Vaccinations For Age 9 To 99
Vaccinations For Age 9 To 99
Uploaded by
lolCopyright:
Available Formats
Vaccinations For Age 9 To 99
Vaccinations For Age 9 To 99
Uploaded by
lolOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Vaccinations For Age 9 To 99
Vaccinations For Age 9 To 99
Uploaded by
lolCopyright:
Available Formats
https://www.peertechzpublications.
com/journals/open-journal-of-trauma
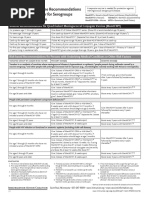
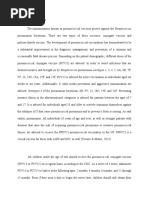
Table 3: Recommended Vaccinations [82].
Vaccination after splemectomy or in
pneumococcal Meningococcal PC influence Seasonal flu
hyposplenic status
1 dose PCV13 and 1 dose
of PPSV23 after at least 8
Vaccination in adults and children >24 weeks. 1 dose of Meningococcal ACWY
months (Unless they have already been Some authors conjugated vaccine.
1 dose 1 dose annually
fully vaccinated earlier in life for the recommended a second A series of 2 doses of Meningococcal
bacteria considered) PPSV23 dose. B vaccine at least 1 month apart.
After 5 years from the first
one.
An age-adapted PCV13
full cycle of immunization
Vaccination for children less than 24
starting from 6 weeks of
months of age. Unless already vaccinated An age-adapted full cycle of Annually (minimum age 6
life.
for the bacteria considered (in those immunization with Meningococcal B An age-adapted, full cycle months) 2 doses divided by
1 dose of PPSV 23
subjects antibiotic prophylaxis is and Meningococcal C (conjugated) of immunization with at least 4 weeks in children
(minimum age 2 years) at
recommended for at least 1 year after vaccine if younger than 12 months Haemophilus type B- aged 6 months through 8
least 8 weeks after the last
splenectomy and/or until the 3rd birthday or Meningococcal ACWY conjugated conjugated vaccine. years 1 dose for children 9
PCV 13.
whichever comes last) vaccine in > 12 months. years and older.
PPSV 23 should be
readministered only once. 3
years after the first dose.
Lifelong prophylactic antibodies should be offered to patients considered at continued high risk; aged less than
6 years or greater than 50 years, or
1) Having inadequate serological response to pnemococcal vaccination, or
2) With a history of previous invasive pneumococcal disease, or
3) Splenectomized for underlying haematological malignancy particularly in the context of on-going
Antibiotic prophylaxis after splenectomy or immunosuppression
hyposphenic status Suggested regimens:
Birth to 3rd month AMX/CLA or AMX 10 mg/kgBID
3rd month-5 years AMX 10 mg/kg BID
>5 years and adults AMX 250 mg BID
For pencillin allergic patients, probably TMP/SMX is the best option, but this should be discussed case by-case. According also
to the type of allergy in cause.
PCV13 is a Indocavalent conjugated pneumococcal and PPSV23 is a 23-valent polyvaccinide pnemoniccal vaccine. AMX Amoxicillin.
AMX XLA Amoxiccillin clavalanic, TMP SMX cotrimonozole
Table 4: WSES Class / Risk [84].
key, also to avoid serious psychological imbalances that can
ɸ WSES class AAST Haemodynamic promote episodes or suicidal thoughts [133].
Minor WSES I I-II Stable
Conclusions
Moderate WSES II III Stable
Severe WSES III IV-V Stable Therefore, it is possible to conclude the following:
WSES IV I-V Unstable
1) patients presenting with hemodynamic instability and/
or peritonitis should be referred for urgent surgical
[91,92] and depression [93] or other kinds [94-96], concerning intervention;
the near future that awaits the patient and his new quality
2) non-operative treatment of splenic lesions is now
of life; but such destabilization may hyperactivate certain
the treatment modality of choice in hemodynamically
personality traits [97-104] decompensating the patient already
stable patients, regardless of the grade of the lesion;
suffering from psychopathological disturbances [105-107] or
prior neurologically based conditions or with traumatic brain 3) the method of Non-Operative Management of splenic
comorbidity [108-120] or prone to easily altered perception trauma is confirmed as a method characterized by lower
(as in psychotic states or psychotic tendencies) [121,122], morbidity, mortality and hospitalization compared to
especially if associated with the traumatic condition there is the surgical method;
a neoplastic origin or comorbidity [123], and therefore having
4) low morbidity and overall mortality is achieved when
to resort to psychotherapeutic or psychiatric intervention
the NOM procedure is applied to an appropriate patient
[124,125] to restore the lost conditions of well-being [126-
population;
129]. Another profile of extreme clinical interest, also because
of the numerous correlations with psychological disorders, 5) nonoperative management of splenic lesions should
is intestinal dysbiosis [130-132] caused by prescribed drug only be considered in a setting that offers the possibility
therapy, which in turn can negatively affect the balance of of serious clinical monitoring and evaluations and that
intestinal flora and all its functions. These profiles, therefore, has an operating room available for 24-hour urgent
deserve greater attention and dignity, especially in a holistic laparotomies;
031
Citation: Perrotta G, Guerrieri E, Guerrieri M (2021) Splenic trauma: Definition, classifications, clinical profiles and best treatments. Open J Trauma 5(1): 019-036.
DOI: https://dx.doi.org/10.17352/ojt.000038
You might also like
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsFrom EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsRating: 5 out of 5 stars5/5 (9)
- Community Health Nursing (Pre-Test) : B. Fertilized Ascaris Lumbricoides OvaDocument2 pagesCommunity Health Nursing (Pre-Test) : B. Fertilized Ascaris Lumbricoides OvaSolsona Natl HS Maananteng100% (2)
- Philippine Childhood Immunization Schedule 2019Document8 pagesPhilippine Childhood Immunization Schedule 2019Linius Cruz67% (3)
- ChlorpromazineDocument2 pagesChlorpromazineevalyn dane50% (2)
- Asplenia ProtocolDocument5 pagesAsplenia ProtocolarjumandNo ratings yet
- Childhood Immunization Schedule 2019Document8 pagesChildhood Immunization Schedule 2019Maribel LutzNo ratings yet
- Immunization ScheduleDocument2 pagesImmunization ScheduleTracy100% (1)
- Expanded Program of ImmunizationDocument20 pagesExpanded Program of ImmunizationgwynNo ratings yet
- Pneumococcal Vaccine Timing For AdultsDocument4 pagesPneumococcal Vaccine Timing For AdultsNur Farhanah Zulkifli100% (1)
- IZSchedule0 6yrsDocument1 pageIZSchedule0 6yrsKaty ForemanNo ratings yet
- VaccinesDocument4 pagesVaccinesSam smithNo ratings yet
- Childhood Immunization 2Document7 pagesChildhood Immunization 2Dexter Carlo GutierrezNo ratings yet
- Splenectomy Updated Dec2019Document4 pagesSplenectomy Updated Dec2019Dessika ListiariniNo ratings yet
- Karla May C. Gentapan, M.D. Post-Graduate Medical Intern DMSFI Department of PediatricsDocument66 pagesKarla May C. Gentapan, M.D. Post-Graduate Medical Intern DMSFI Department of PediatricsCyril James Tagud BualNo ratings yet
- Mening Acwy RecsDocument1 pageMening Acwy Recsnlearn nNo ratings yet
- ImmunizationsDocument64 pagesImmunizationsLily BeltranNo ratings yet
- Published Assessment Report: VarilrixDocument4 pagesPublished Assessment Report: VarilrixkemalahmadNo ratings yet
- Finally Vaccine (Uw + MTB) By: ArakiDocument4 pagesFinally Vaccine (Uw + MTB) By: Arakikoki74No ratings yet
- Immunization in ChildrenDocument28 pagesImmunization in ChildrensaripjunayyahNo ratings yet
- CDC Healthcare Personnel Vaccination RecommendationsDocument1 pageCDC Healthcare Personnel Vaccination RecommendationsdocktpNo ratings yet
- Final - Back 1 PDFDocument2 pagesFinal - Back 1 PDFesbat07No ratings yet
- Childhood Immunizations: Department of PediatricsDocument17 pagesChildhood Immunizations: Department of PediatricsLyrah AlbertoNo ratings yet
- Iap Vaccination RecentDocument7 pagesIap Vaccination RecentDrNavya K UmeshNo ratings yet
- Name of Drug Classification Mechanism of Action Indication Contraindication Side Effects Nursing ResponsibilitiesDocument4 pagesName of Drug Classification Mechanism of Action Indication Contraindication Side Effects Nursing ResponsibilitiesMinaNo ratings yet
- Pneumo Vaccine TimingDocument4 pagesPneumo Vaccine TimingShenouty BNo ratings yet
- Immunisation Schedule Victoria-November 2021Document6 pagesImmunisation Schedule Victoria-November 2021Julie PanditNo ratings yet
- Splenectomy - Factsheet - For - Health - Professionals 2022 FinalDocument4 pagesSplenectomy - Factsheet - For - Health - Professionals 2022 Finalalpha.blocker11No ratings yet
- Vaccine QW5Document2 pagesVaccine QW5hajj2807No ratings yet
- Preventive PediatricsDocument111 pagesPreventive PediatricsPrincess Noreen SavellanoNo ratings yet
- HIC Vaccination Summary - C A R T E LDocument3 pagesHIC Vaccination Summary - C A R T E Lali khaledNo ratings yet
- Preventing and Treating Infections in Children With Asplenia or HypospleniaDocument5 pagesPreventing and Treating Infections in Children With Asplenia or HypospleniaAmélieNo ratings yet
- IMUNISASI2Document29 pagesIMUNISASI2RatnaSuryatiNo ratings yet
- Immunizations in Autoimmune Inflammatory Rheumatic Disease in AdultsDocument6 pagesImmunizations in Autoimmune Inflammatory Rheumatic Disease in Adultsmxg3merNo ratings yet
- Immunization Routine Table1Document11 pagesImmunization Routine Table1javiNo ratings yet
- CHS Recommended VaccinesDocument1 pageCHS Recommended Vaccineslonzell.brantleyNo ratings yet
- Do Patients Who Received Only Two Doses of Hepatitis B Vaccine Need A BoosterDocument3 pagesDo Patients Who Received Only Two Doses of Hepatitis B Vaccine Need A Boostertsiko111No ratings yet
- Altered Immunocompetence: UpdatesDocument27 pagesAltered Immunocompetence: UpdatestrishnaNo ratings yet
- DR Solis - Midterms - Preventive Pediatrics 1&2 & HandoutsDocument12 pagesDR Solis - Midterms - Preventive Pediatrics 1&2 & HandoutschristianNo ratings yet
- Raymund Christopher R. Dela Peña, RN, RM, MAN UNP-College of NursingDocument32 pagesRaymund Christopher R. Dela Peña, RN, RM, MAN UNP-College of NursingrnrmmanphdNo ratings yet
- Childhood Immunization Schedule 2021 EditedDocument11 pagesChildhood Immunization Schedule 2021 EditedPatricia Bernadette PalenciaNo ratings yet
- bexsero-epar-product-information_enDocument38 pagesbexsero-epar-product-information_ensiriteanubiatriceNo ratings yet
- COVID 19 Immunization Schedule Ages 6months OlderDocument6 pagesCOVID 19 Immunization Schedule Ages 6months OlderAlvin EvangelistaNo ratings yet
- 1 CombineDocument726 pages1 CombineSong Hành Vạn KiếpNo ratings yet
- Module 4 - Elements of Primary Health CareDocument12 pagesModule 4 - Elements of Primary Health CareAllyza Pholette DistorNo ratings yet
- Summary Document For Interim Clinical ConsiderationsDocument2 pagesSummary Document For Interim Clinical Considerationssaurabh pandey0% (1)
- Immunization and VaccinationDocument7 pagesImmunization and VaccinationRoyce GonzagaNo ratings yet
- Pneumococcal VaccineDocument1 pagePneumococcal VaccineSarah :-)No ratings yet
- Pneumococcal Vaccines: Lakshay TyagiDocument30 pagesPneumococcal Vaccines: Lakshay TyagiLakshay TyagiNo ratings yet
- 7-18yr Schedule For Immunizations, CDC 2008Document1 page7-18yr Schedule For Immunizations, CDC 2008Tracy100% (1)
- Childhood Immunization Schedule 2021Document11 pagesChildhood Immunization Schedule 2021Paula QuiñonesNo ratings yet
- Week 4 Peer ResponseDocument3 pagesWeek 4 Peer ResponseMayumi BalmesNo ratings yet
- Adult Immunization Schedule by Vaccine and Age Group - CDCDocument17 pagesAdult Immunization Schedule by Vaccine and Age Group - CDCCamacaro Arevalo JoseNo ratings yet
- Pneumonia VaccinesDocument4 pagesPneumonia Vaccinesapi-237094717No ratings yet
- Vaccine Timing CDCDocument40 pagesVaccine Timing CDCanindita.prasidha.parameswariNo ratings yet
- Ijn 26 7Document8 pagesIjn 26 7Alex WayneNo ratings yet
- Vibriosis Vaccine (Inactivated) For Sea BassDocument2 pagesVibriosis Vaccine (Inactivated) For Sea BassaymenbiogalenicNo ratings yet
- Vaccination SchedDocument9 pagesVaccination SchedDaihachi DaimeNo ratings yet
- Pediatria Integral XIX 9 - WEB PDFDocument98 pagesPediatria Integral XIX 9 - WEB PDFIvan BurgosNo ratings yet
- Artikel 1Document3 pagesArtikel 1Dieni Rhdezscpecjthor UnityNo ratings yet
- The Routine Immunisation ScheduleDocument10 pagesThe Routine Immunisation ScheduleJamesWaitonNo ratings yet
- Table I IAP Immunization Schedule 2016 FinalDocument7 pagesTable I IAP Immunization Schedule 2016 FinalVaishnavi AgrawalNo ratings yet
- A Statistical Inquiry Into the Nature and Treatment of EpilepsyFrom EverandA Statistical Inquiry Into the Nature and Treatment of EpilepsyNo ratings yet
- Blood TransfusionDocument8 pagesBlood TransfusionAlthea AlcalaNo ratings yet
- Neonatal JaundiceDocument5 pagesNeonatal JaundiceIzwan KyNo ratings yet
- Epidemiology and Pathophysiology of Colonic Diverticular DiseaseDocument8 pagesEpidemiology and Pathophysiology of Colonic Diverticular DiseaseAnonymous Hz5w55No ratings yet
- Conversation Between ProfessionsDocument3 pagesConversation Between ProfessionsHeryani AnikNo ratings yet
- Pubic Health SurvilanceDocument28 pagesPubic Health Survilanceteklay100% (2)
- Cardiology - Video - Slides KaplanDocument51 pagesCardiology - Video - Slides KaplanAishwarya RaghuramNo ratings yet
- Drugs Acting On CNSDocument32 pagesDrugs Acting On CNSjustin rodrigoNo ratings yet
- HIVand Texas LawDocument2 pagesHIVand Texas LawForfamNo ratings yet
- Workshop On Early Warning Score System - Ali HaedarDocument61 pagesWorkshop On Early Warning Score System - Ali HaedarGede Kevin Adhitya SaputraNo ratings yet
- Keys Shah - SCI CW Genetics Project Research 114 - 15721804Document3 pagesKeys Shah - SCI CW Genetics Project Research 114 - 15721804keysha31No ratings yet
- Urinary Incontinence in Older Adults.25Document6 pagesUrinary Incontinence in Older Adults.25citraNo ratings yet
- Twinrix Product MonographDocument27 pagesTwinrix Product Monographandy175No ratings yet
- Ebook StrokeDocument195 pagesEbook StrokeLaurenz KilmanunNo ratings yet
- Biofeedback Therapy in Pune - Dr. Rupali Bandgar-JankarDocument3 pagesBiofeedback Therapy in Pune - Dr. Rupali Bandgar-JankardrrupalibandgarNo ratings yet
- Thyroid Disorder: by DR - Wael MetwalyDocument9 pagesThyroid Disorder: by DR - Wael MetwalysardashtiNo ratings yet
- Ramadan Guide For DiabetesDocument9 pagesRamadan Guide For DiabetesUjwal TickooNo ratings yet
- 103057Document49 pages103057ohridiftNo ratings yet
- This Patient Have A Hemorrhagic StrokeDocument7 pagesThis Patient Have A Hemorrhagic StrokeMario ARNo ratings yet
- Berra 2020Document12 pagesBerra 2020Indri AswariNo ratings yet
- 2015 - October - PD Mind and Memory With FlyersDocument53 pages2015 - October - PD Mind and Memory With Flyersapi-280025964No ratings yet
- Cranium 3Document26 pagesCranium 3giant nitaNo ratings yet
- Mind MapsDocument5 pagesMind MapsMaahin IbrahimNo ratings yet
- COVID 19 Ab Fact SheetDocument4 pagesCOVID 19 Ab Fact Sheet10tenharmonyNo ratings yet
- RPP MfaDocument10 pagesRPP MfaIZZAT DANAZZATNo ratings yet
- Case Presentation On Acute Infectious Diarrhea By: Francis B. Aquino Som - IiiDocument10 pagesCase Presentation On Acute Infectious Diarrhea By: Francis B. Aquino Som - IiiCalingalan Hussin CaluangNo ratings yet
- HysterectomyDocument24 pagesHysterectomypt.mahmoudNo ratings yet
- Prescription J d8z c2jjm56sUcPPQmHsPxI216ZuVp2dT3jXJWSBHrFMo69w6N3I92ftygTLEXDocument2 pagesPrescription J d8z c2jjm56sUcPPQmHsPxI216ZuVp2dT3jXJWSBHrFMo69w6N3I92ftygTLEXafreensiddique1771No ratings yet
- List of BacteriaDocument3 pagesList of BacteriaSol T. ParedesNo ratings yet