinNo ratings yet
- MUNICIPALITY OF BUENAVISTABohol, PhilippinesSituational Analysis and SWOT AnalysisStakeholder Analysis With Strategic PlanCase Study With Preventive Action PlanDocument36 pagesMUNICIPALITY OF BUENAVISTABohol, PhilippinesSituational Analysis and SWOT AnalysisStakeholder Analysis With Strategic PlanCase Study With Preventive Action PlanMark Johnuel Duavis100% (1)
- Pathophysiology of Brain Abscess Secondary To Chronic Otitis MediaDocument5 pagesPathophysiology of Brain Abscess Secondary To Chronic Otitis Mediafufulabrador100% (1)
- RPM Employee Benefitguide 2023Document16 pagesRPM Employee Benefitguide 2023kcrow.bizNo ratings yet
- Data-Driven Wound Care A Business and Clinical OpportunityDocument18 pagesData-Driven Wound Care A Business and Clinical OpportunityBob RiouxNo ratings yet
- Heinert CVDocument9 pagesHeinert CVapi-608513468No ratings yet
- Form FDocument2 pagesForm FAnand Chiney100% (2)
- Godavari College of Nursing, Jalgaon: Daily Clinical Dairy ReportDocument6 pagesGodavari College of Nursing, Jalgaon: Daily Clinical Dairy ReportbuntyNo ratings yet
- Lecture 19 - AnticoagulantsDocument43 pagesLecture 19 - Anticoagulantsapi-3703352100% (1)
- Help With Health Costs: Can You Get Help With The Cost ofDocument42 pagesHelp With Health Costs: Can You Get Help With The Cost ofkhlodiaNo ratings yet
- 3864 11520 1 PBDocument22 pages3864 11520 1 PBaulia maharaniNo ratings yet
- Dissertation Topics in Rajiv Gandhi University of Health SciencesDocument7 pagesDissertation Topics in Rajiv Gandhi University of Health SciencesWhereCanIFindSomeoneToWriteMyPaperNewarkNo ratings yet
- MDV 161Document12 pagesMDV 161rasika bhatNo ratings yet
- Kajian Hukum Peran "Apoteker" Dalam Saintifikasi JamuDocument6 pagesKajian Hukum Peran "Apoteker" Dalam Saintifikasi JamuPetrisyia ReyvhonniNo ratings yet
- Week 10 - PHAR1006 Calculations - 2024 - wANSWERSDocument23 pagesWeek 10 - PHAR1006 Calculations - 2024 - wANSWERSvicrobalmarieNo ratings yet
- Collection of Soiled Contaminated &transporting Handling of EqupmentDocument3 pagesCollection of Soiled Contaminated &transporting Handling of EqupmentRAZNAS ASLAM A KNo ratings yet
- AntiBiotic Medicine by AdEel-SaiMDocument21 pagesAntiBiotic Medicine by AdEel-SaiMAdeel ur RahmanNo ratings yet
- Full Download Fuhrman & Zimmerman's Pediatric Critical Care 6th Edition Jerry J. Zimmerman PDFDocument64 pagesFull Download Fuhrman & Zimmerman's Pediatric Critical Care 6th Edition Jerry J. Zimmerman PDFdmalexuquete100% (4)
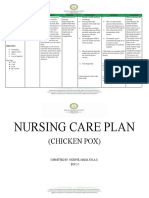
- Chicken Pox - NCPDocument2 pagesChicken Pox - NCPMaria Kyla VicenteNo ratings yet
- Shivanee Sathia ResumeDocument3 pagesShivanee Sathia Resumeapi-456295176No ratings yet
- Manifestasi Klinis, Pencegahan, PengendalianDocument34 pagesManifestasi Klinis, Pencegahan, PengendalianSelly LiLyNo ratings yet
- Wounds, Tissue Repair and ScarsDocument28 pagesWounds, Tissue Repair and ScarsShahid HameedNo ratings yet
- A Case Report of Femoral Neck Fracture in An ElderDocument7 pagesA Case Report of Femoral Neck Fracture in An ElderALIANo ratings yet