0 ratings0% found this document useful (0 votes)
166 viewsNursing Care Plan Assessment Data Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale Evaluation Independent
Nursing Care Plan Assessment Data Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale Evaluation Independent
Uploaded by
Wyeth Earl Padar Endriano Dependent on 1. Monitor vital signs
nursing: every 2 hours and
1. Administer assess respiratory
bronchodilator status.
medication as 2. Provide comfort
prescribed. measures such as
2. Provide oxygen warm mist, back
therapy as rubs, and quiet
prescribed. environment.
3. Monitor respiratory 3. Administer
status and vital bronchodilator and
signs every 2 hours. other medications as
4. Provide comfort prescribed.
measures such as 4. Monitor client's
warm mist, back response to
rubs, and quiet interventions and
environment. adjust care plan as
5.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Nursing Care Plan Assessment Data Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale Evaluation Independent
Nursing Care Plan Assessment Data Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale Evaluation Independent
Uploaded by
Wyeth Earl Padar Endriano0 ratings0% found this document useful (0 votes)
166 views3 pages Dependent on 1. Monitor vital signs
nursing: every 2 hours and
1. Administer assess respiratory
bronchodilator status.
medication as 2. Provide comfort
prescribed. measures such as
2. Provide oxygen warm mist, back
therapy as rubs, and quiet
prescribed. environment.
3. Monitor respiratory 3. Administer
status and vital bronchodilator and
signs every 2 hours. other medications as
4. Provide comfort prescribed.
measures such as 4. Monitor client's
warm mist, back response to
rubs, and quiet interventions and
environment. adjust care plan as
5.
Original Description:
asthma or COPD
Original Title
Asthma +Secretions NCP
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Dependent on 1. Monitor vital signs
nursing: every 2 hours and
1. Administer assess respiratory
bronchodilator status.
medication as 2. Provide comfort
prescribed. measures such as
2. Provide oxygen warm mist, back
therapy as rubs, and quiet
prescribed. environment.
3. Monitor respiratory 3. Administer
status and vital bronchodilator and
signs every 2 hours. other medications as
4. Provide comfort prescribed.
measures such as 4. Monitor client's
warm mist, back response to
rubs, and quiet interventions and
environment. adjust care plan as
5.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
166 views3 pagesNursing Care Plan Assessment Data Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale Evaluation Independent
Nursing Care Plan Assessment Data Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale Evaluation Independent
Uploaded by
Wyeth Earl Padar Endriano Dependent on 1. Monitor vital signs
nursing: every 2 hours and
1. Administer assess respiratory
bronchodilator status.
medication as 2. Provide comfort
prescribed. measures such as
2. Provide oxygen warm mist, back
therapy as rubs, and quiet
prescribed. environment.
3. Monitor respiratory 3. Administer
status and vital bronchodilator and
signs every 2 hours. other medications as
4. Provide comfort prescribed.
measures such as 4. Monitor client's
warm mist, back response to
rubs, and quiet interventions and
environment. adjust care plan as
5.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 3
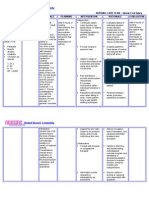
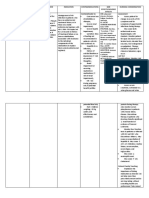
NURSING CARE PLAN
NURSING SCIENTIFIC NURSING
ASSESSMENT DATA PLANNING RATIONALE EVALUATION
DIAGNOSIS RATIONALE INTERVENTIONS
Subjective: Impaired breathing The bronchial muscles and Short term: INDEPENDENT: INdEPENDENT Short term:
“May asthma ine hiya. due to ineffective mucus glands enlarge; thick, After 2 hours of 1. Auscultate breath 1. Some degree of After 2 hours of nursing
Ngan ginkukurian hiya airway clearance tenacious sputum is nursing intervention sounds. Note bronchospasm is present intervention the patient
paghinga ngan bagat related to produced; and the alveoli the patient will be adventitious breath with obstructions in airway will be able to:
may plema niya na dire increased mucous hyperinflate. Some patients able to: sounds such as and may or may not be Participate in activities
nagagawas” as secretions and may have airway Participate in wheezes, crackles, manifested in adventitious that promotes breathing
verbalized by SO. tenacious subbasement membrane activities that or rhonchi. breath sounds, such as such as breathing
Dyspnea secretions. fibrosis. This is called airway promotes breathing 2. Assess and monitor scattered, moist crackles exercises and coughing
Anxiety “remodeling” and occurs in such as breathing respiratory rate. (bronchitis); faint sounds, exercise.
response to chronic Note inspiratory-to- with expiratory wheezes
Chest tightness exercises and
inflammation. The fibrotic expiratory ratio. (emphysema); or absent
coughing exercise. Maintain breathing and
changes in the airway lead 3. Note presence and breath sounds (severe
Objective: oxygenation in normal
to airway narrowing and degree of dyspnea. asthma)
Usage of Maintain breathing range
potentially irreversible 4. Assist client to 2. Tachypnea is usually
accessory and oxygenation in
airflow limitation maintain a present to some degree and
muscles normal range Long term:
comfortable may be pronounced on
RR 34 Source: admission, during stress, or
After 2-3 days of nursing
position to facilitate
HR 160 Medical Surgical Nursing by Long term:
breathing by during concurrent acute
intervention the patient
Weakness Brunner Suddarth 10th After 2-3 days of will be able to:
elevating the head infectious process.
Ineffective cough edition, pg. 588 nursing intervention
Respirations may be Maintain normal
the patient will be of bed, leaning on
Wheezing shallow and rapid, with performance of
over-bed table, or
able to: ADLs
Crackles sitting on edge of prolonged expiration in
Maintain comparison to inspiration Demonstrate stable
auscultated on bed.
normal 3. Respiratory dysfunction breathing pattern
the 5. Encourage and
performance is variable depending on the
treacheobronchial assist with
of ADLs abdominal or underlying process, for
area
Demonstrate pursed-lip breathing example, infection, allergic
stable exercises. reaction, and the stage of
breathing 6. Observe for chronicity in a client with
pattern. persistent, hacking, established COPD. Note:
or moist cough. Using a scale to rate
Assist with dyspnea aids in quantifying
measures to and tracking changes in
improve respiratory distress. Rapid
onset of acute dyspnea may
reflect pulmonary embolus.
effectiveness of 4. Elevation of the head of
cough effort. the bed facilitates
7. Increase fluid intake respiratory function using
to 3000 mL/day gravity; however, client in
within cardiac severe distress will seek the
tolerance. Provide position that most eases
warm or tepid breathing. Supporting arms
liquids. Recommend and legs with table, pillows,
intake of fluids and so on helps reduce
between, instead of muscle fatigue and can aid
during, meals. chest expansion.
8. Limit exposure to 5. Provides client with some
environmental means to cope with and
pollutants such as control dyspnea and reduce
dust, smoke, and air-trapping.
feather pillows 6. Cough can be persistent
according to but ineffective, especially if
individual situation client is elderly, acutely ill,
DEPENDENT: or debilitated. Coughing is
1. Artificial surfactant most effective in an upright
such as colfosceril or in a head-down position
palmitate (Exosurf) after chest percussion.
2. Provide 7. Hydration helps decrease
supplemental the viscosity of secretions,
humidification, such facilitating expectoration. 8.
as ultrasonic Precipitators of allergic type
nebulizer and of respiratory reactions that
aerosol room can trigger or exacerbate
humidifier. onset of acute episode.
3. Provide
supplemental Dependent
humidification, such 1. Research suggests
as ultrasonic aerosol
nebulizer and administration may
aerosol room enhance
humidifier. expectoration of
Source: sputum, improve
Nursing Care Plans 9th pulmonary
Edition pg. 122-124 function, and
reduce lung
volumes (air-
trapping)
2. Humidity helps
reduce viscosity of
secretions,
facilitating
expectoration, and
may reduce or
prevent formation
of thick mucous
plugs in
bronchioles.
3. Breathing exercises
help enhance
diffusion; aerosol or
nebulizer
medications can
reduce
bronchospasm and
stimulate
expectoration.
Postural drainage
and percussion
enhance removal of
excessive and sticky
secretions and
improve ventilation
of bottom lung
segments. Note:
Chest
physiotherapy may
aggravate
bronchospasm in
asthmatics.
You might also like
- Nursing Care Plan (COPD - IMBALANCE NUTRITION)Document2 pagesNursing Care Plan (COPD - IMBALANCE NUTRITION)Kathleen MartinezNo ratings yet
- Camarines Sur Polytechnic Colleges: Cues/Clues Nursing Diagnosis Plan Intervention Rationale EvaluationDocument8 pagesCamarines Sur Polytechnic Colleges: Cues/Clues Nursing Diagnosis Plan Intervention Rationale EvaluationEdelweiss Marie CayetanoNo ratings yet
- Wear and Tear TheoryDocument2 pagesWear and Tear TheoryAko ManghudNo ratings yet
- Ineffective Breathing PatternDocument3 pagesIneffective Breathing PatternReichelle Perlas64% (14)
- Ineffective Tissue PerfusionDocument5 pagesIneffective Tissue PerfusionApryll Kristin Villaluna ZafeNo ratings yet
- Filipino Culture and BeliefsDocument20 pagesFilipino Culture and BeliefsYeona BaeNo ratings yet
- NCP Drug StudyDocument5 pagesNCP Drug StudyAndrea JoyaNo ratings yet
- Nursing Care PlanDocument8 pagesNursing Care PlanssucbotNo ratings yet
- Ligaya Millare 51 F CASE: Community Acquired Pneumonia, Moderate RiskDocument6 pagesLigaya Millare 51 F CASE: Community Acquired Pneumonia, Moderate RiskNeil AlviarNo ratings yet
- Activity IntoleranceDocument4 pagesActivity IntoleranceShermane Criszen F. SallanNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Inference Goal Intervention Rationale EvaluationDocument4 pagesNursing Care Plan: Assessment Diagnosis Inference Goal Intervention Rationale EvaluationSugar Capule - ManuelNo ratings yet
- NCPDocument13 pagesNCPÍam KristineNo ratings yet
- Ineffective Airway Clearance CareplanDocument6 pagesIneffective Airway Clearance CareplanderreshaNo ratings yet
- NCP Ineffective BreathingDocument6 pagesNCP Ineffective BreathingCuttie Anne GalangNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care Planusama_salaymehNo ratings yet
- Pontine BleedingDocument99 pagesPontine BleedingJeffrey Dela CruzNo ratings yet
- NCP Acute Pain NCSDocument3 pagesNCP Acute Pain NCSPaolo Vittorio Perdigueros GonzalesNo ratings yet
- Steps of CPR ProcedureDocument8 pagesSteps of CPR ProcedureKrupa Jyothi PerumallaNo ratings yet
- Wk2 NCP Edited2012Document6 pagesWk2 NCP Edited2012Jessely Caling SalasNo ratings yet
- BSN 1 H Case Application Nursing Care PlanDocument3 pagesBSN 1 H Case Application Nursing Care PlanAntonio EscotoNo ratings yet
- NCP AnxietyDocument3 pagesNCP AnxietyNeil Alcazaren かわいいNo ratings yet
- Nursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermDocument4 pagesNursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermErika Danalle ArceoNo ratings yet
- Discharge Plan EndoDocument3 pagesDischarge Plan EndoCharlayne AnneNo ratings yet
- Predisposing Factors: Precipitating Factors: Contributing FactorsDocument6 pagesPredisposing Factors: Precipitating Factors: Contributing FactorsKen SimonNo ratings yet
- Nursing Care Plan FinalDocument4 pagesNursing Care Plan FinalSheana TmplNo ratings yet
- Nursingcribcom Nursing Care Plan Spinal Cord InjuryDocument2 pagesNursingcribcom Nursing Care Plan Spinal Cord InjuryJanine Erika Julom Brillantes100% (1)
- Ineffective Breathing PatternDocument2 pagesIneffective Breathing PatternNicole Genevie MallariNo ratings yet
- C. Diet Date Ordered Date Performed Date Changed General Description Indications Specific Foods Taken Client's Reaction And/or Reaction To The DietDocument35 pagesC. Diet Date Ordered Date Performed Date Changed General Description Indications Specific Foods Taken Client's Reaction And/or Reaction To The Dieteuqilegna_13No ratings yet
- Chapter 6 - MCNDocument2 pagesChapter 6 - MCNPrincess Queenie OlarteNo ratings yet
- NCP Risk For BleedingDocument1 pageNCP Risk For BleedingHannah ChiuNo ratings yet
- DINAWANAO3BM2PNDocument2 pagesDINAWANAO3BM2PNCherry Mae DinawanaoNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanMarielle SorianoNo ratings yet
- Asthma Nursing Care Plan NCP Ineffective Airway Clearance CompressDocument2 pagesAsthma Nursing Care Plan NCP Ineffective Airway Clearance CompressMargarette GeresNo ratings yet
- GEC 13 Prelim Exam 3Document8 pagesGEC 13 Prelim Exam 3lavadiajhonNo ratings yet
- NCP PneumoniaDocument2 pagesNCP Pneumoniajulz_otso6359No ratings yet
- NCM 200 - Preparing Administering MedicationDocument21 pagesNCM 200 - Preparing Administering MedicationjhonmarcNo ratings yet
- HyperthermiaDocument5 pagesHyperthermiaRapunzel Leanne100% (1)
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument3 pagesSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNo ratings yet
- Disharge Plan Patient'S Outcome Criteria Nursing OrderDocument2 pagesDisharge Plan Patient'S Outcome Criteria Nursing OrderDianne Loregas SanchezNo ratings yet
- NCP CopdDocument4 pagesNCP CopdMarion Dela VegaNo ratings yet
- Topic 3 NCM 112Document4 pagesTopic 3 NCM 112Marielle ChuaNo ratings yet
- EsophagomyotomyDocument3 pagesEsophagomyotomySamVelascoNo ratings yet
- NCP Acute PainDocument3 pagesNCP Acute PainSian Grace AsadaNo ratings yet
- HTP Ineffective BreathingDocument3 pagesHTP Ineffective BreathingShyrra Edades Pinder100% (1)
- 3 Chapter V-CONCEPT-ON-ORGANIZATIONAL-MANAGEMENT-finalDocument20 pages3 Chapter V-CONCEPT-ON-ORGANIZATIONAL-MANAGEMENT-finalMariane DacalanNo ratings yet
- Ineffective Tissue PerfusionDocument3 pagesIneffective Tissue Perfusionkimglaidyl bontuyanNo ratings yet
- Finals NCMB418Document24 pagesFinals NCMB418Jiro MarianoNo ratings yet
- Tonsilitis & Allergic Rhinitis NCPDocument11 pagesTonsilitis & Allergic Rhinitis NCPJorgia SalardaNo ratings yet
- Viii NCPDocument6 pagesViii NCPAdrian MangahasNo ratings yet
- BronchitisDocument129 pagesBronchitisMark Norriel CajandabNo ratings yet
- Unit 1Document16 pagesUnit 1reeta yadav0% (1)
- NCPDocument9 pagesNCPLeolene Grace BautistaNo ratings yet
- 1 Ineffective Airway ClearanceDocument8 pages1 Ineffective Airway ClearanceEsel Mae DinamlingNo ratings yet
- CMCA Case ScenarioDocument3 pagesCMCA Case ScenarioPatricia DoNo ratings yet
- NCP Case Analysis GastritisDocument7 pagesNCP Case Analysis GastritisSteffi GolezNo ratings yet
- St. Paul College of Ilocos Sur: Stages in The Natural History of Disease and The Levels of Prevention During Ncov-19Document3 pagesSt. Paul College of Ilocos Sur: Stages in The Natural History of Disease and The Levels of Prevention During Ncov-19Marie Kelsey Acena Macaraig100% (1)
- GRP 3 2 Renal Nephrectomy NCPDocument6 pagesGRP 3 2 Renal Nephrectomy NCPPam RomeroNo ratings yet
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- NCP 1 AND SOAPIE 1) Ineffective Breathing PatternDocument5 pagesNCP 1 AND SOAPIE 1) Ineffective Breathing PatternMicaela CrisostomoNo ratings yet
- NCM 120 11.3 - 4 Disaster Management Continuum (C - D) Albesa BalagaDocument9 pagesNCM 120 11.3 - 4 Disaster Management Continuum (C - D) Albesa BalagaWyeth Earl Padar EndrianoNo ratings yet
- NCM 120 - 9.3 Transitional Human Shelter-Internal Disasters and Loss of Power Loss of Medical GasesDocument5 pagesNCM 120 - 9.3 Transitional Human Shelter-Internal Disasters and Loss of Power Loss of Medical GasesWyeth Earl Padar EndrianoNo ratings yet
- PART A: Questionnaire On AttitudesDocument8 pagesPART A: Questionnaire On AttitudesWyeth Earl Padar EndrianoNo ratings yet
- PARDIÑAS Geriatric Assessment ToolDocument6 pagesPARDIÑAS Geriatric Assessment ToolWyeth Earl Padar EndrianoNo ratings yet
- CHN Program Prob 2Document2 pagesCHN Program Prob 2Wyeth Earl Padar EndrianoNo ratings yet
- NCM 120-11.7-Shelter in Place and Bugging Out-AbellaDocument5 pagesNCM 120-11.7-Shelter in Place and Bugging Out-AbellaWyeth Earl Padar EndrianoNo ratings yet
- NCM 120 9.4 Threats To Safety Loss of Telecommunications and Hospital Incident Command System CRISTINO Caber Cadiente Camacho Carson CaterialDocument3 pagesNCM 120 9.4 Threats To Safety Loss of Telecommunications and Hospital Incident Command System CRISTINO Caber Cadiente Camacho Carson CaterialWyeth Earl Padar EndrianoNo ratings yet
- Pautang AuditDocument4 pagesPautang AuditWyeth Earl Padar EndrianoNo ratings yet
- Common Areas in Terms of Activities That Is Done by An NDPDocument2 pagesCommon Areas in Terms of Activities That Is Done by An NDPWyeth Earl Padar EndrianoNo ratings yet
- Herbal Plant FormatDocument1 pageHerbal Plant FormatWyeth Earl Padar EndrianoNo ratings yet
- Chicken 11 39.29% Pig 3 10.71% Chicken, Pig 9 32.14% Chicken, Quail 1 3.57% Chicken, Rooster 1 3.57% Pig, Carabao 1 3.57% Pig, Carabao, Chicken, Duck, Goat 1 3.57% Pig, Goat, Chicken, Carabao 1 3.57%Document2 pagesChicken 11 39.29% Pig 3 10.71% Chicken, Pig 9 32.14% Chicken, Quail 1 3.57% Chicken, Rooster 1 3.57% Pig, Carabao 1 3.57% Pig, Carabao, Chicken, Duck, Goat 1 3.57% Pig, Goat, Chicken, Carabao 1 3.57%Wyeth Earl Padar EndrianoNo ratings yet
- I Lobe Lungs BananaDocument2 pagesI Lobe Lungs BananaWyeth Earl Padar EndrianoNo ratings yet
- ParacetamolDocument2 pagesParacetamolWyeth Earl Padar EndrianoNo ratings yet
- Q32-43 QUIBLAT: Table 1Document4 pagesQ32-43 QUIBLAT: Table 1Wyeth Earl Padar EndrianoNo ratings yet
- College of Nursing: Nursing On January 8, 2020, 8:00A.M. To 3:30 P.M. at Room 108, College of NursingDocument3 pagesCollege of Nursing: Nursing On January 8, 2020, 8:00A.M. To 3:30 P.M. at Room 108, College of NursingWyeth Earl Padar EndrianoNo ratings yet
- ZidovudineDocument2 pagesZidovudineWyeth Earl Padar Endriano100% (1)
- Insight Paper On Computer: Wyeth Earl P. EndrianoDocument3 pagesInsight Paper On Computer: Wyeth Earl P. EndrianoWyeth Earl Padar EndrianoNo ratings yet
- Inventory Cost Selling Price Income StatusDocument3 pagesInventory Cost Selling Price Income StatusWyeth Earl Padar EndrianoNo ratings yet
- Drug Name Mechanism of Action Indication Contraindications Side Effects/Adverse Effects Nursing ConsiderationDocument5 pagesDrug Name Mechanism of Action Indication Contraindications Side Effects/Adverse Effects Nursing ConsiderationWyeth Earl Padar EndrianoNo ratings yet
- Drug Classification Action Indication Contraindication Pharmacokinetics Adverse Effects Nursing ResponsibilitiesDocument2 pagesDrug Classification Action Indication Contraindication Pharmacokinetics Adverse Effects Nursing ResponsibilitiesWyeth Earl Padar EndrianoNo ratings yet
- Interviewer: Wyeth Earl P. Endriano Clinical Group: E Clinical Instructor: Socorro Salvacion-Gasco, D.M, H.R.M, M.N, RNDocument10 pagesInterviewer: Wyeth Earl P. Endriano Clinical Group: E Clinical Instructor: Socorro Salvacion-Gasco, D.M, H.R.M, M.N, RNWyeth Earl Padar EndrianoNo ratings yet
- Table 1. Type of Device Device Gender Total Male FemaleDocument2 pagesTable 1. Type of Device Device Gender Total Male FemaleWyeth Earl Padar EndrianoNo ratings yet
- Pautang AuditDocument4 pagesPautang AuditWyeth Earl Padar EndrianoNo ratings yet
- Is Google Making Us StupidDocument2 pagesIs Google Making Us StupidWyeth Earl Padar Endriano100% (1)
- Reflection Paper On BIll JoyDocument3 pagesReflection Paper On BIll JoyWyeth Earl Padar Endriano100% (1)
- The Good Life: A. QuestionsDocument3 pagesThe Good Life: A. QuestionsWyeth Earl Padar EndrianoNo ratings yet
- Colecistogastrostomia-Biopsia de HigadoDocument8 pagesColecistogastrostomia-Biopsia de HigadoWildor Herrera GuevaraNo ratings yet
- Motivational Interviewing and Behavior Change: How Many Times Do I Have To Tell You - ?'Document85 pagesMotivational Interviewing and Behavior Change: How Many Times Do I Have To Tell You - ?'Bubbles100% (2)
- A Novel Modified Vista Technique With Connective Tissue Graft in The Treatment of Gingival Recession - Chowdary 2020Document19 pagesA Novel Modified Vista Technique With Connective Tissue Graft in The Treatment of Gingival Recession - Chowdary 2020Natalia AcevedoNo ratings yet
- NCP 1Document2 pagesNCP 1Eva WillkomNo ratings yet
- Final OST ReportDocument21 pagesFinal OST ReportrodanyoroNo ratings yet
- Intensity of CRRT in Critically Ill PatientsDocument12 pagesIntensity of CRRT in Critically Ill PatientsAmr ElsharkawyNo ratings yet
- Surgery of The Head in Large AnimalsDocument31 pagesSurgery of The Head in Large AnimalsUNICORN TIMENo ratings yet
- Extra CreditDocument4 pagesExtra CreditGabrielle SandovalNo ratings yet
- Psychiatric Nursing Pnle 2022Document25 pagesPsychiatric Nursing Pnle 2022Bariwan FaredaNo ratings yet
- Rima DylDocument3 pagesRima DylsupravietuireNo ratings yet
- An Overview of Artificial Intelligence in Medical Physics and Radiation OncologyDocument11 pagesAn Overview of Artificial Intelligence in Medical Physics and Radiation Oncologyxiwevi4103No ratings yet
- Sensorimotor Intervention Group For Children With ADHD and Sensory Processing Dif Ficulties: A Feasibility StudyDocument13 pagesSensorimotor Intervention Group For Children With ADHD and Sensory Processing Dif Ficulties: A Feasibility StudyMageeNo ratings yet
- SOGC Clinical Guideline LiomyomaDocument22 pagesSOGC Clinical Guideline LiomyomaSarah MuharomahNo ratings yet
- DR Case Pres Updated 1Document30 pagesDR Case Pres Updated 1Ethan NamoNo ratings yet
- Article77 PDFDocument9 pagesArticle77 PDFJoão Victor horacio pires 1ano 9No ratings yet
- Electro Convulsive Therapy (Ect) : BY Mr. Kalyan Kumar MSC (N)Document22 pagesElectro Convulsive Therapy (Ect) : BY Mr. Kalyan Kumar MSC (N)kalyan kumarNo ratings yet
- Sigmund Freud - BiographyDocument2 pagesSigmund Freud - BiographyFREIMUZICNo ratings yet
- Group 5 - Percutaneous Transluminal AngioplastyDocument15 pagesGroup 5 - Percutaneous Transluminal AngioplastyKimberly Abella CabreraNo ratings yet
- Surgical Hand Scrub ProceduresDocument8 pagesSurgical Hand Scrub ProceduresArya MuhammadNo ratings yet
- Management of Asthma in PregnancyDocument59 pagesManagement of Asthma in PregnancyakokpanasNo ratings yet
- Brain Edema A. Definition of Brain EdemaDocument10 pagesBrain Edema A. Definition of Brain EdemariyafebrinaNo ratings yet
- Precipitating Factor Predisposing Factor: Case Analysis and Interventions PyschopathologyDocument1 pagePrecipitating Factor Predisposing Factor: Case Analysis and Interventions PyschopathologySydelle GravadorNo ratings yet
- Drugs: Drug - Target InteractionDocument10 pagesDrugs: Drug - Target InteractionAnil Choudhary100% (1)
- 1 Occupational Health & Hygiene-LenovaDocument22 pages1 Occupational Health & Hygiene-Lenovasamer alrawashdehNo ratings yet
- Psychopathology I 20Document16 pagesPsychopathology I 20manuelNo ratings yet
- Scripta Medica 46 2 English PDFDocument62 pagesScripta Medica 46 2 English PDFSinisa RisticNo ratings yet
- DM CBLDocument18 pagesDM CBLbpt2No ratings yet
- Mu Trash MariDocument22 pagesMu Trash MariVenkatesan VidhyaNo ratings yet
- Malaysia: Mohamad Nor Bin Mohamad TaibDocument5 pagesMalaysia: Mohamad Nor Bin Mohamad TaibAbdul Ghaffar JaafarNo ratings yet
- Tinea CapitisDocument7 pagesTinea CapitiswinNo ratings yet