Assessment and Concept Map Care Plan For Critical Care Patient
Assessment and Concept Map Care Plan For Critical Care Patient
Uploaded by
api-546697029Copyright:
Available Formats
Assessment and Concept Map Care Plan For Critical Care Patient
Assessment and Concept Map Care Plan For Critical Care Patient
Uploaded by
api-546697029Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Assessment and Concept Map Care Plan For Critical Care Patient
Assessment and Concept Map Care Plan For Critical Care Patient
Uploaded by
api-546697029Copyright:
Available Formats
1
Assessment and Concept Map Care Plan
For
Critical Care Patient
Created by
Abigail Collins
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
2
Step 2. Support problems with clinical patient data, including abnormal physical
assessment findings, treatments, medications, and IV’s, abnormal diagnostic and lab
tests, medical history, emotional state and pain. Also, identify key assessments that are
related to the reason for health care (chief medical diagnosis/surgical procedure) and put
these in the central box. If you do not know what box to put data in, then put it off to the
side of the map.
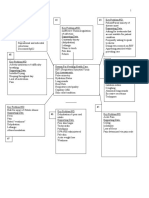
#5 Key Problem/ND: Impaired #6 Key Problems/ND: Imbalanced #7 Key Problem/ND: Risk for
Spontaneous Ventilation Nutrition: less than body Unstable Glucose
requirements
Supporting Data Supporting data:
Pt. RRT w/ severe levels of Supporting data: Hx insulin dependent T2DM
hypoxia that required ventilation NPO d/t vent Lispro sliding scale
A/C mode Dextrose drip 100 mL/hr. Dextrose drip (100 mL/hr.)
Rate 20 Albumin 3.0 BS check q. 4 hrs.
FiO2 65 Hx of diabetes (glucose check Q Last glucose level was 244
TV 470 4 hrs.) - lispro
PEEP 15 No bowel movements w/
SpO2 96 hypoactive bowel sounds
Nimbex and Fentanyl On multivitamin and vit. D
#4 Key Problem/ND: Fluid Volume
#8 Key Problem/ND: Impaired
deficit
verbal Communication
Supporting data: Reason For Needing Health Care
Supporting data:
Dark urine (Medical Dx/ Surgery)
Intubated
Oliguria Acute on chronic resp failure with hypoxia
Assess cuff pressure
Dry mucous membranes Interstitial lung disease
Nimbex
Some tenting, but not severe Hx of HFpEF, T2DM
Fentanyl
Weak pulse 56 yo male, full code
No eye opening, or response
to verbal command
Key assessment
Neuro, with assessment of therapeutic
effectiveness of paralytics
Allergies: NKA
#3 Key Problem/ND: Diminished #2 Key Problem/ND: Impaired Gas #1 Key Problem/ND: Risk for
Urine output (with a rule out for exchange drug imbalance (paralytics)
AKI)
Supporting data: Supporting data:
Supporting data: Rt. Interstitial Lung disease; Nimbex
Pt was having UO of 10 mL in 1 acute on chronic respitory failure Fentanyl
hr ABG: pH 7.4, CO2 46.2, O2 On ventilator
Fluid Challenge, failed 118, HCO3 28 Reason: fighting vent and hx of
Foley Catheter not draining urine FiO2 65 pulling out vent, Fentanyl was
BUN 71 PEEP 15 not enough to relax
Creatine 1.4 RR 20
SPO2 96 w/ FiO2 of 65
Step 3: Draw lines between related problems. Number boxes as you prioritize problems.
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
3
LASTLY- label the problem with a nursing diagnosis.
Step 4: Identification of goals, outcomes and interventions.
Step 5: Evaluation of Outcomes
Problem # 1: risk for drug imbalance r/t paralytics
General Goal: pt. will remain paralyzed and sedated safely
Predicted Behavioral Outcome Objective (s): The patient will…… not have an overresponse or underresponse
to the train-of-four test (or not breathe over vent)
on the day of care.
Nursing Interventions Patient Responses
1. Train-of-four 1. Equipment not working
2. RR 2. 20, not breathing over vent
3. Line patency 3. Line is patent (saline flush)
4. Dosage check 4. Dosage is correct with orders
5. Pain responses 5. Pt. has no response to pain
6. HR 6. HR remains at baseline of 54
7. Eye response to commands 7. Eyes do not spontaneously open
8. 8.
Evaluation of outcome objectives: pt. remains paralyzed and sedated within therapeutic range
Problem # 2: impaired gas exchange
General Goal: increased gas exchange
Predicted Behavioral Outcome Objective (s): The patient will………have ABG’s WNL and have SpO2
remain above 95
on the day of care.
Nursing Interventions Patient Responses
9. Assess breath sounds
10. Assess ABG 9. Breath sounds are becoming clear
11. Check SpO2 Q2 hrs. 10. pH 7.4 CO2 46.2 O2 118.4 HCO3 28
12. Assess chest X-ray 11. 96
12. ETT placement WDL, R>L perfusion
13. Keep HOB elevated 30 degrees
13. HOB elevated 30
14. Suction Q2 hrs.
14. No secretions
15.
15.
Evaluation of outcome objectives: Pt. ABG are in compensated resp. acidosis, SpO2 remained above 95 (at
96-98)
Problem # 3: diminished urine output
General Goal: pt will have increased urine output
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
4
Predicted Behavioral Outcome Objective (s): The patient will…… have urine output of more than 120 mL in
1 hr
on the day of care.
Nursing Interventions Patient Responses
16. Assess mucus membranes 16. dry
17. Assess skin turgor 17. some tenting
18. Fluid challenge 18. failed, no response from kidneys
19. Assess foley line 19. no sediment, not laying on line
20. Flush foley 20. received more output (50)
21. 21.
22. 22.
23. 23.
Evaluation of outcome objectives: pt. catheter line seemed to be blocked, after flushing line bag received 400
mL of urine, not AKI
Problem # 4: fluid volume deficit
General Goal: pt. will not be dehydrated
Predicted Behavioral Outcome Objective (s): The patient will…… no longer show signs of dehydration and
urine output will increase to 120 mL/hr
on the day of care.
Nursing Interventions Patient Responses
24. Assess mucus membranes 24. dry
25. Assess skin turgor 25. some tenting
26. Assess line patency 26. lines are patent
27. Check urine output 27. UO 10 ml -> 400 after flush
28. Mouth care 28. Brushed and suctioned
29. Assess pulses 29. Weak
30. 30.
31. 31.
Evaluation of outcome objectives: pt still remains dehydrated, will talk with nurse about maybe getting orders
for NS on top of dextrose, meds seem to be drying him out
Problem # 5: impaired spontaneous ventilation
General Goal: maintain ventilation
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
5
Predicted Behavioral Outcome Objective (s): The patient will…… tolerate ventilator on ordered settings and
have ease of respirations
on the day of care.
Nursing Interventions Patient Responses
32. Assess vent settings 32. AC/VC: rate 20 FiO2 65 TV 470
33. Monitor SpO2 PEEP 15
34. Mouth care q2 hrs 33. 96-98
35. RR 34. 20
36. Assess breath sounds 35. clear
37. HOB 30 degrees 36. elevated 30 degrees
38. Assess for drug therapy of 37. seems to be WDL
Fentanyl/Nimbex 38.
39. 39.
Evaluation of outcome objectives: pt. does not breathe over vent, the settings he is on seems to be allowing
ease of respirations and maintenance of ventilation
Problem # 6: imbalanced nutrition: less than body requirements
General Goal: improved nutritional status
Predicted Behavioral Outcome Objective (s): The patient will…… pt. weight will remain at 266
on the day of care.
Nursing Interventions Patient Responses
40. Assess bowel sounds 40. hypoactive
41. Assess NG placement w/ CXR 41. NG is correctly placed
and air bolus 42. Albumin 30 electrolytes WDL
42. Monitor labs 43. Bed 30 degrees
43. Elevate HOB 30 degrees 44. No stool this shift
44. Assessment of stool 45. 266
45. Weigh 46. Line is patent
46. Assess line patency 47.
47. Check dosage of dextrose Dextrose runs at 100mL/hr per orders
Evaluation of outcome objectives: pt. weight remains stable
Problem # 7: risk for unstable glucose
General Goal: pt BS will be WDL
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
6
Predicted Behavioral Outcome Objective (s): The patient will……pt. Blood glucose will be within 74-99
on the day of care.
Nursing Interventions Patient Responses
48. BS checks q 4 hrs. 48. 244
49. Insulin if needed 49. Lispro administered
50. Line patency 50. Line patent
51. Dextrose dosage check 51. Running at 100 ml/hr per orders
52. 52.
53. 53.
54. 54.
55. 55.
Evaluation of outcome objectives: pt BS still fluctuates with the need for insulin administration
Problem # 8: impaired communication
General Goal: pt. will remain sedated
Predicted Behavioral Outcome Objective (s): The patient will…… remain sedated and free of anxiety related
to the ventilator and NG tube
on the day of care.
Nursing Interventions Patient Responses
56. Neuro assessment 56. Pupils round and reactive, no
57. ETT tube placement spontaneous eye movement
58. Cuff pressure 57. ETT correctly placed, lip line same
59. NG tube placement 58. Cuff pressure normal
60. Free from pain 59. NG tube correctly placed
61. Therapeutic levels of 60. CPOT assessment 0
Nimbex/Fentanyl 61. Pt. remains safely sedated and
62. paralyzed
62.
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
7
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
8
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
9
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
10
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
11
Evaluation of outcome objectives: pt. remains sedated and unable to communicate needs. This is for his own
safety in order to maintain ETT/NG/IV-line placement (he pulls them)
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
You might also like
- STUDENT-Sepsis - Fundamental - Reasoning Fillable-1Document5 pagesSTUDENT-Sepsis - Fundamental - Reasoning Fillable-1Laura PoultneyNo ratings yet
- Beginners Guide To DigitalRXDocument14 pagesBeginners Guide To DigitalRXStarrx714No ratings yet
- Behavioral Health Care PlanDocument13 pagesBehavioral Health Care Planapi-521003884No ratings yet
- CC Concept MapDocument11 pagesCC Concept Mapapi-546355187No ratings yet
- Concept Map Finished 2Document6 pagesConcept Map Finished 2api-352785497100% (1)
- NUR 200 Tanner's Model - Noticing Through Reflecting-Updated 2020Document4 pagesNUR 200 Tanner's Model - Noticing Through Reflecting-Updated 2020Oliver NamyaloNo ratings yet
- CC Concept MapDocument6 pagesCC Concept Mapapi-741058487No ratings yet
- CC Concept MapDocument5 pagesCC Concept Mapapi-663024375No ratings yet
- Concept Map Complex Care 2017Document7 pagesConcept Map Complex Care 2017api-401537905No ratings yet
- Concept Map FinalDocument5 pagesConcept Map Finalapi-545001894No ratings yet
- Concept Map 2020Document4 pagesConcept Map 2020api-546505804No ratings yet
- Concept Map Part LLDocument5 pagesConcept Map Part LLapi-662892413No ratings yet
- 4832 Concept MapDocument7 pages4832 Concept Mapapi-508446364No ratings yet
- Concept Map CCDocument8 pagesConcept Map CCapi-402644703No ratings yet
- CC Concept Map Part LL 1Document5 pagesCC Concept Map Part LL 1api-604539767No ratings yet
- Concept MapDocument5 pagesConcept Mapapi-546509005No ratings yet
- E-Port Works Peds CMDocument5 pagesE-Port Works Peds CMapi-592360584No ratings yet
- 4832 Concept MapDocument9 pages4832 Concept Mapapi-663135887No ratings yet
- Critical Care Concept Map Template Final 2Document6 pagesCritical Care Concept Map Template Final 2api-740444719No ratings yet
- Assessment and Concept Map Care Plan: Joseph GorospeDocument5 pagesAssessment and Concept Map Care Plan: Joseph Gorospeapi-497389977No ratings yet
- Leymarie Concept MapDocument5 pagesLeymarie Concept Mapapi-546885639No ratings yet
- Concept Map Critical CareDocument6 pagesConcept Map Critical Careapi-508559825No ratings yet
- 4832 Concept MapDocument3 pages4832 Concept Mapapi-498427226No ratings yet
- Pediatric Concept MapDocument6 pagesPediatric Concept Mapapi-593213381No ratings yet
- Concept Map PedsDocument6 pagesConcept Map Pedsapi-498759347No ratings yet
- Adrenal Crises 2Document3 pagesAdrenal Crises 2s6h9jh6f47No ratings yet
- Concept Map Critical CareDocument5 pagesConcept Map Critical Careapi-546401036No ratings yet
- Concept Map Templatef21Document4 pagesConcept Map Templatef21api-741272284No ratings yet
- CC Concept Map 3-1-24Document6 pagesCC Concept Map 3-1-24api-739624128No ratings yet
- Concept Map Critical CareDocument6 pagesConcept Map Critical Careapi-498759347No ratings yet
- Concept Map Part LLDocument5 pagesConcept Map Part LLapi-663568963No ratings yet
- PediaDocument6 pagesPediaAaron Joshua PobreNo ratings yet
- Concept MapDocument10 pagesConcept Mapapi-608044542No ratings yet
- Critical Care Concept Map FinishedDocument7 pagesCritical Care Concept Map Finishedapi-604156447No ratings yet
- Ashley Wolanzyk Concept MapDocument5 pagesAshley Wolanzyk Concept Mapapi-455796674No ratings yet
- STUDENT COPD Pneumonia FUNDAMENTAL - Reasoning PDFDocument8 pagesSTUDENT COPD Pneumonia FUNDAMENTAL - Reasoning PDFYeny PenaNo ratings yet
- OB Care Plan: Assessment DataDocument10 pagesOB Care Plan: Assessment Dataapi-520858833No ratings yet
- Concept Map f21 FinishedDocument5 pagesConcept Map f21 Finishedapi-601070065No ratings yet
- 4832 Concept MapDocument7 pages4832 Concept Mapapi-739571122No ratings yet
- Concept Map Template - Andreanna TocickiDocument5 pagesConcept Map Template - Andreanna Tocickiapi-741174198No ratings yet
- Ocne 9 SupportDocument8 pagesOcne 9 Supportapi-349380871No ratings yet
- Thuy Functional DimensionDocument3 pagesThuy Functional DimensionTweetie PieNo ratings yet
- Critical Care Concept MapDocument7 pagesCritical Care Concept Mapapi-604097499No ratings yet
- Assessment and Concept Map Care PlanDocument6 pagesAssessment and Concept Map Care Planapi-508445604No ratings yet
- Clustering Data Sheet and Concept Map and Nursing Care Plan HTNDocument4 pagesClustering Data Sheet and Concept Map and Nursing Care Plan HTNAyman NabilNo ratings yet
- Case Study - RSV - (Student Version) Keith RNDocument10 pagesCase Study - RSV - (Student Version) Keith RNcrazyblondegirl2008No ratings yet
- Cirrhosis: Primary Concept Nutrition Interrelated Concepts (In Order of Emphasis)Document12 pagesCirrhosis: Primary Concept Nutrition Interrelated Concepts (In Order of Emphasis)Peggy100% (2)
- Assessment and Concept Map Care Plan: Elizabeth RouxDocument6 pagesAssessment and Concept Map Care Plan: Elizabeth Rouxapi-507304905No ratings yet
- Concept Map CCDocument7 pagesConcept Map CCapi-546473008No ratings yet
- Rle RequirementsDocument8 pagesRle RequirementsUzziel Galinea TolosaNo ratings yet
- Sheila Dalton Case Study-1Document4 pagesSheila Dalton Case Study-1tommy0% (7)
- Concept Map Done Updated PDFDocument6 pagesConcept Map Done Updated PDFapi-655682809No ratings yet
- Careplan 2 NSG 434 CCDocument8 pagesCareplan 2 NSG 434 CCapi-509642710No ratings yet
- POC and Concepts Maps Week 12Document23 pagesPOC and Concepts Maps Week 12Michelle CollinsNo ratings yet
- Concept Map Format For CLADocument41 pagesConcept Map Format For CLAAdellaine Lois GreyNo ratings yet
- Oral and Parenteral Medication Administration: Skills & Reasoning Case StudyDocument15 pagesOral and Parenteral Medication Administration: Skills & Reasoning Case StudyMary WamboltNo ratings yet
- Concept Map RSV 4Document10 pagesConcept Map RSV 4api-546577761No ratings yet
- Placenta Previa Case StudyDocument7 pagesPlacenta Previa Case StudyKing NavsunNo ratings yet
- Darunday NCP Rot 3Document12 pagesDarunday NCP Rot 3Ezra Miguel DarundayNo ratings yet
- Polarity Analysis in Homeopathy:: A Precise Path to the SimillimumFrom EverandPolarity Analysis in Homeopathy:: A Precise Path to the SimillimumRating: 5 out of 5 stars5/5 (1)
- Antonine SistersDocument3 pagesAntonine Sistersapi-546697029No ratings yet
- Copd - Capstone VideoDocument11 pagesCopd - Capstone Videoapi-546697029No ratings yet
- Health Policies and PoliticsDocument27 pagesHealth Policies and Politicsapi-546697029No ratings yet
- Abigail Collins: 3049 Main Street West Middlesex, Pennsylvania 724-301-8085Document2 pagesAbigail Collins: 3049 Main Street West Middlesex, Pennsylvania 724-301-8085api-546697029No ratings yet
- Paper Work For Seminar On Gynaecological Update For Doctors and Paramedic For State of TerengganuDocument2 pagesPaper Work For Seminar On Gynaecological Update For Doctors and Paramedic For State of TerengganuRosdi AbdullahNo ratings yet
- Shigella MCQDocument7 pagesShigella MCQSonia ThakkarNo ratings yet
- Medical Form & Document ChecklistDocument2 pagesMedical Form & Document Checklistrjadhav0075No ratings yet
- Adenomioza PDFDocument2 pagesAdenomioza PDFtraciadrianaNo ratings yet
- 2018 ESC Guidelines For The Management of Cardiovascular Disease in PregnancyDocument84 pages2018 ESC Guidelines For The Management of Cardiovascular Disease in Pregnancyasm obginNo ratings yet
- Features: Viasys Bird VIP VentilatorDocument2 pagesFeatures: Viasys Bird VIP VentilatorNana MohamedNo ratings yet
- HTN in South Asian RegDocument90 pagesHTN in South Asian RegbrolieNo ratings yet
- Mq Surgery 1920Document7 pagesMq Surgery 1920Fadhlina OmarNo ratings yet
- Acls LectureDocument15 pagesAcls LectureVincent Bautista100% (1)
- Etiopatogenesis DermatofitosisDocument8 pagesEtiopatogenesis DermatofitosisFalensia Dwita LestariNo ratings yet
- Frequencies - ListDocument171 pagesFrequencies - Listparamatman111199100% (5)
- InTechEtiology and Clinical Presentation of AstigmatismDocument26 pagesInTechEtiology and Clinical Presentation of AstigmatismAnasthasia hutagalungNo ratings yet
- Heart Rate Steps RationaleDocument3 pagesHeart Rate Steps RationaleWincy SalazarNo ratings yet
- Occlusal SplintsDocument25 pagesOcclusal SplintsSalim MalikNo ratings yet
- Katalog Astograf PDFDocument2 pagesKatalog Astograf PDFandi lenyNo ratings yet
- Edema - Symptoms and Causes - Mayo ClinicDocument2 pagesEdema - Symptoms and Causes - Mayo ClinicRafan AddisNo ratings yet
- Rosenberg's Molecular and Genetic Basis of Neurological and Psychiatric Disease Roger N. Rosenberg All Chapters Instant DownloadDocument62 pagesRosenberg's Molecular and Genetic Basis of Neurological and Psychiatric Disease Roger N. Rosenberg All Chapters Instant Downloadlallymatho100% (3)
- Te AmoDocument5 pagesTe Amoravindra1234456789No ratings yet
- ANAESTHESIA FOR GASTROINTESTINAL CANCER SURGERIES AutosavedDocument40 pagesANAESTHESIA FOR GASTROINTESTINAL CANCER SURGERIES AutosavedKavyasree KatamNo ratings yet
- Assignment ON CPCR: Submitted To: Submitted byDocument49 pagesAssignment ON CPCR: Submitted To: Submitted byGowri Sri100% (1)
- Read The Following Text Very Carefully To Get A General Impression of It, Analyze It and Then Do The Exercises That FollowDocument3 pagesRead The Following Text Very Carefully To Get A General Impression of It, Analyze It and Then Do The Exercises That FollowAinita KusmawatiNo ratings yet
- "Ni-Raspa Ako Dahil Nalalag Yung Baby Ko." As Verbalized byDocument1 page"Ni-Raspa Ako Dahil Nalalag Yung Baby Ko." As Verbalized byMary AgorillaNo ratings yet
- Menopause & Its Psychological ConsequencesDocument35 pagesMenopause & Its Psychological ConsequencesPrabhnoorNo ratings yet
- AirLiquide Hospital Eng BDDocument88 pagesAirLiquide Hospital Eng BDNandhini SivakumarNo ratings yet
- Kegunaan LinacDocument2 pagesKegunaan LinaccicichepiNo ratings yet
- Sublingual Ranula: Case Report and Review of Literature: June 2015Document4 pagesSublingual Ranula: Case Report and Review of Literature: June 2015Putri AmaliaNo ratings yet
- Running Head: Overview of Binge-Eating Disorder 1Document15 pagesRunning Head: Overview of Binge-Eating Disorder 1TatianaNo ratings yet
- Guideline For DHF-WHODocument212 pagesGuideline For DHF-WHORegir KurNo ratings yet
- Paramedic Certification Exam, 4th EditionDocument224 pagesParamedic Certification Exam, 4th EditionDanny Rivera100% (3)