Review
Review
Uploaded by
karanwavhal47Copyright:
Available Formats
Review
Review
Uploaded by
karanwavhal47Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Review
Review
Uploaded by
karanwavhal47Copyright:
Available Formats
C L I N I C A L SIGNIF ICANCE OF MINIMAL RE SID UA L D IS EASE IN C H ILD H OOD AC UTE LY MPH OBL ASTIC LEUK EM IA
CLINICAL SIGNIFICANCE OF MINIMAL RESIDUAL DISEASE IN CHILDHOOD
ACUTE LYMPHOBLASTIC LEUKEMIA
HÉLÈNE CAVÉ, PH.D., JUTTE VAN DER WERFF TEN BOSCH, M.D., STEFAN SUCIU, M.S., CHRISTINE GUIDAL, M.S.,
CHRISTINE WATERKEYN, M.S., JACQUES OTTEN, M.D., MARLEEN BAKKUS, PH.D., KRIS THIELEMANS, M.D.,
BERNARD GRANDCHAMP, PH.D., M.D., AND ETIENNE VILMER, M.D., FOR THE
EUROPEAN ORGANIZATION FOR RESEARCH AND TREATMENT OF CANCER–CHILDHOOD LEUKEMIA COOPERATIVE GROUP
ABSTRACT yses4,5,8 or have involved a small number of patients
Background and Methods The implications of the who were sometimes treated with different proto-
detection of residual disease after treatment of acute cols. Furthermore, the course of residual disease has
lymphoblastic leukemia (ALL) are unclear. We con- varied considerably in some studies.4,6-10
ducted a prospective study at 11 centers to deter- In a pilot study, we validated the method of
mine the predictive value of the presence or absence quantitating residual blasts in the marrow with a
of detectable residual disease at several points in time competitive PCR assay.11 This method uses the re-
during the first six months after complete remission arranged T-cell–receptor or immunoglobulin heavy-
of childhood ALL had been induced. Junctional se-
chain genes of the leukemic blasts as clonal markers.
quences of T-cell–receptor or immunoglobulin gene
rearrangements were used as clonal markers of leu- We found that quantitation of residual leukemia dur-
kemic cells. Residual disease was quantitated with a ing the first months of remission can help identify
competitive polymerase-chain-reaction (PCR) assay. patients who are likely to have a relapse.11 We under-
Of 246 patients enrolled at diagnosis and treated took this prospective study to extend our prelimi-
with a uniform chemotherapy protocol, 178 were nary findings.
monitored for residual disease with one clone-spe-
cific probe (in 74 percent) or more than one probe (in METHODS
26 percent). The median follow-up period was 38 Treatment
months.
We used the Berlin–Frankfurt–Munster (BFM) treatment pro-
Results The presence or absence and level of re- tocol with minor modifications (European Organization for Re-
sidual leukemia were significantly correlated with the search and Treatment of Cancer [EORTC] protocol 58881).12 In
risk of early relapse at each of the times studied brief, after one week of treatment with prednisolone and one
(P<0.001). PCR measurements identified patients at intrathecal injection of methotrexate, induction therapy was be-
high risk for relapse after the completion of induction gun. It consisted of a five-drug regimen given over a period of
therapy (those with »10¡2 residual blasts per 2¬105 four weeks (daily prednisolone, weekly vincristine and daunoru-
mononuclear bone marrow cells) or at later time bicin, asparaginase twice weekly, and intrathecal methotrexate on
points (those with »10¡3 residual blasts). Multivariate days 8 and 22). After the completion of this treatment, patients
analysis showed that as compared with immunophe- who had had more than 1000 blasts per cubic millimeter of blood
at the end of the first week of prednisolone treatment, those who
notype, age, risk group (standard or very high risk),
did not have a complete remission, and those with the t(4;11) or
and white-cell count at diagnosis, the presence or ab- t(9;22) translocation were classified as having a very high risk of
sence and level of residual disease were the most relapse. All other patients were classified as having a standard risk.
powerful independent prognostic factors. Patients with a standard risk of relapse received four weeks of
Conclusions Residual leukemia after induction of consolidation therapy, consisting of daily mercaptopurine, four
a remission is a powerful prognostic factor in child- four-day courses of cytarabine, and cyclophosphamide on days
hood ALL. Detection of residual disease by PCR
should be used to identify patients at risk for relapse
and should be taken into account in considering al- From the Laboratoire de Biochimie Génétique and the Service d’Hé-
ternative treatment. (N Engl J Med 1998;339:591-8.) mato-Immunologie, Hôpital Robert Debré, Paris (H.C., C.G., B.G., E.V.);
©1998, Massachusetts Medical Society. the Department of Physiology, Vrige Universiteit Brussel, Brussels, Bel-
gium (J.W.B., M.B., K.T.); the European Organization for Research and
Treatment of Cancer Data Center, Brussels, Belgium (S.S., C.W.); and the
Akademisch Ziekenhuis, Vrige Universiteit Brussel, Brussels, Belgium
(J.O.). Address reprint requests to Dr. Vilmer at the Service d’Hémato-
D
Immunologie, Hôpital Robert Debré, 48 Blvd. Serurier, 75019 Paris,
ESPITE advances in the treatment of France.
childhood acute lymphoblastic leukemia Other authors were Brigitte Nelken and Martine Fournier (Centre Hos-
(ALL), the risk of relapse remains about pitalier Universitaire, Lille, France), Patrick Boutard and Emmanuel Le-
brun (Centre Hospitalier Universitaire, Caen, France), Françoise Méchi-
30 percent. Studies have shown that the naud and Richard Garand (Centre Hospitalier Régional Hôtel Dieu, Nantes,
presence or absence of residual disease, as assessed France), Alain Robert and Nicole Dastugue (Centre Hospitalier Universi-
taire, Toulouse, France), Emmanuel Plouvier and Evelyne Racadot (Centre
by the polymerase-chain-reaction (PCR) assay, can Hospitalier Régional, Besançon, France), Alice Ferster (Centre Hospitalier
serve as a prognostic factor in patients with ALL,1-4 Universitaire, Reine Fabiola, Brussels, Belgium), Jan Gyselinck (Algemeen
and threshold levels of residual leukemic cells have Kinderziekenhuis, Antwerp, Belgium), Odile Fenneteau and Michel Duval
(Hôpital Robert Debré, Paris), Gabriel Solbu (European Organization for
been proposed for predicting relapse.5-10 However, Research and Treatment of Cancer Data Center, Brussels, Belgium), and
many of the studies have been retrospective anal- Anne-Marie Manel (Centre Hospitalier Régional, Lyons, France).
Vol ume 33 9 Numb e r 9 · 591
The New England Journal of Medicine
Downloaded from nejm.org on September 28, 2024. For personal use only.
No other uses without permission. Copyright © 1998 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
1 and 28. This consolidation phase was followed by an eight-week Bone marrow samples from all patients were obtained at the time
course of daily mercaptopurine and four courses of high-dose of diagnosis and at the end of induction therapy. In the standard-
methotrexate (interval therapy). A delayed intensification phase risk group, samples were obtained after consolidation, interval,
consisted of dexamethasone (for 3 weeks), four weekly injections and delayed intensification treatments. In the very-high-risk group,
of vincristine and doxorubicin, and four injections of asparaginase samples were obtained on completion of intensified consolidation
(protocol IIA), followed by daily thioguanine (for 14 days), one therapy, which was given after induction therapy. Bone marrow
injection of cyclophosphamide, two courses of cytarabine, and samples were analyzed at one of two reference laboratories (in
one intrathecal injection of methotrexate (protocol IIB). The du- Brussels, Belgium, and in Paris) for the detection of residual dis-
ration of treatment from the start of induction therapy to the ease. Quantitative analysis was performed at a single laboratory
completion of the delayed intensification phase was about 27 (in Paris) for all samples in which residual leukemia was detected.
weeks. Delayed intensification therapy was followed by mainte- Personnel at both laboratories were unaware of the patients’ sta-
nance treatment consisting of daily mercaptopurine and weekly tus at the time the samples were assayed. Clinical and molecular
methotrexate. The total duration of treatment was two years. data were centralized at the EORTC data center, where the sta-
Patients at very high risk for relapse received intensified consol- tistical analysis was performed.
idation therapy of six weeks’ duration, consisting of cyclophos-
phamide, high-dose methotrexate and cytarabine, asparaginase, Patients
and oral mercaptopurine, followed by two series of three chemo-
therapeutic courses according to the BFM relapse protocol.13 A total of 246 children with ALL were enrolled in the study at
the time of diagnosis. The enrollment period started in Novem-
Detection of Residual Disease ber 1989 (at 1 center) or July 1993 (at 10 centers) and ended in
March 1996. Four patients were excluded because they did not
Bone marrow mononuclear cells were counted, lysed, and have a remission, defined by the detection of fewer than 5 percent
stored at ¡20°C until analysis. Rearrangements of the T-cell– blasts in bone marrow smears, which were independently re-
receptor genes TCRg (V1–J1,2; V1–JP1,2; and V9–J1,2) and viewed by two cytologists. At least three bone marrow samples
TCRd (V2–D3, V1–J1, D2–D3, and V2–J1) were sought in from each patient were studied, with the exception of patients
samples obtained at the time of diagnosis.11,14 If none of these re- who had relapses before delayed intensification therapy was com-
arrangements were detected, rearrangements of the gene for im- pleted. Sixteen patients were excluded because fewer than three
munoglobulin heavy chain (IgH ) were sought with the use of follow-up bone marrow samples were obtained.
consensus FRIII and JH primers.15 The presence or absence of Among the remaining 226 patients, no gene rearrangements
such clonal markers was determined after polyacrylamide-gel elec- were detected in 25 (11 percent), whereas at least one rearrange-
trophoresis. Discrete bands of PCR products corresponding to ment was detected in 201 (89 percent). TCRd was rearranged in
clonal rearrangements were sequenced. An oligonucleotide probe 115 of 188 patients (61 percent) with B-lineage ALL and in 14
specific for the junctional sequence was synthesized for each re- of 38 (37 percent) with T-lineage ALL. TCRg was rearranged in
arrangement. Tests for residual disease were conducted by PCR 108 patients (57 percent) with B-lineage ALL and in 32 (84 per-
amplification of 2¬105 mononuclear bone marrow cells in sam- cent) with T-lineage ALL. An IgH rearrangement was detected
ples obtained during remission, with the use of the primer set in 12 of 32 patients (38 percent) with B-lineage ALL in whom
corresponding to the T-cell or B-cell clonal rearrangement iden- no TCRd or TCRg rearrangement was detected.
tified at the time of diagnosis. PCR products were dot-blotted In 23 of 201 patients with at least one rearrangement, no
and hybridized to the radiolabeled clone-specific probe.11 probe could be obtained because of an oligoclonal pattern of re-
All frozen samples obtained at all time points from a given pa- arrangement or biallelic rearrangements that were unsuitable for
tient were run at the same time. The specificity of detection was good electrophoretic separation. At least one clone-specific probe
checked for each probe on at least two different polyclonal sam- was available for 178 patients, who formed the study group. Re-
ples. The sensitivity of each probe was assessed by testing serial sidual disease was evaluated with the use of a single probe in 132
dilutions of the patient’s blasts in a mixture of polyclonal marrow patients (74 percent) and with two or more probes in 46 patients
mononuclear cells. The median level of detection was 5¬10¡5 (26 percent). One or more TCRd probes were used alone in 64
(i.e., 5 blasts per 100,000 normal mononuclear cells). For the sta- patients (36 percent), one or more TCRg probes were used alone
tistical analyses, the results were considered negative only if the in 83 patients (47 percent), both TCRd and TCRg probes were
level detected was less than 1.5¬10¡4. used in 19 patients (11 percent), and one or more IgH probes
We used a competitive PCR assay to quantitate residual blasts. were used alone in 12 patients (7 percent). In 18 patients, residual
Amplification was carried out as for blast detection in the pres- disease was detected but could not be quantitated because the
ence of 100 copies of internal standard in each PCR sample. In- samples were inadequate. Data for the 25 patients in the pilot
ternal standards consisted of DNA from monoclonal cells that study11 were included in the statistical analysis.
had a rearrangement involving the same genomic segments as the The comparability of our patients with the general population
patient’s blasts but with a distinct junctional sequence. Each PCR of children with ALL was evaluated by comparing the outcomes
series included serial dilutions of the patient’s blasts. PCR prod- in our group with those among the 654 children treated during
ucts were hybridized in duplicate with clone-specific probes cor- the same period in the Childhood Leukemia Cooperative Group
responding to the patient’s blasts and to the internal standard. centers that did not participate in the study of residual disease
The ratio of the radioactivity of the two probes was calculated. A (Table 1).
calibration curve was drawn from the results obtained with the
serial dilutions. In samples obtained during remission, the num- Statistical Analysis
ber of blasts per 100,000 mononuclear marrow cells was derived
from the calibration curve. Replicate assays gave results with a The principal end point used to determine the prognostic value
standard deviation of 15 to 30 percent of the mean value. When of the presence or absence of residual disease was the relapse-free
two different markers (e.g., one TCRd V2–D3 rearrangement interval, which was calculated as the interval from the time of a
and one TCRg V9–J1 rearrangement) were analyzed to quanti- given assessment of residual disease until the date of the first re-
tate residual leukemic cells in the same sample, the results were lapse. Actuarial curves were computed according to the Kaplan–
closely correlated (correlation coefficient for 28 samples, 0.94). Meier method.16 The prognostic value of the variables studied
was assessed with the use of the log-rank test,17 or the log-rank
Study Design test for linear trend in the case of ordered categorical variables.
The relative risk represented the ratio of the daily risk of relapse
The 11 centers participating in the study enrolled all their pa- in patients with residual disease to the risk in patients without re-
tients at the time of diagnosis, after obtaining informed consent. sidual disease or the ratio of the daily risk of relapse in those with
592 · Augus t 2 7 , 19 9 8
The New England Journal of Medicine
Downloaded from nejm.org on September 28, 2024. For personal use only.
No other uses without permission. Copyright © 1998 Massachusetts Medical Society. All rights reserved.
C L I N I C A L SIGNIF ICANCE OF MINIMAL RE SID UA L D ISEASE IN C H ILD H OOD AC UTE LY MPH OBL ASTIC LEUK EM IA
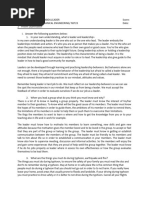
TABLE 1. PROGNOSTIC FACTORS AND OUTCOMES IN THE STUDY GROUP
AND AMONG PATIENTS AT OTHER CENTERS.*
VARIABLE STUDY GROUP PATIENTS AT OTHER CENTERS
NO. OF RELATIVE P NO. OF RELATIVE P
PATIENTS (%) RISK† VALUE‡ PATIENTS (%) RISK† VALUE‡
Total 178 (100) 654 (100)
Age (yr) 0.10 <0.001
0–1 10 (6) 1.7 70 (11) 2.4
2–9 145 (81) 1.0 470 (72) 1.0
10–15 23 (13) 2.2 114 (17) 2.3
Risk group 0.07 <0.001
Standard risk 162 (91) 1.0 563 (86) 1.0
Very high risk 16 (9)§ 2.2 91 (14) 2.9
Immunophenotype 0.01 0.50
B-lineage 149 (84) 1.0 565 (86) 1.0
T-lineage 29 (16) 2.4 89 (14) 1.2¶
White-cell count 0.05 <0.001
<10,000/mm3 76 (43) 1.0 310 (47) 1.0
10,000–99,000/mm3 81 (46) 1.4 261 (40) 2.0
»100,000/mm3 21 (12) 2.6 83 (13) 4.7
Karyotype 0.08 0.40
Normal 55 (31) 3.0 155 (24) 1.9
Hyperdiploidy (>50 33 (19) 1.0 49 (7) 1.0
chromosomes)
Other 50 (28) 1.8 284 (43) 1.8
Not available 40 (22) — 166 (25) —
Outcome¿
Continuous remission 140 (79) 531 (81)
Marrow relapse 22 (12) 63 (10)
Extramedullary relapse 9 (5) 20 (3)
Combined relapse 7 (4) 25 (4)
Death during remission 0 (0) 15 (2)
*Percentages may not sum to 100 because of rounding. The patients at other centers were treated
with the same chemotherapeutic regimen as the study group, but these centers did not participate in
the analysis of residual disease.
†The relative risk was estimated by calculating the ratio of observed to expected relapses.
‡P values were determined by the log-rank test. Because of the small number of relapses in the
study group (38), the P value did not reach statistical significance for several comparisons.
§Fifteen of the patients had poor responses to the corticosteroid therapy, and one had the t(9;22)
translocation.
¶The prognosis was slightly worse for the T-lineage group, particularly because of their higher re-
lapse rate during therapy.
¿The instantaneous risk of relapse was similar in the two groups of patients (relative risk in the
study group as compared with the patients at other centers, 1.19). For the analysis of outcomes, data
for patients who died while in remission were censored at the time of death.
a high level of residual disease to the risk in those with a low level. for residual disease. These 178 patients were similar
This was estimated by calculating the ratio of observed to expect- to the 654 patients in the nonparticipating centers
ed relapses18 with the use of log-rank computations.
The prognostic significance of other variables measured at the with regard to the time to relapse and the distribu-
time of diagnosis was determined in the same way. Subgroups of tion of prognostic factors (Table 1). The effects of
patients were defined according to classic prognostic factors (Ta- prognostic factors were also similar in the two groups,
ble 1). The stratified log-rank test was used to determine the except for immunophenotype. The duration of re-
prognostic value of residual disease as compared with other prog-
nostic factors, and the corresponding stratified relative risks were
mission in the group of 68 patients who were en-
computed. Cytogenetic characteristics were not included in the rolled at the time of diagnosis but were subsequently
stratified analyses because of the high percentage of patients in excluded from the study was similar to that in the
whom they could not be evaluated (22 percent). The Cox regres- 178 patients who remained in the study. The medi-
sion model19 was used to determine the most significant inde- an follow-up period was 38 months.
pendent prognostic factors. The stratified Cox regression model19
was used to determine the prognostic value of residual disease as Residual Disease during the First Six Months of Remission
compared with that of immunophenotype. This method provided
an estimate of the relative risk and 95 percent confidence interval. After the completion of induction therapy, 42
percent of the patients had residual leukemia (Table
RESULTS 2). Residual blasts were detected in 38 percent of
Of the 246 patients enrolled in the study at the the standard-risk group and 66 percent of the very-
time of diagnosis, 178 (72 percent) were monitored high-risk group; they were detected in 36 percent of
Vol ume 33 9 Numb e r 9 · 593
The New England Journal of Medicine
Downloaded from nejm.org on September 28, 2024. For personal use only.
No other uses without permission. Copyright © 1998 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
residual disease increased during the first 6 months
TABLE 2. RISK OF RELAPSE ACCORDING TO THE PRESENCE had a relapse 1 to 15 months later.
OR ABSENCE AND LEVEL OF RESIDUAL DISEASE AT DIFFERENT
TIMES AFTER INDUCTION OF REMISSION. Predictive Value of Residual Disease
at the End of Induction Therapy
NO. OF PATIENTS/ NO. WITH RELATIVE The patients with detectable residual disease at the
RESIDUAL DISEASE* TOTAL NO. (%)† RELAPSES RISK‡
end of induction therapy, including those with a
After induction therapy standard risk of relapse and those with a very high
Absent 88/151 (58) 7 1.0 risk, had a significantly shorter time to relapse
Present 63/151 (42) 25 5.7
Residual blasts than the patients with undetectable residual disease
<10¡3 109/133 (82) 10 1.0 (P<0.001 by the log-rank test), and the instanta-
10¡3 to <10¡2 9/133 (7) 2 2.3
»10¡2 15/133 (11) 11 16.0§
neous risk of relapse was 5.7 times as high in the pa-
After consolidation therapy tients with residual disease as in those without resid-
Absent 95/127 (75) 8 1.0 ual disease (Fig. 1 and Table 2). To determine whether
Present 32/127 (25) 15 7.3
Residual blasts the level of residual disease could be used to predict
<10¡3 110/118 (93) 11 1.0 relapse, we assigned the patients to one of three sub-
»10¡3 8/118 (7) 6 15.3 groups according to the concentration of residual
After interval therapy
Absent 108/130 (83) 11 1.0 leukemic cells in marrow samples: less than 10¡3,
Present 22/130 (17) 11 7.3 10¡3 or more but less than 10¡2, and 10¡2 or more.
Residual blasts
<10¡3 118/127 (93) 13 1.0
The probability of relapse increased with the level of
»10¡3 9/127 (7) 7 18.5 residual disease. Patients with 10¡2 or more residual
After delayed intensification blasts had a shorter time to relapse than those with
therapy
Absent 107/123 (87) 14 1.0 lower levels of blasts (P<0.001 by the log-rank test)
Present 16/123 (13) 10 9.2 (Fig. 1), and the relative risk of relapse was 16 times
Residual blasts as high in the patients with 10¡2 or more blasts as in
<10¡3 114/119 (96) 17 1.0
»10¡3 5/119 (4) 5 22.0 those with less than 10¡3 blasts.
The duration of survival was also related to the
*The number of residual blasts is expressed as the ratio of residual blasts presence or absence and level of residual disease. Pa-
to 2¬105 mononuclear bone marrow cells.
†The numbers of patients studied were different at different points in
tients with residual disease had a risk of death that
time for two reasons: samples were not obtained from all patients at each was 10 times that in patients without detectable re-
time point, and at the end of induction therapy, the study group consisted sidual disease. The quantitative analysis was even
of patients at standard risk and those at very high risk, whereas the study
group consisted only of patients at standard risk at the other time points.
more predictive: the risk of death was 24 times as
‡The relative risk was estimated by calculating the ratio of observed to
high for patients with 10¡2 or more residual leuke-
expected relapses. For all comparisons, P<0.001 by the log-rank test. mic cells as for patients with lower levels of residual
§The relative risk was 14.2 for patients who had »10¡2 residual blasts disease (data not shown).
as compared with those who had <10¡2 residual blasts.
Predictive Value of Residual Disease at Later Times
At three different time points, the time to relapse
the group with B-lineage ALL and 90 percent of the in the standard-risk group was significantly shorter
group with T-lineage ALL. In the standard-risk for patients with detectable residual disease than for
group, 25 percent of the patients had detectable re- those without detectable residual disease (P<0.001
sidual disease after consolidation therapy, 17 percent by the log-rank test) (Fig. 2). The risk of relapse was
after interval therapy, and 13 percent after delayed significantly higher in patients with detectable dis-
intensification therapy. ease than in those with undetectable disease (7.3
Table 3 shows the predictive value of a change in times as high after consolidation and interval thera-
status with respect to detectable residual disease at py and 9.2 times as high after delayed intensification
two different points in time. The relative risk of re- therapy) (Table 2). Quantitative assessment of resid-
lapse was 4.9 for the patients who had residual dis- ual leukemia allowed further discrimination: a value
ease initially but did not have residual disease after at or above a threshold of 10¡3 residual leukemic
consolidation therapy and 15.0 for the patients with cells was highly predictive of relapse at all three time
persistent residual disease after consolidation thera- points (P<0.001 by the log-rank test) (Fig. 2). The
py, as compared with the patients in whom residual risk of relapse increased by a factor of 15.3 to 22.0
disease was undetectable after both induction and in patients with 10¡3 or more residual blasts (repre-
consolidation therapy. The results were similar at senting 4 to 7 percent of the patients), as compared
subsequent time points. During the first six months with those with fewer than 10¡3 residual blasts (Ta-
after induction therapy, no patient who initially had ble 2). The risk of death was increased by a factor of
no detectable disease subsequently had detectable approximately 25 in patients with 10¡3 or more re-
disease. However, six patients in whom the level of sidual blasts at each time point (data not shown).
594 · Augus t 2 7 , 19 9 8
The New England Journal of Medicine
Downloaded from nejm.org on September 28, 2024. For personal use only.
No other uses without permission. Copyright © 1998 Massachusetts Medical Society. All rights reserved.
C L I N I C A L SIGNIF ICANCE OF MINIMAL RE SID UA L D ISEASE IN C H ILD H OOD AC UTE LY MPH OBL ASTIC LEUK EM IA
TABLE 3. RELATIVE RISK OF RELAPSE ACCORDING TO THE PRESENCE OR ABSENCE OF RESIDUAL DISEASE
AT TWO TIME POINTS.
AFTER INDUCTION THERAPY, AFTER INDUCTION THERAPY, AFTER CONSOLIDATION THERAPY,
RESIDUAL DISEASE* AFTER CONSOLIDATION THERAPY AFTER INTERVAL THERAPY AFTER INTERVAL THERAPY
NO. OF NO. WITH RELATIVE NO. OF NO. WITH RELATIVE NO. OF NO. WITH RELATIVE
PATIENTS RELAPSES RISK† PATIENTS RELAPSES RISK† PATIENTS RELAPSES RISK†
Absent, absent 73 3 1.0 78 4 1.0 91 7 1.0
Present, absent 15 3 4.9 23 5 4.1 8 2 3.0
Present, present 32 15 15.0 22 11 14.0 22 11 9.6
*During the first six months, residual disease was not detected in any of the patients who did not previously have de-
tectable residual disease.
†The relative risk was estimated by calculating the ratio of observed to expected relapses. For all comparisons, P<0.001
by the log-rank test for linear trend.
100 No residual disease
90
Patients withoutL
80 <10¡2 Residual blasts
Relapses (%)
70
60 Residual disease
50
40
30 »10¡2 Residual blasts
20
10
0
0 1 2 3 4 5 6 7
Year
NO. OF RELAPSESL NO. OF PATIENTS AT RISKL
No residual diseaseL L 7L L88L 86L 74L 44L 18L 1L 1L
Residual diseaseL 25L 63L 53L 42L 25L 10L 4L 1L
<10¡2 Residual blastsL 12L 118L 115L 98L 58L 25L 2L 1L
»10¡2 Residual blastsL 11L 15L 7L 4L 3L 0L 0L 0L
Figure 1. Kaplan–Meier Estimates of the Relapse-free Interval According to the Presence or Absence
and Level of Residual Disease in Patients with a First Complete Remission of ALL at the End of Induc-
tion Therapy.
P<0.001 for the comparison between patients with residual disease and those without residual disease
and for the comparison between patients with »10¡2 residual blasts and those with <10¡2 residual
blasts. Nine of the 15 patients with a high level of residual disease (»10¡2 blasts) died, as compared
with only 4 of the 118 with a lower level of residual disease (<10¡2 blasts). The numbers of patients
shown below the graph are the numbers at standard or very high risk for whom bone marrow samples
were available. In 18 patients, residual disease was detected but was not quantitated.
In the very-high-risk group, patients without de- were associated with the poorest outcome, with a
tectable residual disease after intensified consolida- relative risk of relapse ranging from 2.18 to 2.58
tion therapy had a lower probability of relapse than (Table 1). Bivariate analyses showed that the pres-
those with detectable disease (P=0.03 by the log- ence or absence and level of residual disease at dif-
rank test). ferent time points remained significant prognostic
factors after stratification for white-cell count, im-
Predictive Value of Residual Disease after Stratification munophenotype, risk group, and age (Table 4). With
for Other Factors
the use of the stratified log-rank method, the esti-
The T-lineage immunophenotype, a white-cell mated relative risk of relapse was about 5 for the pa-
count of 100,000 per cubic millimeter or higher, an tients with residual disease and more than 5 for
age of 10 to 15 years, and assignment to the very- those with 10¡2 or more residual blasts after induc-
high-risk group (which accounted for 9 to 16 per- tion and 10¡3 or more subsequently (Table 4).
cent of the patients monitored for residual disease) In a Cox model, residual disease remained the
Vol ume 33 9 Numb e r 9 · 595
The New England Journal of Medicine
Downloaded from nejm.org on September 28, 2024. For personal use only.
No other uses without permission. Copyright © 1998 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
100 No residual disease
90
Patients withoutL
80 <10¡3 Residual blasts
Relapses (%)
70
60
Residual disease
50
40
30
20 »10¡3 Residual blasts
10
0
0 1 2 3 4 5 6 7
Year
NO. OF RELAPSESL NO. OF PATIENTS AT RISKL
No residual diseaseL L 8L L95L 92L 76L 46L 20L 3L 2L
Residual diseaseL 15L 32L 23L 17L 10L 3L 3L 1L
<10¡3 Residual blastsL 11L 110L 106L 88L 54L 21L 4L 2L
»10¡3 Residual blastsL 6 8L 3L 1 1L 1 1L 0L
100
No residual disease
90
Patients withoutL
80
<10¡3 Residual blasts
Relapses (%)
70
60
50 Residual disease
40
30
20 »10¡3 Residual blasts
10
0
0 1 2 3 4 5 6 7
Year
NO. OF RELAPSESL NO. OF PATIENTS AT RISKL
No residual diseaseL L 11L L
108L 101L 85L 48L 14L 2L 2L
Residual diseaseL 11L 22L 12L 8L 5L 3L 2L 1L
<10¡3 Residual blastsL 13L 118L 111L 91L 52L 16L 3L 3L
»10¡3 Residual blastsL 7 9L 1L 1 1L 1 1L 0L
100
90 No residual disease
Patients withoutL
80
Relapses (%)
70 <10¡3 Residual blasts
60
50
40 Residual disease
30
20
10 »10¡3 Residual blasts
0
0 1 2 3 4 5 6 7
Year
NO. OF RELAPSESL NO. OF PATIENTS AT RISKL
No residual diseaseL L 14L L
107L 97L 76L 37L 16L 3L 0L
Residual diseaseL 10L 16L 7L 3L 2L 1L 1L 1L
<10¡3 Residual blastsL 17L 114L 101L 78L 39L 17L 4L 1L
»10¡3 Residual blastsL 5 5L 1L 0 0L 0 0L 0L
596 · Augus t 2 7 , 19 9 8
The New England Journal of Medicine
Downloaded from nejm.org on September 28, 2024. For personal use only.
No other uses without permission. Copyright © 1998 Massachusetts Medical Society. All rights reserved.
C L I N I C A L SIGNIF ICANCE OF MINIMAL RE SID UA L D ISEASE IN C H ILD H OOD AC UTE LY MPH OBL ASTIC LEUK EM IA
TABLE 4. RELATIVE RISK OF RELAPSE ACCORDING TO THE PRESENCE OR ABSENCE
AND LEVEL OF RESIDUAL DISEASE AND OTHER PROGNOSTIC FACTORS.*
IMMUNO-
RISK WHITE-CELL IMMUNO- PHENOTYPE
RESIDUAL DISEASE† GROUP AGE COUNT PHENOTYPE (COX MODEL)
relative risk‡
After induction therapy
Present versus absent 5.2 5.2 4.8 4.3 5.3 (2.2–12.6)
»10¡2 versus <10¡2 residual blasts 12.8 10.7 8.1 5.7 10.6 (3.9–28.7)
After consolidation therapy
Present versus absent — 6.5 6.2 5.3 6.1 (2.5–14.9)
»10¡3 versus <10¡3 residual blasts — 14.4 5.6 7.8 11.2 (3.6–34.7)
After interval therapy
Present versus absent — 6.5 5.3 5.4 6.5 (2.7–15.6)
»10¡3 versus <10¡3 residual blasts — 12.5 6.1 9.2 —§
After delayed intensification therapy
Present versus absent — 7.8 5.5 5.2 7.9 (3.1–19.8)
»10¡3 versus <10¡3 residual blasts — 22.3 5.1 6.0 14.7 (3.2–64.7)
*The cutoff points for categorical variables were identical to those in Table 1 except for age (2 to
9 years vs. others); upper and lower age groups (<2 years and »10 years) were pooled to obtain a
larger group with a poor prognosis. Analysis according to risk group (standard or very high risk) was
carried out for all patients at the end of induction therapy. For later time points, stratified and re-
gression analyses were performed only for patients at standard risk.
†The number of residual blasts is expressed as the ratio of residual blasts to 2¬10 5 mononuclear
bone marrow cells.
‡For all four prognostic factors, the relative risk was estimated by calculating the ratio of observed
to expected differences. For immunophenotype, the relative risk was also estimated with the stratified
Cox model, as shown in the right-hand column, with 95 percent confidence intervals in parentheses.
§The relative risk was not estimated because of problems with the convergence of values.
most important prognostic factor, followed by either ed relapses, indicating that the two methods give
immunophenotype or white-cell count (data not consistent results (Table 4). The lower limits of these
shown). Since the immunophenotype was a signifi- confidence intervals were markedly higher than 1,
cant prognostic factor and was closely correlated confirming that the presence or absence and level of
with the level of residual disease after induction residual disease were important independent prog-
therapy, the Cox model was stratified according to nostic factors.
immunophenotype to assess the relative prognostic
importance of the subsequent evaluations of residual DISCUSSION
disease (Table 4). The relative risks calculated with We found that the use of PCR to detect small
this model were higher than those based on the ratio numbers of leukemic cells remaining in the bone
of observed to expected relapses. However, the 95 marrow after the induction of a remission by chemo-
percent confidence intervals for the Cox-model rel- therapy can predict relapse. Since the clinical out-
ative risks spanned the ratios of observed to expect- come was similar in the 178 patients who were ana-
lyzed for residual disease and the 654 patients
registered in the same trial but not enrolled in the
Figure 2. Kaplan–Meier Estimates of the Relapse-free Interval
study of residual disease, we believe that our conclu-
in Patients with ALL at Standard Risk, According to the Pres- sions have general applicability to patients with ALL.
ence or Absence and Level of Residual Disease after Consoli- Residual disease was detected in about 40 percent
dation Therapy (Top Panel), Interval Therapy (Middle Panel), of patients after the completion of induction thera-
and Delayed Intensification Therapy (Bottom Panel).
py. After consolidation and interval treatment, the
P<0.001 for the comparison between patients with residual
disease and those without residual disease and for the com-
proportion of patients with detectable residual dis-
parison between patients with »10¡3 residual blasts and those ease decreased. Delayed intensification therapy had a
with <10¡3 residual blasts. The majority of patients with »10¡3 limited effect on eliminating residual disease, per-
blasts died: four of eight after consolidation therapy, six of nine haps because of resistance to chemotherapy. Our re-
after interval therapy, and five of five after delayed intensifica- sults differ from those of studies showing that leuke-
tion therapy. For each point in time, the numbers of patients
shown below the graph are the numbers at standard risk for
mic cells persist in most patients during the first six
whom bone marrow samples were available. In 18 patients, re- months of treatment.4,7,9,10,20 However, there are dif-
sidual disease was detected but was not quantitated. ferences in the sensitivity of detection methods. For
Vol ume 33 9 Numb e r 9 · 597
The New England Journal of Medicine
Downloaded from nejm.org on September 28, 2024. For personal use only.
No other uses without permission. Copyright © 1998 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
example, in the study by Roberts et al.,20 a detection The views expressed in this article are solely those of the authors and do
not represent the official views of the National Cancer Institute.
level of about 5¬10¡6 was achieved by testing a large
number of cells,21 thus resulting in a longer period REFERENCES
during which residual leukemia could be detected.
1. d’Auriol L, Macintyre E, Galibert F, Sigaux F. In vitro amplification of
Our study also differs from the work of Roberts et T cell g gene rearrangements: a new tool for the assessment of minimal
al. with regard to the statistical methods used and residual disease in acute lymphoblastic leukemias. Leukemia 1989;3:155-8.
the characteristics of the patients. Their small sample 2. Macintyre EA, d’Auriol L, Duparc N, Leverger G, Galibert F, Sigaux F.
Use of oligonucleotide probes directed against T cell antigen receptor gam-
(25 patients) may not be representative; none of ma delta variable-(diversity)-joining junctional sequences as a general
their patients, for example, had an early relapse. In method for detecting minimal residual disease in acute lymphoblastic leu-
kemias. J Clin Invest 1990;86:2125-35.
our view, the numbers of measurements made in the 3. Hansen-Hagge T, Yokota S, Bartram CR. Detection of minimal residual
early stages of remission in the study by Roberts et disease in acute lymphoblastic leukemia by in vitro amplification of rear-
al.20 were too small for an accurate assessment of the ranged T-cell receptor d chain sequences. Blood 1989;74:1762-7.
4. Yamada M, Wasserman R, Lange B, Reichard BA, Womer RB, Rovera
predictive value of the level of residual disease. G. Minimal residual disease in childhood B-lineage lymphoblastic leuke-
In our study, the risk of relapse was markedly in- mia: persistence of leukemic cells during the first 18 months of treatment.
creased in patients with 10¡2 or more residual leuke- N Engl J Med 1990;323:448-55.
5. Campana D, Pui CH. Detection of minimal residual disease in acute
mic cells at the end of induction therapy. This cutoff leukemia: methodologic advances and clinical significance. Blood 1995;85:
value was below the limit of detection with conven- 1416-34.
6. Wasserman R, Galili N, Ito Y, et al. Residual disease at the end of in-
tional microscopical examination of bone marrow by duction therapy as a predictor of relapse during therapy in childhood
two experienced cytologists. For the additional three B-lineage acute lymphoblastic leukemia. J Clin Oncol 1992;10:1879-88.
time points, a value at or above a cutoff of 10¡3 leu- 7. Potter MN, Steward CG, Oakhill A. The significance of detection of
minimal residual disease in childhood acute lymphoblastic leukaemia. Br J
kemic blasts was highly predictive of relapse. Haematol 1993;83:412-8.
The presence or absence and level of residual leuke- 8. Brisco MJ, Condon J, Hughes E, et al. Outcome prediction in child-
mic cells were predictive of survival at all four time hood acute lymphoblastic leukaemia by molecular quantification of residual
disease at the end of induction. Lancet 1994;343:196-200.
points. Our results show that residual leukemia is es- 9. Yokota S, Hansen-Hagge TE, Ludwig WD, et al. Use of polymerase
pecially predictive of relapses during therapy. Under chain reactions to monitor minimal residual disease in acute lymphoblastic
leukemia patients. Blood 1991;77:331-9.
these circumstances, the prognosis is particularly poor. 10. Nizet Y, Van Daele S, Lewalle P, et al. Long-term follow-up of residual
Stratified and multivariate analyses showed that disease in acute lymphoblastic leukemia patients in complete remission us-
the presence or absence and level of residual disease ing clonogeneic IgH probes and the polymerase chain reaction. Blood
1993;82:1618-25.
remained significant prognostic factors even when 11. Cavé H, Guidal C, Rohrlich P, et al. Prospective monitoring and quan-
other known prognostic factors, such as immuno- titation of residual blasts in childhood acute lymphoblastic leukemia by
phenotype, white-cell count, age, and risk group, polymerase chain reaction study of d and g T-cell receptor genes. Blood
1994;83:1892-902.
were taken into consideration. However, the occur- 12. Reiter A, Schrappe M, Ludwig W-D, et al. Chemotherapy in 998 un-
rence of individual relapses was not always predicted. selected childhood acute lymphoblastic leukemia patients: results and con-
clusions of the multicenter trial ALL-BFM 86. Blood 1994;84:3122-33.
The failure to predict relapses in patients without 13. Henze G, Buchmann S, Fengler R, Hartmann R. The BFM relapse
detectable residual disease was probably not due to studies in childhood ALL: concepts of two multicenter trials and results
inadequate sensitivity of the PCR assay (median level after 21/2 years. Haematol Blood Transfus 1987;30:147-55.
14. Breit T, Wolvers-Tettero LI, Hählen K, van Wering ER, van Dongen
of detection, 5¬10¡5), since the relapse rate was JJ. Limited combinatorial repertoire of gdT-cell receptors expressed by
similar in the group of patients with a level of resid- T-cell acute lymphoblastic leukemias. Leukemia 1991;5:116-24.
ual disease below 10¡3 and in those without detect- 15. Trainor KJ, Brisco MJ, Wan JH, Neoh S, Grist S, Morley AA. Gene
rearrangement in B- and T-lymphoproliferative disease detected by the pol-
able disease. It is likely that these relapses resulted ymerase chain reaction. Blood 1991;78:192-6.
from the emergence of a malignant subclone with 16. Peto J. The calculation and interpretation of survival curves. In: Buyse
ME, Staquet MJ, Sylvester RJ, eds. Cancer clinical trials: methods and prac-
resistance to chemotherapy. tice. Oxford, England: Oxford University Press, 1984:361-80.
If the detection of residual leukemia is to be used 17. Breslow N. Comparison of survival curves. In: Buyse ME, Staquet MJ,
in clinical practice to identify patients with a high Sylvester RJ, eds. Cancer clinical trials: methods and practice. Oxford, Eng-
land: Oxford University Press, 1984:381-406.
probability of early relapse, two conditions must be 18. Peto R, Pike MC, Armitage P, et al. Design and analysis of random-
met: the analysis should be performed as early as pos- ized clinical trials requiring prolonged observation of each patient. II.
sible, and the laboratory technique should be simple Analysis and examples. Br J Cancer 1977;35:1-39.
19. Cox DR. Regression models and life-tables. J R Soc Stat [B] 1972;34:
and rapid so that treatment can be tailored to the 187-220.
adjusted assessment of risk. In this respect, the thresh- 20. Roberts WM, Estrov Z, Ouspenskaia MV, Johnston DA, McClain KL,
Zipf TF. Measurement of residual leukemia during remission in childhood
olds that we found predicted relapse can now be acute lymphoblastic leukemia. N Engl J Med 1997;336:317-23.
reached with simpler and more rapid techniques, 21. Ouspenskaia MV, Johnston DA, Roberts WM, Estrov Z, Zipf TF. Ac-
such as use of the leukemia-associated immunophe- curate quantitation of residual B-precursor acute lymphoblastic leukemia
by limiting dilution and a PCR-based detection system: a description of
notype to detect residual cells 22 or fluorescence– the method and the principles involved. Leukemia 1995;9:321-8.
PCR analysis of gene rearrangements.23 22. Coustan-Smith E, Behm FG, Sanchez J, et al. Immunological detec-
tion of minimal residual disease in children with acute lymphoblastic leu-
kaemia. Lancet 1998;351:550-4.
Supported by grants from the Association pour la Recherche sur le Can- 23. Shiach CR, Evans PA, Short MA, Bailey CC, Lewis IJ, Kinsey SE. De-
cer and the National Cancer Institute (5U10-CA11488-23 through 5U10- tection and accurate sizing of PCR product by automated scanning: im-
CA11488-28). Drs. van der Werff ten Bosch and Bakkus are the recipients proved detection of immunoglobulin gene rearrangements in ALL. Br J
of research awards from the Belgian National Fund for Scientific Research. Haematol 1993;85:431-3.
598 · Augus t 2 7 , 19 9 8
The New England Journal of Medicine
Downloaded from nejm.org on September 28, 2024. For personal use only.
No other uses without permission. Copyright © 1998 Massachusetts Medical Society. All rights reserved.
You might also like
- Approach To Diagnosis of Celiac Disease - UpToDateDocument2 pagesApproach To Diagnosis of Celiac Disease - UpToDatemiguelNo ratings yet
- Speaking Sample Test 3 - Veterinary ScienceDocument1 pageSpeaking Sample Test 3 - Veterinary ScienceMehdi YarmohammadiNo ratings yet
- PIIS014067361261900XDocument10 pagesPIIS014067361261900X呂鍇東No ratings yet
- Obinutuzumab Versus Rituximab Immunochemotherapy in Previously Untreated iNHL: Final Results From The GALLIUM StudyDocument10 pagesObinutuzumab Versus Rituximab Immunochemotherapy in Previously Untreated iNHL: Final Results From The GALLIUM StudyBreno SouzaNo ratings yet
- Dexametasona en Meningitis TBCDocument11 pagesDexametasona en Meningitis TBCVerónica NaniNo ratings yet
- Aparicio 2011Document5 pagesAparicio 2011Bruno AlanNo ratings yet
- 9Document13 pages9Osama BakheetNo ratings yet
- Choueiri 2021Document13 pagesChoueiri 2021Dálete BarcelosNo ratings yet
- Blood Culture-Negative EndocarditisDocument7 pagesBlood Culture-Negative EndocarditisIkhsan Amadea9969No ratings yet
- 10.1016@S1473 30992030796 9Document15 pages10.1016@S1473 30992030796 9lamnguyendzvcl123No ratings yet
- Ournal of Linical Ncology: PurposeDocument7 pagesOurnal of Linical Ncology: PurposeFadhillah ArafahNo ratings yet
- Pi Is 1201971213002142Document5 pagesPi Is 1201971213002142melisaberlianNo ratings yet
- Early Use of TIPS in Cirrhosis and Variceal BleedingDocument10 pagesEarly Use of TIPS in Cirrhosis and Variceal Bleedingray liNo ratings yet
- Haematopoietic-stem-cell-transplantation-in-Crohn'Document2 pagesHaematopoietic-stem-cell-transplantation-in-Crohn'pp2jpfyvq6No ratings yet
- Portec 2.Document8 pagesPortec 2.henryNo ratings yet
- Marneffei: Cytological Diagnosis of Penicillium InfectionDocument5 pagesMarneffei: Cytological Diagnosis of Penicillium InfectionAnonymous oQtve4oNo ratings yet
- VasculitisDocument12 pagesVasculitisMaite OrellanaNo ratings yet
- 2 - Adult Meningitis in A Setting of High HIV and TB Prevalence - Findings From 4961 Suspected Cases 2010 (Modelo para o Trabalho)Document6 pages2 - Adult Meningitis in A Setting of High HIV and TB Prevalence - Findings From 4961 Suspected Cases 2010 (Modelo para o Trabalho)SERGIO LOBATO FRANÇANo ratings yet
- A Systematic Review of Immunotherapy in Urologic Cancer - Evolving Roles For Targeting of CTLA-4, PD-1 PD-L1, and HLA-G 2Document13 pagesA Systematic Review of Immunotherapy in Urologic Cancer - Evolving Roles For Targeting of CTLA-4, PD-1 PD-L1, and HLA-G 2Lydia Angelia YanitaNo ratings yet
- UntitledDocument26 pagesUntitledAounAbdellahNo ratings yet
- Appropriate Antibiotics For Peritonsillar Abscess - A 9 Month CohortDocument5 pagesAppropriate Antibiotics For Peritonsillar Abscess - A 9 Month CohortSiti Annisa NurfathiaNo ratings yet
- Yao 2011Document10 pagesYao 2011Jemma ArakelyanNo ratings yet
- Cancer - 2004 - Li - Treatment Outcome and Pattern of Failure in 77 Patients With Sinonasal Natural Killer T Cell or T CellDocument10 pagesCancer - 2004 - Li - Treatment Outcome and Pattern of Failure in 77 Patients With Sinonasal Natural Killer T Cell or T Cell2512505993No ratings yet
- Henriot 2016Document7 pagesHenriot 2016Tzeto Han CongNo ratings yet
- Eortc 22911 PDFDocument10 pagesEortc 22911 PDFAndres Felipe Cordoba AriasNo ratings yet
- PIIS2214109X23001353Document14 pagesPIIS2214109X23001353Joaquin OlivaresNo ratings yet
- Publication OncologyDocument12 pagesPublication Oncologyokoye ucheNo ratings yet
- Vandenbosch 2011Document8 pagesVandenbosch 2011nimaelhajjiNo ratings yet
- Brief Report - Childhood Onset Systemic Necrotizing Vasculitides - Long Term Data From The French Vasculitis Study Group RegistryDocument7 pagesBrief Report - Childhood Onset Systemic Necrotizing Vasculitides - Long Term Data From The French Vasculitis Study Group RegistryMiguel ArmidaNo ratings yet
- Articles: BackgroundDocument10 pagesArticles: BackgroundivanlchNo ratings yet
- Boutolleau 2021Document9 pagesBoutolleau 2021nathalialusman98No ratings yet
- Combes 2007Document9 pagesCombes 2007RaffaharianggaraNo ratings yet
- 1 Weber Et Al Nivo Vs Chemo Checkmate037Document10 pages1 Weber Et Al Nivo Vs Chemo Checkmate037kaeferchen1609No ratings yet
- Antifungal Treatment Duration in Hematology Patients With Invasive Mold Infections A Real-Life UpdateDocument9 pagesAntifungal Treatment Duration in Hematology Patients With Invasive Mold Infections A Real-Life UpdateNelly Mabel Quiroz HernandezNo ratings yet
- Bonney 2015Document9 pagesBonney 2015drkripa100No ratings yet
- Pinda FynDocument7 pagesPinda FynCaballero X CaballeroNo ratings yet
- De-Escalation of Antimicrobial Treatment in Neutropenic Patients With Severe Sepsis: Results From An Observational StudyDocument10 pagesDe-Escalation of Antimicrobial Treatment in Neutropenic Patients With Severe Sepsis: Results From An Observational StudyyostiNo ratings yet
- Rez BFM Rez 2009Document12 pagesRez BFM Rez 2009erickmattosNo ratings yet
- Javali2018 en IdDocument10 pagesJavali2018 en IdDona Ratna SariNo ratings yet
- The Evaluation of Tumor-Infiltrating Lymphocytes (TILs) in Breast Cancer - Recommendations by An International TILs Working Group 2014Document13 pagesThe Evaluation of Tumor-Infiltrating Lymphocytes (TILs) in Breast Cancer - Recommendations by An International TILs Working Group 2014liliaiyutianNo ratings yet
- Nejmoa 2032125Document13 pagesNejmoa 2032125CARLOS DURANNo ratings yet
- Gene Therapy Clinical Trials Worldwide To 2017 An UpdateDocument16 pagesGene Therapy Clinical Trials Worldwide To 2017 An UpdateLeonardo Sandi SalazarNo ratings yet
- Per-Protocol Repeat Kidney Biopsy Portends Relapse and Long-Term Outcome in Incident Cases of Proliferative Lupus NephritisDocument11 pagesPer-Protocol Repeat Kidney Biopsy Portends Relapse and Long-Term Outcome in Incident Cases of Proliferative Lupus Nephritisjose pablo quero reyesNo ratings yet
- Ciaa 1611Document8 pagesCiaa 1611Silvia Rodriguez PitreNo ratings yet
- Effectiveness and Safety of Cefazolin Versus Cloxacillin in Endocarditis Due ToDocument9 pagesEffectiveness and Safety of Cefazolin Versus Cloxacillin in Endocarditis Due Toanna531No ratings yet
- Research Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology FindingsDocument9 pagesResearch Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology Findings28121998No ratings yet
- Ournal of Linical Ncology: PurposeDocument11 pagesOurnal of Linical Ncology: PurposeRicky Cornelius TariganNo ratings yet
- Nebulized Colistin in The Treatment of Pneumonia Due To Multidrug-Resistant Acinetobacter Baumannii and Pseudomonas AeruginosaDocument4 pagesNebulized Colistin in The Treatment of Pneumonia Due To Multidrug-Resistant Acinetobacter Baumannii and Pseudomonas AeruginosaPhan Tấn TàiNo ratings yet
- Liquid Biopsy_ From Concept to Clinical ApplicationDocument5 pagesLiquid Biopsy_ From Concept to Clinical Applicationshreyassuper365No ratings yet
- 149 FullDocument10 pages149 Fullসোমনাথ মহাপাত্রNo ratings yet
- European Respiratory Journal 2014 DenkingerDocument12 pagesEuropean Respiratory Journal 2014 Denkingertammy_tataNo ratings yet
- Robotic Surgery in Pediatric Oncology: Lessons Learned From The First 100 Tumors-A Nationwide ExperienceDocument12 pagesRobotic Surgery in Pediatric Oncology: Lessons Learned From The First 100 Tumors-A Nationwide ExperiencePriyank YadavNo ratings yet
- CANCER UPDATE Clinical Stem Cell Document - Alex Mou & Ryan TangDocument7 pagesCANCER UPDATE Clinical Stem Cell Document - Alex Mou & Ryan Tangalexmou2008No ratings yet
- Pi Is 0022346814003935Document5 pagesPi Is 0022346814003935wibizzzNo ratings yet
- Durable Response After Tisagenlecleucel in Adults With Relapsed:refractory Follicular Lymphoma: ELARA Trial UpdateDocument13 pagesDurable Response After Tisagenlecleucel in Adults With Relapsed:refractory Follicular Lymphoma: ELARA Trial UpdateSoumya PoddarNo ratings yet
- CheckMate 238Document12 pagesCheckMate 238PeyepeyeNo ratings yet
- 33Document11 pages33Joana KellenNo ratings yet
- Jurnal PD 3Document16 pagesJurnal PD 3Suci MayveraNo ratings yet
- Diffuse Malignant Peritoneal Mesothelioma PDFDocument9 pagesDiffuse Malignant Peritoneal Mesothelioma PDFAndreeaPopescuNo ratings yet
- Acute Promyelocytic Leukemia: A Clinical GuideFrom EverandAcute Promyelocytic Leukemia: A Clinical GuideOussama AblaNo ratings yet
- Pediatric Gastroenterology and NutritionDocument206 pagesPediatric Gastroenterology and NutritionArlene BañosNo ratings yet
- Eseu EnglezaDocument2 pagesEseu EnglezaAna MașcauțanNo ratings yet
- Bipolar MseDocument6 pagesBipolar MsesksanisidrogensanNo ratings yet
- Download Full Essentials of Psychiatry in Primary Care: Behavioral Health in the Medical Setting Robert C Smith PDF All ChaptersDocument55 pagesDownload Full Essentials of Psychiatry in Primary Care: Behavioral Health in the Medical Setting Robert C Smith PDF All Chapterskunieliwsi6x100% (4)
- CBG MonitoringDocument15 pagesCBG MonitoringIvette RiveraNo ratings yet
- Pre Conception CareDocument58 pagesPre Conception CareMarkos MakishaNo ratings yet
- Download Cancer Immunotherapy Immune Suppression and Tumor Growth 1st Edition George C. Prendergast ebook All Chapters PDFDocument53 pagesDownload Cancer Immunotherapy Immune Suppression and Tumor Growth 1st Edition George C. Prendergast ebook All Chapters PDFlaudetevcin67100% (3)
- DPLD Shoyabbsmmu 180722070931Document128 pagesDPLD Shoyabbsmmu 180722070931nnn nnnNo ratings yet
- Benefits of Kamias For Human Health - Doctor Farrah MDDocument3 pagesBenefits of Kamias For Human Health - Doctor Farrah MDJosmineNo ratings yet
- NSTP - Dimention of Development Health Awareness - 1.2Document36 pagesNSTP - Dimention of Development Health Awareness - 1.2leslyNo ratings yet
- FOSSENCEDocument15 pagesFOSSENCEocombdNo ratings yet
- Sleeping Disorder ThesisDocument7 pagesSleeping Disorder Thesistsivhqvcf100% (2)
- Encyclopedia of Medical Astrology - L. Cornell-3Document250 pagesEncyclopedia of Medical Astrology - L. Cornell-3dquintero10000No ratings yet
- Shapiro 1997Document6 pagesShapiro 1997JohnnyNo ratings yet
- Malignant External Otitis in Diabetic Patient. Endocrinology & Metabolism International JournalDocument3 pagesMalignant External Otitis in Diabetic Patient. Endocrinology & Metabolism International JournalAtrik Pristica100% (1)
- MCQs Parasitology (1-10) With Answers - Microbe OnlineDocument1 pageMCQs Parasitology (1-10) With Answers - Microbe OnlineHabtamu tamiruNo ratings yet
- Cáncer:overviewDocument10 pagesCáncer:overviewkashirokoshiroNo ratings yet
- Corona - Covid-19Document8 pagesCorona - Covid-19The Good DoctorNo ratings yet
- Introduction To Epidemiology-3Document24 pagesIntroduction To Epidemiology-3Me TooNo ratings yet
- Hipopresivos y Dolor Lumbar Cronico 2021Document9 pagesHipopresivos y Dolor Lumbar Cronico 2021klgarivasNo ratings yet
- DiphtheriaDocument25 pagesDiphtheriaRohan TejaNo ratings yet
- Drug Abuse and Drug AddictionDocument19 pagesDrug Abuse and Drug Addictiononunknown07No ratings yet
- Gul Et Al (2017) - Body-Image-Self-Esteem-And-Quality-Of-Life-In-Vitiligo-PatientsDocument6 pagesGul Et Al (2017) - Body-Image-Self-Esteem-And-Quality-Of-Life-In-Vitiligo-PatientsCarlos RodriguezNo ratings yet
- UntitledDocument40 pagesUntitledCrescia Jane TerazaNo ratings yet
- G12 English Paper 2 2014 Marking SchemeDocument5 pagesG12 English Paper 2 2014 Marking SchemeYellowed McLekaniNo ratings yet
- West Midlands Acute Oncology, Directory of Services.: MSCC, AO and CUP Expert Advisory GroupDocument17 pagesWest Midlands Acute Oncology, Directory of Services.: MSCC, AO and CUP Expert Advisory GroupfidhaNo ratings yet
- Jan 24Document4 pagesJan 24Abdurrafie H. AbdulcaderNo ratings yet
- AntibioticsDocument21 pagesAntibioticsJerry ArockeNo ratings yet