0 ratings0% found this document useful (0 votes)
56 viewsNCP Format
NCP Format
Uploaded by
Cyril JavierThis document outlines a nursing care plan for a client with ineffective airway clearance. The plan includes assessing the client's symptoms, diagnosing them with ineffective airway clearance, and planning interventions like positioning, deep breathing exercises, coughing techniques, chest physiotherapy, and medication administration. The goals are for the client to clear secretions, improve oxygen levels and ventilation, and prevent further lung issues. The nurse will evaluate the client's progress in meeting these goals.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
NCP Format
NCP Format
Uploaded by
Cyril Javier0 ratings0% found this document useful (0 votes)
56 views8 pagesThis document outlines a nursing care plan for a client with ineffective airway clearance. The plan includes assessing the client's symptoms, diagnosing them with ineffective airway clearance, and planning interventions like positioning, deep breathing exercises, coughing techniques, chest physiotherapy, and medication administration. The goals are for the client to clear secretions, improve oxygen levels and ventilation, and prevent further lung issues. The nurse will evaluate the client's progress in meeting these goals.
Original Description:
FORMAT
Original Title
Ncp Format
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
This document outlines a nursing care plan for a client with ineffective airway clearance. The plan includes assessing the client's symptoms, diagnosing them with ineffective airway clearance, and planning interventions like positioning, deep breathing exercises, coughing techniques, chest physiotherapy, and medication administration. The goals are for the client to clear secretions, improve oxygen levels and ventilation, and prevent further lung issues. The nurse will evaluate the client's progress in meeting these goals.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
56 views8 pagesNCP Format
NCP Format
Uploaded by
Cyril JavierThis document outlines a nursing care plan for a client with ineffective airway clearance. The plan includes assessing the client's symptoms, diagnosing them with ineffective airway clearance, and planning interventions like positioning, deep breathing exercises, coughing techniques, chest physiotherapy, and medication administration. The goals are for the client to clear secretions, improve oxygen levels and ventilation, and prevent further lung issues. The nurse will evaluate the client's progress in meeting these goals.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 8
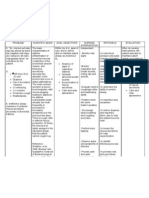
ASSESSMENT DIAGNOSIS PLANNING IMPLEMENTATION RATIONALE EVALUATION
OBJECTIVE Ineffective airway ST -Established Rapport -For the client to
clearance related to After 3 hours of nursing participate and give
-Warm to touch increased production of intervention, accurate information.
-Tachypnea secretions and The client will maintain - Elevated head of bed, - Doing so would lower
-Tachycardic increased viscosity airway patency change position the diaphragm and
-Use of accessory frequently. promote chest
muscles expansion, aeration of
-Intercostal retractions LT lung segments,
and pleuritic chestpain mobilization and
-Unilateral decrease After the shift, expectoration of
respiratory expansion The client will secretions.
-Increased tactile demonstrate - Teach and assist - Deep breathing
fremitus absence/reduction of patient with proper exercises facilitates
-Dullness to percussion congestion with breath deep-breathing maximum expansion of
-Bronchial breath sounding clear, exercises. Demonstrate the lungs and smaller
sounds noiseless respirations, proper splinting of chest airways, and improves
-Inspiratory crackles and improved oxygen and effective coughing the productivity of
-Pectoriloquy exchange while in upright cough.
-Egophony position. Encourage him Coughing is a reflex and
-Weight 72.9kgs to do so often. a natural self-cleaning
VS mechanism that assists
-BP 100/60 mmHg the cilia to maintain
-CR 115bpm patent airways. It is the
-RR 31 CPM most helpful way to
-Temp 38.6 remove most secretions.
-SpO2 89% Splinting reduces chest
discomfort and an
upright position favors
deeper and more
forceful cough effort
making it more effective
- Suction as indicated: - Stimulates cough or
frequent coughing, mechanically clears
adventitious breath airway in patient who is
sounds, desaturation unable to do so because
related to airway of ineffective cough or
secretions. decreased level of
consciousness. Note:
Suctioning can cause
increased hypoxemia;
hyper oxygenate before,
during, and after
suctioning.
- Maintain adequate - Fluids, especially warm
hydration by forcing liquids, aid in
fluids to at least 3000 mobilization and
mL/day unless expectoration of
contraindicated. Offer secretions. Fluids help
warm, rather than cold, maintain hydration and
fluids. increases ciliary action
to remove secretions
and reduces the
viscosity of secretions.
Thinner secretions are
easier to cough out.
- Assist and monitor - Nebulizers humidify
effects of nebulizer the airway to thin
treatment and other secretions and facilitates
respiratory liquefaction and
physiotherapy: incentive expectoration of
spirometer, IPPB, secretions.
percussion, postural Postural drainage may
drainage. not be as effective in
Perform treatments interstitial pneumonias
between meals and limit or those causing
fluids when appropriate. alveolar exudate or
destruction.
Incentive
spirometry serves to
improve deep breathing
and helps prevent
atelectasis.
Chest percussion helps
loosen and mobilize
secretions in smaller
airways that cannot be
removed by coughing or
suctioning.
Coordination of
treatments and oral
intake reduces
likelihood of vomiting
with coughing,
- Encourage ambulation. expectorations.
- Helps mobilize
secretions and reduces
- Administer atelectasis.
medications as indicated
- Use humidified oxygen
or humidifier at bedside. - Increasing the
humidity will decrease
the viscosity of
secretions. Clean the
humidifier before use
to avoid bacterial
growth.
- Monitor serial chest x-
rays, ABGs, pulse - Follows progress and
oximetry readings. effects and extent of
pneumonia. Therapeutic
regimen, and may
facilitate necessary
alterations in therapy.
Oxygen saturation
should be maintain at
90% or greater.
Imbalances in PaCO2
and PaO2 may indicate
respiratory fatigue.
- Anticipate the need for
supplemental oxygen or - These measures are
intubation if patient’s needed to correct
condition deteriorates. hypoxemia. Intubation is
needed for deep
suctioning efforts and
provide a source for
augmenting
oxygenation.
-
ASSESSMENT DIAGNOSIS PLANNING IMPLEMENTATION RATIONALE EVALUATION
OBJECTIVE Impaired Gas exchange ST -Established Rapport -For the client to
related to Inflammation After 3 hours of nursing participate and give
-Warm to touch of airways and alveoli intervention, accurate information.
-Tachypnea The client will - Maintain bedrest by - Prevents over
-Tachycardic demonstrate improved planning activity and exhaustion and reduces
-Use of accessory ventilation and rest periods to minimize oxygen demands to
muscles adequate oxygenation energy use. Encourage facilitate resolution of
-Intercostal retractions of tissues by ABGs use infection. Relaxation
and pleuritic chestpain within client’s usual of relaxation techniques techniques helps
-Unilateral decrease parameters and absence and diversional conserve energy that
respiratory expansion of symptoms of activities. can be used for effective
-Increased tactile respiratory distress breathing and coughing
fremitus efforts.
-Dullness to percussion - Elevate head and - These measures
-Bronchial breath LT encourage frequent promote maximum
sounds position changes, deep chest expansion,
-Inspiratory crackles After the shift, breathing, and effective mobilize secretions and
-Pectoriloquy The client will coughing. improve ventilation.
-Egophony participate in treatment
-Weight 72.9kgs regimen within level of - Administer oxygen - The purpose of oxygen
VS ability or situation therapy by appropriate therapy is to maintain
-BP 100/60 mmHg means: nasal prongs, PaO2 above 60 mmHg.
-CR 115bpm mask, Venturi mask. Oxygen is administered
-RR 31 CPM by the method that
-Temp 38.6 provides appropriate
-SpO2 89% delivery within the
patient’s tolerance.
Note: Patients with
underlying chronic lung
diseases should be given
oxygen cautiously.
ASSESSMENT DIAGNOSIS PLANNING IMPLEMENTATION RATIONALE EVALUATION
OBJECTIVE Ineffective breathing ST -Established Rapport -For the client to
pattern related to After 3 hours of nursing participate and give
-Warm to touch Decreased lung intervention, accurate information.
-Tachypnea expansion aeb using The client will - Place patient with - A sitting position
-Tachycardic accessory muscle established a normal, proper body alignment permits maximum lung
-Use of accessory effective respiratory. for maximum breathing excursion and chest
muscles pattern. expansion.
-Intercostal retractions - Encourage sustained - These techniques
and pleuritic chestpain LT deep breaths by: promotes deep
-Unilateral decrease Using demonstration: inspiration, which
respiratory expansion After the shift, highlighting slow increases oxygenation
-Increased tactile The client will initiate inhalation, holding end and prevents
fremitus needed lifestyle changes inspiration for a few atelectasis. Controlled
-Dullness to percussion seconds, and passive breathing methods may
-Bronchial breath exhalation also aid slow
sounds Utilizing incentive respirations in patients
-Inspiratory crackles spirometer who are tachypneic.
-Pectoriloquy Requiring the patient to Prolonged expiration
-Egophony yawn prevents air trapping.
-Weight 72.9kgs - Encourage - This method relaxes
VS diaphragmatic breathing muscles and increases
-BP 100/60 mmHg for patients with chronic the patient’s oxygen
-CR 115bpm disease. level.
-RR 31 CPM - Maintain a clear airway - This facilitates
-Temp 38.6 by encouraging patient adequate clearance of
-SpO2 89% to mobilize own secretions.
secretions with
successful coughing.
- Suction secretions, as - This is to clear
necessary. blockage in airway.
- Stay with the patient - This will reduce the
during acute episodes of patient’s anxiety,
respiratory distress. thereby reducing
oxygen demand.
- Ambulate patient as - Ambulation can further
tolerated with doctor’s break up and move
order three times daily. secretions that block the
- Encourage frequent airways.
rest periods and teach - Extra activity can
patient to pace activity. worsen shortness of
breath. Ensure the
patient rests between
- Encourage small strenuous activities.
frequent meals. - This prevents crowding
- Help patient with of the diaphragm
ADLs, as necessary - This conserves energy
and avoids overexertion
- Educate patient or and fatigue.
significant other proper - These allow sufficient
breathing, coughing, mobilization of
and splinting methods. secretions.
- Teach patient about:
pursed-lip breathing - These measures allow
abdominal breathing patient to participate in
performing relaxation maintaining health
techniques status and improve
performing relaxation ventilation.
techniques
taking prescribed
medications (ensuring
accuracy of dose and
frequency and
monitoring adverse
effects)
scheduling activities to
avoid fatigue and
provide for rest periods
You might also like
- Nursing Care Plan Bronchial AsthmaDocument2 pagesNursing Care Plan Bronchial Asthmaderic93% (60)
- Ards Concept MapDocument1 pageArds Concept Mapchristine louise bernardo100% (1)
- Camarines Sur Polytechnic Colleges: Cues/Clues Nursing Diagnosis Plan Intervention Rationale EvaluationDocument8 pagesCamarines Sur Polytechnic Colleges: Cues/Clues Nursing Diagnosis Plan Intervention Rationale EvaluationEdelweiss Marie CayetanoNo ratings yet
- Ineffective Breathing PatternDocument3 pagesIneffective Breathing PatternReichelle Perlas62% (13)
- Respiratory Diseases Chapter From Nelson Textbook of PediatricsDocument312 pagesRespiratory Diseases Chapter From Nelson Textbook of PediatricsMilan Andrejevic100% (1)
- NCP FormatDocument8 pagesNCP FormatMack Javier VenturaNo ratings yet
- NCP of PnuemoniaDocument13 pagesNCP of PnuemoniaFrando kenneth100% (1)
- Nursing Care PlanDocument3 pagesNursing Care Planjnx_anonymousNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument9 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationKen IgnacioNo ratings yet
- Copd NCPDocument16 pagesCopd NCPcy belNo ratings yet
- Nursing Care Plan: St. Anthony's College San Jose, Antique Nursing Department NAME:R.D.RDocument1 pageNursing Care Plan: St. Anthony's College San Jose, Antique Nursing Department NAME:R.D.Rcen janber cabrillosNo ratings yet
- Nursing Care PlanDocument8 pagesNursing Care Planalexander abasNo ratings yet
- Asthma AssessmentDocument1 pageAsthma AssessmentnarstinesirkNo ratings yet
- NCP (Monreal)Document5 pagesNCP (Monreal)Karen Joy MonrealNo ratings yet
- Assessment Background Knowledge Nursing Diagnosis Planning Intervention Rationale EvaluationDocument4 pagesAssessment Background Knowledge Nursing Diagnosis Planning Intervention Rationale EvaluationAriaNo ratings yet
- Tuberculosis Nursing Care Plan Ineffective Airway Clearance PDFDocument2 pagesTuberculosis Nursing Care Plan Ineffective Airway Clearance PDFPratiksha AmbedkarNo ratings yet
- NCP-Ineffective Airway ClearanceDocument2 pagesNCP-Ineffective Airway ClearanceTimi BCNo ratings yet
- Baiae NCPDocument1 pageBaiae NCPreignyfayeNo ratings yet
- Nursing Interventions - RespiratoryDocument4 pagesNursing Interventions - Respiratorymanager.intelligentsolutionsNo ratings yet
- Nursing Care Plan: Lopez, Maria Sofia B. 9/29/2020 3-BSN-B Prof. ZoletaDocument5 pagesNursing Care Plan: Lopez, Maria Sofia B. 9/29/2020 3-BSN-B Prof. ZoletaSofiaLopezNo ratings yet
- Acute Respiratory DistressDocument2 pagesAcute Respiratory Distressminaanne100% (4)
- UntitledDocument4 pagesUntitledPie CanapiNo ratings yet
- Task NCPDocument12 pagesTask NCPferdy ilhamNo ratings yet
- NCPPDocument11 pagesNCPPAngelo Miguel MuñozNo ratings yet
- NCP For Scenario BreathingDocument4 pagesNCP For Scenario Breathingmy moznNo ratings yet
- Lopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaDocument9 pagesLopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaSofia Lopez100% (2)
- Assess The Rate, Rhythm, and Depth of Respiration, Chest Movement, and Use of Accessory MusclesDocument4 pagesAssess The Rate, Rhythm, and Depth of Respiration, Chest Movement, and Use of Accessory MusclesjkfgNo ratings yet
- Nursing Care Plan For Pneumonia NCPDocument2 pagesNursing Care Plan For Pneumonia NCPCelline Isabelle ReyesNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument9 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationYzel Vasquez AdavanNo ratings yet
- Planning 3 NCPSDocument5 pagesPlanning 3 NCPSCuttie Anne GalangNo ratings yet
- Ineffective Airway ClearanceDocument1 pageIneffective Airway ClearancejomerdalonaNo ratings yet
- Nursing Care Plan Format TubercolosisDocument2 pagesNursing Care Plan Format TubercolosisDara AyuNo ratings yet
- Revise Nursing Care PlanDocument5 pagesRevise Nursing Care PlanNur SetsuNo ratings yet
- NCP Ineffective Airway ClearanceDocument4 pagesNCP Ineffective Airway ClearanceMary Joyce Limoico100% (1)
- Air Gets Inside The Chest CavityDocument2 pagesAir Gets Inside The Chest CavityLore Anne Mhae SantosNo ratings yet
- Nursing Care Plan Ineffective Airway Clearance Related To Tracheobronchial Secretions CAPDocument2 pagesNursing Care Plan Ineffective Airway Clearance Related To Tracheobronchial Secretions CAPLP Benoza100% (2)
- AssessmentDocument1 pageAssessmentFat NrqzNo ratings yet
- Nursing Care Plan For Pneumonia NCPDocument3 pagesNursing Care Plan For Pneumonia NCPFARAH MAE MEDINANo ratings yet
- Nursing Care Plan For Pneumonia NCP PDFDocument3 pagesNursing Care Plan For Pneumonia NCP PDFFARAH MAE MEDINA100% (2)
- Nursing Care Plan Assessment Data Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale Evaluation IndependentDocument3 pagesNursing Care Plan Assessment Data Nursing Diagnosis Scientific Rationale Planning Nursing Interventions Rationale Evaluation IndependentWyeth Earl Padar EndrianoNo ratings yet
- Nursing Diagnosis Nursing Intervention Rationale Airway ClearanceDocument7 pagesNursing Diagnosis Nursing Intervention Rationale Airway ClearanceJinaan MahmudNo ratings yet
- Ineffective Tissue PerfusionDocument5 pagesIneffective Tissue PerfusionApryll Kristin Villaluna ZafeNo ratings yet
- Cues/Clues Nursing Diagnosis Plan Intervention Rationale EvaluationDocument1 pageCues/Clues Nursing Diagnosis Plan Intervention Rationale EvaluationChristine IbiasNo ratings yet
- Nursing Care Plan Assessment Explanation of The Problem Goals and Objectives Intervention Rationale EvaluationDocument10 pagesNursing Care Plan Assessment Explanation of The Problem Goals and Objectives Intervention Rationale EvaluationGuile RilleraNo ratings yet
- Requirement in NCM 312: Presented By: Chloie Marie C. Rosalejos Submitted To: Ma. Lynn C. ParambitaDocument7 pagesRequirement in NCM 312: Presented By: Chloie Marie C. Rosalejos Submitted To: Ma. Lynn C. ParambitaChloie Marie RosalejosNo ratings yet
- Nursing Diagnosis Nursing Intervention Rationale Airway ClearanceDocument8 pagesNursing Diagnosis Nursing Intervention Rationale Airway ClearanceJinaan MahmudNo ratings yet
- NCPDocument1 pageNCPAnne Nicole ObispoNo ratings yet
- Cu 4Document3 pagesCu 4Paul SahagunNo ratings yet
- NCP (Ineffective Airway)Document2 pagesNCP (Ineffective Airway)Angeline CasabuenaNo ratings yet
- NCP Acute BronchitisDocument9 pagesNCP Acute BronchitisCarl Simon CalingacionNo ratings yet
- Ineffective Airway Clearance - PTBDocument2 pagesIneffective Airway Clearance - PTBIrish Eunice FelixNo ratings yet
- NCPDocument6 pagesNCPJoannabel RodriguezNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanRachelleNo ratings yet
- Cues Diagnosi S Desired Outcome Interventions Rationale EvaluationDocument2 pagesCues Diagnosi S Desired Outcome Interventions Rationale EvaluationYamete KudasaiNo ratings yet
- NCP 1 AND SOAPIE 1) Ineffective Breathing PatternDocument5 pagesNCP 1 AND SOAPIE 1) Ineffective Breathing PatternMicaela CrisostomoNo ratings yet
- Nursing Care Plan: Holy Name University College of Health Sciences Department of Nursing Tagbilaran City, BoholDocument4 pagesNursing Care Plan: Holy Name University College of Health Sciences Department of Nursing Tagbilaran City, BoholAllison CrookeNo ratings yet
- Nursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale Evaluationmyer pasandalanNo ratings yet
- THE WATER AND THE BREATH: A guide to using water and breathing towards a stress free and successful lifeFrom EverandTHE WATER AND THE BREATH: A guide to using water and breathing towards a stress free and successful lifeNo ratings yet
- A Simple Guide to Oxygen, Posture and Health, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Oxygen, Posture and Health, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Status Asthmaticus Case StudyDocument18 pagesStatus Asthmaticus Case Studygeorgeloto12No ratings yet
- The Human Breathing SystemDocument5 pagesThe Human Breathing SystemHarry Cianne Luther Sayon100% (1)
- Gas Exchange in Humans 1 QP PDFDocument9 pagesGas Exchange in Humans 1 QP PDFSyakir FahmieNo ratings yet
- Respiratory AssessmentDocument38 pagesRespiratory AssessmentNisha MwlzNo ratings yet
- (A. McLuckie) Respiratory Disease and Its Manageme PDFDocument169 pages(A. McLuckie) Respiratory Disease and Its Manageme PDFDerison Marsinova100% (1)
- Bio q2 Week 4Document2 pagesBio q2 Week 4Vanessa Joy TombocNo ratings yet
- Mechanical Ventilation in Pediatric PatientDocument11 pagesMechanical Ventilation in Pediatric PatientHandris YanitraNo ratings yet
- Exhale: High Concentration 60 - 90% High Flow Oxygen Non-RebreathingDocument1 pageExhale: High Concentration 60 - 90% High Flow Oxygen Non-RebreathingvharsyaNo ratings yet
- Lecure-10 Measurements of The Respiratory SystemDocument48 pagesLecure-10 Measurements of The Respiratory SystemNoor Ahmed100% (1)
- Oxygen Therapy: Citra Rencana Perangin Angin Anesthesiology Division Faculty of Medicine UKRIDADocument56 pagesOxygen Therapy: Citra Rencana Perangin Angin Anesthesiology Division Faculty of Medicine UKRIDAPaulus Apostolos Hasintongan SianturiNo ratings yet
- Kunjungan Sakit CilinayaDocument56 pagesKunjungan Sakit CilinayaAji S WidodoNo ratings yet
- Bob's - Children's Book ProjectDocument11 pagesBob's - Children's Book ProjectRunningLightxNo ratings yet
- Nursing Care Plan For PneumoniaDocument2 pagesNursing Care Plan For PneumoniaJonas Galeos100% (2)
- IAL Biology SB2 Assessment 7ADocument3 pagesIAL Biology SB2 Assessment 7AsalmaNo ratings yet
- Enote - Chapter14Document5 pagesEnote - Chapter14Aarav AroraNo ratings yet
- Kursus Critical Care Respiratory FunctionDocument63 pagesKursus Critical Care Respiratory FunctionJeyaganesh SellvarajuNo ratings yet
- ARDS Concept MapDocument1 pageARDS Concept Mapchristine louise bernardoNo ratings yet
- Dead Space The Physiology of Wasted Ventilation ERJ 2015Document13 pagesDead Space The Physiology of Wasted Ventilation ERJ 2015Javier SegoviaNo ratings yet
- Table 18-3 - Commonly Used Ventilator ModesDocument2 pagesTable 18-3 - Commonly Used Ventilator ModesDragutin PetrićNo ratings yet
- Group 2Document9 pagesGroup 2Lexter Jimenez ResullarNo ratings yet
- ATP Photosynthesis Respiration Webquest ReviewDocument2 pagesATP Photosynthesis Respiration Webquest ReviewAlayna SheltonNo ratings yet
- ABGDocument16 pagesABGKesavanVeeraNo ratings yet
- A Case Study On Bronchial Asthma in Acute ExacerbationDocument71 pagesA Case Study On Bronchial Asthma in Acute ExacerbationATEHAN BORDSNo ratings yet
- Functional Anatomy and Control of BreathingDocument34 pagesFunctional Anatomy and Control of BreathingIvan Yudha PradityaNo ratings yet
- Resusitasi NeonatusDocument7 pagesResusitasi NeonatusIqbal Miftahul HudaNo ratings yet
- Cellular Respiration Webquest DBBBBDocument5 pagesCellular Respiration Webquest DBBBB....No ratings yet
- Ats Efr 2023Document75 pagesAts Efr 2023MarcelaNo ratings yet
- Trilogy FamilyDocument2 pagesTrilogy FamilyHidayath_sharieffNo ratings yet
- NOTES CLASS7 L10 Respiration in Organisms-1Document6 pagesNOTES CLASS7 L10 Respiration in Organisms-1Blue PlayzNo ratings yet