Drug Study
Drug Study
Uploaded by
Vicenia BalloganCopyright:
Available Formats
Drug Study
Drug Study
Uploaded by
Vicenia BalloganCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Drug Study
Drug Study
Uploaded by
Vicenia BalloganCopyright:
Available Formats
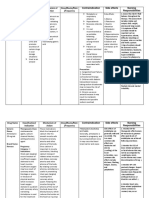
DRUG STUDY 1.
Generic Name:Methylergonovine maleate Brand Name: Methergine
Classification: Oxytocic Therapeutic Actions: A partial agonist or antagonist at alpha receptors; as a result, it increases thestrength, duration, and frequency of uterine contractions. Indications: Routine management after delivery of the placenta. Treatment of postpartum atony and hemorrhage; subinvolution of the uterus. Uterine stimulation during the second stage of labor following the delivery of the anterior shoulder, under strict medical supervision. Contraindications Contraindicated with allergy to methylergonovine, hypertension, toxemia,lactation, pregnancy. Adverse Effects: CNS: Dizziness, headache, tinnitus, diaphoresis CV: Transient hypertension, palpitations, chest pains, dyspnea GI: Nausea and vomiting Nursing Considerations: Assess history of allergy to the drug. Administer by IM injection or orally unless emergency requires IV use.Complications are more frequent with IV use. Monitor postpartum women for BP changes and amount and character of vaginal bleeding. Avoid prolonged use of the drug. Teach client to report difficulty breathing, headache, numb or coldextremities, severe abdominal cramping. 2. Generic Name:Dinoprostone (prostaglandin E2) Brand Name: Classification Therapeutic Actions: Stimulates the myometrium of the pregnant uterus to contract; similar to thecontractions of the uterus during labor, thus evacuating the contents of theuterus. Indications: Termination of pregnancy 12-20 wks from the first day of the LMP. Evacuation of the uterus in the management of missed abortion orintrauterine fetal death up to 28 wk gestational stage Initiation of cervical ripening before induction of labor Contraindications: Contraindicated with allergy to prostaglandins; acute PID; active cardiachepatic; pulmonary, renal disease; women in whom prolonged uterinecontractions are inappropriate. Cervidil :Prostaglandin; abortifacient
Adverse Effects: CNS: Headache, paresthesias, anxiety, weakness, syncope, dizziness CV: Hypotension, arrthymias, chest pain Fetal: Abnormal heart rates GI: vomiting, diarrhea, nauseaRespiratory: Coughing, dyspnea Nursing Considerations: Monitor uterine tone and vaginal discharge throughout the procedureand several days after the procedure. Ensure adequate hydration throughout the procedure. Be prepared to support patient through labor. Give oxytocin infusion 6-12 hr after dinoprostone. Teach client to report severe pain, difficulty breathing, palpitations,eye pain, rash. 3. Generic Name:Oxytocin Brand Name: Pitocin
Classification: Oxytocic; hormone Therapeutic Actions: Synthetic form of an endogenous hormone produced in the hypothalamusand stored in the posterior pituitary; stimulates the uterus, especially thegravid uterus just before parturition, and causes myoepithelium of the lactealglands to contract, which results in milk ejection in lactating women. Indications: Antepartum: to initiate or improve uterine contractions to achieve earlyvaginal delivery; stimulation or reinforcement of labor in selected cases of uterine inertia; management of inevitable or incomplete abortion; 2nd trimester abortion Postpartum: to produce uterine contractions during the third stage of labor tocontrol postpartum bleeding or hemorrhage Lactation defieciency Contraindications: Significant cephalopelvic disproportion, unfavorable fetal positions orpresentations, obstetric emergencies that favor surgical intervention,prolonged use in severe toxemia, uterine inertia, hypertonic uterine patterns,induction or augmentation of labor when vaginal delivery is contraindicated,previous cesarian section. Adverse Effects: CV: cardiac arrhythmias, PVCs, hypertension, subarachnoid hemorrhage Fetal effects: fetal bradycardia, neonatal jaundice, low Apgar scores GI: nauseas, vomiting GU: postpartum hemorrhage, uterine rupture, pelvic hematoma, uterinehypertonicity, spasm Nursing Considerations: Ensure fetal position and size and absence of complications that arecontraindicated with oxytocin therapy Ensure continuous observation for induction of labor; fetal monitoring ispreferred. Regulate rate of oxytocin delivery; monitor rate and strength of contractions Monitor BP during administration
4. Generic Name:Lidocaine hydrochloride Brand Name :Dilocaine
Classification: Local anesthetic Therapeutic Actions: Blocks the generation and conduction of action potentials in sensory nervesby reducing sodium permeability, reducing height and rate of rise of theaction potential, increasing excitation threshold, and slowing conductionvelocity Indications: Infiltration anesthesia, peripheral and sympathetic nerve blocks, centralnerve blocks, spinal and caudal anesthesia Contraindications: Contraindicated with allergy to lidocaine or amide-type local anesthetics, CHFcardiogenic shock, 2nd or 3 rd degree AV blocks Adverse Effects: CNS: headache, backache, septic meningitis, persistent sensory CV: hypotension Dermatologic: urticaria, pruritus, erythema, edema GU: urinary retention, urinary or fecal incontinence Nursing Considerations: Check drug concentrations carefully Establish safety precautions if CNS changes occur Teach client to report difficulty speaking, thick tongue, numbness, tingling,difficulty breathing, pain or numbness at site, swelling or pain at site
5. Generic Name: Terbutaline Sulfate Brand Name: Brethine
Classification: Tocolytic Therapeutic Actions: -In low doses, acts relatively selectively at beta 2-adrenergic receptors tocause bronchodilation and relax the pregnant uterus; at higher doses, beta 1selectivity is lost and the drug acts at beta 2 receptors to cause typicalsympathomimetic cardiac effects Indications: -Tocolytic to prevent preterm labor Contraindications: -Contraindicated with hypersensitivity to terbutaline, tachyarrythmias,tachycardia, hypertension, lactation. Adverse Effects: CNS: restlessness, apprehension, anxiety, fear, CNS stimulation, hyperkinesias,insomnia, tremorsCV: cardiac arrhythmias, palpitations, angina pain, changes in BP and ECG GI: Nausea, vomiting, heartburn, unusual or bad taste
Respiratory: Respiratory difficulties, pulmonary edema, coughing, bronchospasm Nursing Considerations: -Use minimal doses for minimal periods of time; drug tolerance can occur-Maintain a beta-adrenergic blocker on standby in case cardiac arrhythmiasoccur-Teach client to report chest pain, dizziness, insomnia, weakness, tremor 6. Generic Name: Carboprost tromethamine Brand Name: Hemabate
Classification: Prostaglandin; Abortifacient Therapeutic Actions: Stimulates the myometrium of the pregnant uterus to contract; similar to thecontractions of the uterus during labor, thus evacuating the contents of theuterus. Indications: -Termination of pregnancy 13-20 wk from the first day of the LMP -Evacuation of the uterus in instance of missed abortion or intrauterine fetaldeath in the 2nd trimester -Postpartum hemorrhage due to uterine atony unresponsive to conventionalmethods Contraindications: -Contraindicated with allergy to prostaglandin preparations, acute PID; activecardiac,hepatic, pulmonary, renal disease Adverse Effects: CNS: headache, paersthesias, flushing, anxiety, weakness, syncope, dizziness CV: hypotension, arrhythmias, chest pain GI: vomiting, diarrhes, nausea Nursing Considerations: -Assess allergy to the drug -Monitor uterine tone and vaginal discharge during procedure and severaldays after to assess drug effects and recovery -Ensure adequate hydration 7. Generic Name: Nalbuphine hydrochloride Brand Name: Nubain
Classification: Narcotic agonisy-antagonist analgesic Therapeutic Actions: -Nalbuphine acts as an agonist at specific opioid receptors in the Cns toproduce analgesia, sedation but also acts to cause hallucinations and is anantagonist at mu receptors Indications: -Relief of moderate to severe pain-For obstetric analgesia during labor and delivery Contraindications: -Contraindicated with hypersensitivity to nalbuphine, sulfites; lactation Adverse Effects: CNS: sedation, clamminess, sweating, headache, nervousness, restlessness,depression, crying, confusion, faintness, hostility, unusual dreams, hallucinations,euphoria, blurred vision
CV: hypotension, hypertension, bradycardia, tachycardiaDermatologic: itching, burning, urticaria GI: N/V, cramps, dyspepsia, bitter taste, dry mouth GU: Urinary urgencyRespiratory: Respiratory depression, dyspnea, asthma Nursing Considerations: -Assess hypersensitivity to the drug-Provide narcotic antagonist, facilitates for assisted or controlled respirationon standby in case of respiratory depression-Reassure patient about addiction liability; most patients who receive opiatesfor medical reasons do not develop dependence syndrome-Inform clients about these side effects: dizziness, sedation, drowsiness,impaired visual acuity, nausea, loss of appetite
8. Generic Name:Magnesium sulfate Brand Name: Epsom salt
Classification: electrolyte; anticonvulsant; laxarive Therapeutic Actions: -Cofactor of many enzyme systems involved in neuromuscular transmissionand muscular excitability Indications: -Preeclampsia/eclampsia-Inhibition of premature labor Contraindications: -Contraindicated with allergy to magnesium product; heart block, myocardialdamage, abdominal pain, N/V, acute surgical abdomen, fecal impaction,hepatitis. DO NOT GIVE 2 HR PRECEEDING DELIVERY BECAUSE OF RISK OFMAGNESIUM TOXICITY IN THE NEONATE. Adverse Effects: CNS: weakness, dizziness, fainting, sweating CV: palpitations GI: excessive bowel activity, perianal irritation Metabolic: Magnesium intoxication, hypocalcemia with tetany Nursing Considerations: -Assess history of allergy to the drug and other contraindications-Reserve IV use in eclampsia for immediate lifethreatening situations-Monitor magnesium levels during parenteral therapy-Monitor knee-jerk reflex before repeated parenteral administration, if happens, do not administer because respiratory failure may occur -Do not give orally with abdominal pain, N/V-Monitor urine output 9. Generic Name :Butorphanol tartrate Brand Name: stadol
Classification: Narcotic agonist- antagonist analgesic Therapeutic Actions: -Acts as an agonist at opioid receptors in the CNS to produce analgesia,sedation, but also acts to produce hallucinations; has low abuse potential Indications: -Relief of moderate to severe pain-To supplement balances anesthesia and to relieve prepartum pain Contraindications: - Contraindicated with hypersensitivity to butorphanol, physical dependence on anarcotic analgesic, pregnancy lactation
Adverse Effects: CNS: sedation, clamminess, sweating, headache, vertigo, dizziness, lethargy,confusion, unusual dreams, agitation, euphoria, hallucinations CV: Palpitations, increase or decrease in blood pressure Dermatologic: Ras, hives, pruritus, flushing, warmth, sensitivity to cold EENT: diplopia, blurred vision GI: N/VRespiratory: slow, shallow respiration Nursing Considerations: -Assess history of allergy to butorphanol , depression DM, lactation, anddependence-Monitor diet for presence of caffeine- containing foods that may contribute tooverdose-Inform patients that these side effects may occur: diuresis, restlessness,insomnia, muscular tremors, light- headedness, nausea, abdominal pain-Remind patient to report abnormal heart rate, dizziness, palpitations
10.Generic Name: Misoprostol Brand Name: Cytotec
Classification: Prostaglandin Therapeutic Actions: -A synthetic prostaglandin E1 analog; inhibits gastric acid secretion andincreases bicarbonate and mucus production, protecting the lining of thestomach Indications: -With mifepristone as an abortifacient-Cervical ripening and labor induction Contraindications: -History of allergy to prostaglandins; pregnancy; lactation Adverse Effects: GI: nausea, diarrhea, abdominal pain, flatulence, vomiting, dyspepsia, constipation GU: Miscarriage, excessive bleeding, spotting, cramping, menstrual disorders Nursing Considerations: -Assess history of allergy to the drug-Report severe diarrhea, spotting, or menstrual pain, severe menstrualbleeding 11. Generic Name: Midazolam hydrochloride Brand Name: Versed
Classification: Benzodiazepine (short-acting); CNS depressant Therapeutic actions: -Exact mechanisms of action not understood; acts mainly at the limbicsystem and reticular formation; potentiates the effects of GABA, aninhibitory neurotransmitter; anxiolytic and amnesia effects occur atdoses below those needed to cause sedation, ataxia; has little effect oncortical function. Indications -IV or IM: Sedation, anxiolysis, and amnesia prior to diagnostic,therapeutic, or endoscopic procedures or surgery-Induction of general anesthesia -Continuous sedation of intubated and mechanically ventilated patientsas a component of anesthesia or during treatment in the critical caresetting-Unlabeled uses: Treatment of epileptic seizure or refractory statusepilepticus
Contraindications and cautions -Contraindicated with hypersensitivity to benzodiazepines; psychoses,acute narrow-angle glaucoma, shock, coma, acute alcoholicintoxication; pregnancy (cleft lip or palate, inguinal hernia, cardiacdefects, microcephaly, pyloric stenosis have been reported when usedin first trimester; neonatal withdrawal syndrome reported in infants);neonates.-Use cautiously in elderly or debilitated patients; with impaired liver orkidney function, lactation. Adverse effects CNS: Transient, mild drowsiness (initially); sedation, depression, lethargy,apathy, fatigue, light-headedness, disorientation, restlessness, confusion,crying, delirium, headache, slurred speech, dysarthria, stupor, rigidity,tremor, dystonia, vertigo, euphoria, nervousness, difficulty in concentration,vivid dreams, psychomotor retardation, extrapyramidal symptoms; mildparadoxical excitatory reactions (during first 2 wk of treatment), visual andauditory disturbances, diplopia, nystagmus, depressed hearing, nasalcongestion CV: Bradycardia, tachycardia, CV collapse, hypertension, hypotension,palpitations, edemaDermatologic: Urticaria, pruritus, skin rash, dermatitis GI: Constipation, diarrhea, dry mouth, salivation, nausea, anorexia, vomiting,difficulty in swallowing, gastric disorders, elevations of blood enzymes: LDH,alkaline phosphatase, AST, ALT, hepatic dysfunction, jaundiceGU: Incontinence, urinary retention, changes in libido, menstrualirregularitiesHematologic: Decreased Hct, blood dyscrasias Other: Phlebitis and thrombosis at IV injection sites, hiccups, fever,diaphoresis, paresthesias, muscular disturbances, gynecomastia; pain,burning, and redness after IM injection Dependence: Drug dependence with withdrawal syndrome when drug isdiscontinued (more common with abrupt discontinuation of higher dosageused for longer than 4 mo) Nursing considerations -History: Hypersensitivity to benzodiazepines; psychoses, acutenarrow-angle glaucoma, shock, coma, acute alcoholic intoxication withdepression of vital signs; elderly or debilitated patients; impaired liveror kidney function; pregnancy, lactation -Physical: Weight; skin color, lesions; orientation, affect, reflexes,sensory nerve function, ophthalmologic examination; P, BP; respiratoryrate, adventitious sounds; bowel sounds, normal output, liverevaluation; normal output; LFTs, renal function tests, CBC -Do not administer intra-arterially, which may produce arteriospasm organgrene.-Do not use small veins (dorsum of hand or wrist) for IV injection.-Administer IM injections deep into muscle. -Arrange to reduce dose of midazolam if patient is also being givenopioid analgesics; reduce dosage by at least 50% and monitor patientclosely. -Monitor level of consciousness before, during, and for at least 26 hrafter administration of midazolam.-Carefully monitor P, BP, and respirations carefully duringadministration. -Keep resuscitative facilities readily available; have flumazenil availableas antidote if overdose should occur.-Keep patients in bed for 3 hr; do not permit ambulatory patients tooperate a vehicle following an injection.-Establish safety precautions if CNS changes occur (use side rails,accompany ambulating patient). -Client may experience these side effects: Drowsiness, dizziness (thesemay become less pronounced after a few days; avoid driving a car orengaging in other dangerous activities if these occur); GI upset;dreams, difficulty concentrating, fatigue, nervousness, crying (it mayhelp to know that these are effects of the drug; consult your healthcare provider if these become bothersome).-Report severe dizziness, weakness, drowsiness that persists, rash orskin lesions, visual or hearing disturbances, difficulty voiding.
12. Generic Name:Fresofol Brand Name: Propofol
Classification: sedative hypnotic; anesthetic agent Therapeutic Actions: -Propofol is a short-acting hypnotic. Its mechanism of action has notbeen well-defined.
Indications: -induction of general anesthesia in adults and in pediatric patientsgreater than 3 years of age-maintenance of anesthesia utilizing balanced techniques with otherappropriate agents such as opioids and inhalation anesthetics in adultsand pediatric patients greater than 2 months of age-produce sedation or amnesia as a supplement to local or regionalanesthetics Contraindications: -Contraindicated in pediatric patients for monitored anesthesia care(MAC) sedation or for sedation in intensive care; epileptics; usecautiously in lactation Adverse Effects: CV: Arterial hypotension; decreased systemic vascular resistance,myocardial blood flow, and oxygen consumption, palpitations, tachycardiaRespiratory: apnea, hyperventilation, bradypnea, dyspnea, wheezing,swelling of throat CNS: increased ICP, lethargy, drowsiness, euphoria, hallucinations, blurredvision, anxiety, tension, seizure, lightheadedness, fainting DERM: skin rash, flushing, urticaria Nursing Considerations: -Assess history of allergy to the components of the drug.-Use safety precautions after administration.-Advise patient that mental alertness, coordination, and physicaldexterity may be impaired for some time after administration.-For IV, do not mix with other therapeutic agents prior toadministration. Avoid mixing blood or plasma in same IV catheter.-Minimize pain associated with administration by infusing into largerveins.-Should be administered only by personnel who are trained inadministration of general anesthesia and familiar with drug.Shake well before use. Do not use if there is evidence of separation of phases of emulsion. 13. Generic Name:Hyoscine-N-butylbromide Brand Name: Buscopan
Classification: Antispasmodic; Anticholinergic Therapeutic Actions: -acts by interfering with the transmission of nerve impulses byacetylcholine in the parasympathetic nervous system. Indications: -Buscopan Tablets are indicated for the relief of spasm of the genito-urinary tract or gastro- intestinal tract and for the symptomatic relief of Irritable Bowel Syndrome Contraindications: -Buscopan Tablets should not be administered to patients withmyasthenia gravis, megacolon and narrow angle glaucoma. Inaddition, they should not be given to patients with a knownhypersensitivity to hyoscine-Nbutylbromide or any other component of the product. Adverse Effects: CNS: dizziness, anaphylactic reactions, anaphylactic shock, increased ICP,disorientation,restlessness, irritability, dizziness, drowsiness, headache, confusion,hallucination, delirium, impairedmemory CV: hypotension, tachycardia, palpitations, flushing GI: Dry mouth, constipation, nausea, epigastric distress DERM: flushing, dyshidrosis GU: Urinary retention, urinary hesitancyResp: dyspnea, bronchial plugging, depressed respiration EENT: mydriasis, dilated pupils, blurred vision, photopobia, increasedintraocular pressure,difficulty of swallowing.
Nursing Considerations: -Drug compatibility should be monitored closely in patients requiringadjunctive therapy-Avoid driving & operating machinery after parenteral administration.-Avoid strict heat
-Raise side rails as a precaution because some patients becometemporarily excited or disoriented and some develop amnesia orbecome drowsy.-Reorient patient, as needed, Tolerance may develop when therapy isprolonged-Atropine-like toxicity may cause dose related adverse reactions.Individual tolerance varies greatlyOverdose may cause curare-like effects, such as respiratory paralysis.Keep emergency equipment available.
You might also like
- Servsafe WorksheetDocument16 pagesServsafe Worksheetrialcoleman50% (4)
- Drug StudyDocument13 pagesDrug StudyGi Ey ElNo ratings yet
- Pharmacology Final Study GuideDocument9 pagesPharmacology Final Study GuideMichaelaNo ratings yet
- Mindanao State University - Iligan Institute of Technology Student: EGAO, Vanessa Jones C. - Section:260Document1 pageMindanao State University - Iligan Institute of Technology Student: EGAO, Vanessa Jones C. - Section:260Vanessa EgaoNo ratings yet
- Methyldopa, Losartan K, Ascorbic AcidDocument4 pagesMethyldopa, Losartan K, Ascorbic AcidRico Mae ValenciaNo ratings yet
- Folic AcidDocument3 pagesFolic Acidapi-37979410% (1)
- Med 3 Drug StudyDocument12 pagesMed 3 Drug StudyJinky Nacar DomingoNo ratings yet
- Drug StudyDocument17 pagesDrug StudyTherese ArellanoNo ratings yet
- Phenergan (Promethazine)Document1 pagePhenergan (Promethazine)E100% (1)
- Drug Study...Document5 pagesDrug Study...Ezra Dizon ManzanoNo ratings yet
- Dolan Drug StudyDocument3 pagesDolan Drug StudyLian Robbie BautistaNo ratings yet
- Drug StudyDocument40 pagesDrug StudyLyka Milo AvilaNo ratings yet
- Drug Study (AFP)Document10 pagesDrug Study (AFP)Summer SuarezNo ratings yet
- MorphineDocument2 pagesMorphineNinoska Garcia-Ortiz80% (5)
- DRUG STUDY - Para, Plasil, CiprofloxacinDocument5 pagesDRUG STUDY - Para, Plasil, CiprofloxacinrhegellNo ratings yet
- Nahco3 Vancomycin AmlodipineDocument3 pagesNahco3 Vancomycin AmlodipineShan Dave TupasNo ratings yet
- DORMICUMDocument1 pageDORMICUMArian Rose100% (1)
- Drug Name Mechanism of Action Administration Indication Contraindication Adverse Effects Nursing ResponsibilitiesDocument1 pageDrug Name Mechanism of Action Administration Indication Contraindication Adverse Effects Nursing ResponsibilitiesIvan Liquiran AvenadoNo ratings yet
- Magnesium Sulfate Drug StudyDocument3 pagesMagnesium Sulfate Drug StudyMonica Lyka BancaleNo ratings yet
- Nifedepine Drug StudyDocument1 pageNifedepine Drug StudyMa. Sheenadel ZamudioNo ratings yet
- PentoxifyllineDocument2 pagesPentoxifyllineAshley Nordstrom CollinsNo ratings yet
- Imipenem Cilastatin (Primaxin)Document1 pageImipenem Cilastatin (Primaxin)ENo ratings yet
- Drug StudyDocument5 pagesDrug StudyBridgette ArañesNo ratings yet
- Dextrose 50 InjectionDocument6 pagesDextrose 50 InjectionLip StickNo ratings yet
- Leoprolide Drug StudyDocument2 pagesLeoprolide Drug Studyhappymee927No ratings yet
- Drug StudyDocument5 pagesDrug Studyjanelle123 toribioNo ratings yet
- SimethiconeDocument1 pageSimethiconeDivine Dela PenaNo ratings yet
- Name of The Drug Dosage Indication and Mechanism of Action Contraindication Adverse Effects Nursing ResponsbilitiesDocument2 pagesName of The Drug Dosage Indication and Mechanism of Action Contraindication Adverse Effects Nursing ResponsbilitiesMiguel Paolo Bastillo MercadoNo ratings yet
- MisoprostolDocument3 pagesMisoprostolMichael Aditya LesmanaNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationAbigail BascoNo ratings yet
- Insulin NPHDocument1 pageInsulin NPHChristopher LeeNo ratings yet
- NifedipineDocument3 pagesNifedipineNovi YulianaNo ratings yet
- Drug Study On Gastrointestinal AgentsDocument18 pagesDrug Study On Gastrointestinal AgentsJenica ManuntagNo ratings yet
- Heparin InjectionDocument2 pagesHeparin InjectiongagandipkSNo ratings yet
- Chlorpheniramine Maleate: (klor-fen-AIR-uh-meen MAL-ee-ate)Document4 pagesChlorpheniramine Maleate: (klor-fen-AIR-uh-meen MAL-ee-ate)Nurginayah RusliNo ratings yet
- AtroventDocument2 pagesAtroventKatie McPeekNo ratings yet
- GlyburideDocument2 pagesGlyburideNinoska Garcia-OrtizNo ratings yet
- Rani Ti Dine Tramadol Ketorolac in Paracetamol Drug StudyDocument10 pagesRani Ti Dine Tramadol Ketorolac in Paracetamol Drug StudyIv'z TandocNo ratings yet
- Generic Name & Brand Name Mechanism of Action Indications and Drug Rationale Contraindications Common Side Effects Nursing ConsiderationsDocument2 pagesGeneric Name & Brand Name Mechanism of Action Indications and Drug Rationale Contraindications Common Side Effects Nursing ConsiderationsMary Shine GonidaNo ratings yet
- KaliumDocument2 pagesKaliumJustine Kaye Iballa HarligaNo ratings yet
- FNCPDocument6 pagesFNCPlovlyNo ratings yet
- Florinef (Fludrocortisone)Document3 pagesFlorinef (Fludrocortisone)E100% (1)
- Nalbuphine (Nubain)Document2 pagesNalbuphine (Nubain)Adrianne Bazo100% (1)
- Drug Study - FolfoxDocument3 pagesDrug Study - FolfoxTarquin TomadaNo ratings yet
- Drug Study Delivery RoomDocument7 pagesDrug Study Delivery RoomkhleeoNo ratings yet
- ATI DRUG TABLES Module4 Respiratory Expectorants Guaifenesin 1Document1 pageATI DRUG TABLES Module4 Respiratory Expectorants Guaifenesin 1noeyeshaveseenNo ratings yet
- Epirubicin 10Document1 pageEpirubicin 10PdianghunNo ratings yet
- Ondansetron (Zofran)Document1 pageOndansetron (Zofran)Cassie100% (1)
- Methadone HCLDocument2 pagesMethadone HCLtiffanald50% (2)
- OxaliplatinDocument10 pagesOxaliplatinlum_albertNo ratings yet
- Generic Name Brand Name Drug Classification Mechanism of Action Indications Adverse Reaction Nursing ResponsibilitiesDocument1 pageGeneric Name Brand Name Drug Classification Mechanism of Action Indications Adverse Reaction Nursing ResponsibilitiesitsmeayaNo ratings yet
- Er-Drug StudyDocument41 pagesEr-Drug Studyrc_lacampuinganyahooNo ratings yet
- CoversylDocument3 pagesCoversylianecunarNo ratings yet
- Vit K Drug Study PDFDocument2 pagesVit K Drug Study PDFA sisonNo ratings yet
- Lyrica (Pregabalin)Document2 pagesLyrica (Pregabalin)Laromac RolandNo ratings yet
- Delivery Room Drug StudyDocument9 pagesDelivery Room Drug Studymacel sibayan100% (9)
- Drug Study DRDocument6 pagesDrug Study DRBheigh Lomitao AlbueraNo ratings yet
- Drug Name Classific-Ation Therapeutic Action Indications Contraindicatio N Adverse Effects Nursing Consider - AtionDocument5 pagesDrug Name Classific-Ation Therapeutic Action Indications Contraindicatio N Adverse Effects Nursing Consider - AtionElyne BicaldoNo ratings yet
- Drug StudyDocument4 pagesDrug StudyiszahbelleNo ratings yet
- Oxytocin (Pitocin) : Slide 1Document16 pagesOxytocin (Pitocin) : Slide 1Kalesha JonesNo ratings yet
- Drug StudyDocument7 pagesDrug StudyJoy Jarin100% (1)
- Common Drugs During PregnancyDocument16 pagesCommon Drugs During Pregnancymdsoukar2000No ratings yet
- Case Study Group 2 Pediatric ManuscriptDocument26 pagesCase Study Group 2 Pediatric ManuscriptjomariNo ratings yet
- Gastrointestinal Nursing ReviewerDocument17 pagesGastrointestinal Nursing ReviewerWena Grace Nonan100% (1)
- Time USA - 20 07 2020Document103 pagesTime USA - 20 07 2020AD StrategoNo ratings yet
- Review of The TheoryDocument8 pagesReview of The TheoryPriskaCliquersNo ratings yet
- Senokot-S (Senna Concentrate 8.6mg + Docusate Sodium 50mg)Document2 pagesSenokot-S (Senna Concentrate 8.6mg + Docusate Sodium 50mg)E100% (1)
- Med Surg AnswersDocument23 pagesMed Surg Answersedoble67% (3)
- Fitrawati Arifuddin - Nursing Care Plan Deficiency of Fluid VolumeDocument12 pagesFitrawati Arifuddin - Nursing Care Plan Deficiency of Fluid VolumefitrawatiarifuddinNo ratings yet
- Ginger: Ginger, Slices, Fresh 1.00 TBS (6.00 Grams) Calories: 5 GIDocument6 pagesGinger: Ginger, Slices, Fresh 1.00 TBS (6.00 Grams) Calories: 5 GIMart BrendzNo ratings yet
- Drug StudyDocument4 pagesDrug Studygracebel reyesNo ratings yet
- Antiemetic Drug Class ReviewDocument24 pagesAntiemetic Drug Class ReviewNyume Lathifah HanumNo ratings yet
- Herb&Patent Pills PrescriptionsDocument113 pagesHerb&Patent Pills PrescriptionsMassages/Acupuncture Manual OsteopathNo ratings yet
- Chionanthus Virginica.: Common Names.Document15 pagesChionanthus Virginica.: Common Names.Dr Rushen SinghNo ratings yet
- A Step-By-Step Guide To Performing A Complete Abdominal ExaminationDocument8 pagesA Step-By-Step Guide To Performing A Complete Abdominal Examinationjojohnson250No ratings yet
- Adrmg CapecitabineDocument9 pagesAdrmg CapecitabineLauraNo ratings yet
- Characteristics of Patients With Acute Appendicitis at Rsup Dr. M. Djamil Padang Year 2017-2019Document12 pagesCharacteristics of Patients With Acute Appendicitis at Rsup Dr. M. Djamil Padang Year 2017-2019elsy oktaviaNo ratings yet
- 5534 21456 1 PBDocument8 pages5534 21456 1 PBAkhawat Ahir ZamanNo ratings yet
- ClinicalOpiateWithdrawalScale PDFDocument2 pagesClinicalOpiateWithdrawalScale PDFRajamanitiNo ratings yet
- Vibration Disease EngDocument53 pagesVibration Disease EngVeronica SecrieruNo ratings yet
- Discharge Plan: MedicationDocument2 pagesDischarge Plan: MedicationKathleen Joy PingenNo ratings yet
- FDA Response - Public Version - Vanda Pharmaceuticals, Inc. v. Food and Drug Administration Et AlDocument55 pagesFDA Response - Public Version - Vanda Pharmaceuticals, Inc. v. Food and Drug Administration Et AlKirk HartleyNo ratings yet
- Family Home Remedies by Nadeem Y. MuftiDocument3 pagesFamily Home Remedies by Nadeem Y. MuftinymuftiNo ratings yet
- 3648 PresintionDocument9 pages3648 Presintionsajjad khanNo ratings yet
- Chemotherapy For Breast CancerDocument40 pagesChemotherapy For Breast Canceremilia candraNo ratings yet
- Webb 2018 Hepatic Lipidosis Clinical Review Drawn From Collective EffortDocument11 pagesWebb 2018 Hepatic Lipidosis Clinical Review Drawn From Collective EffortJulia Maria dos SantosNo ratings yet
- M&M Hepatocellular CarcinomaDocument68 pagesM&M Hepatocellular Carcinomacharmaine BallanoNo ratings yet
- Metoclopramide CNS: Anxiety,: Metozolv ODT, ReglanDocument15 pagesMetoclopramide CNS: Anxiety,: Metozolv ODT, ReglanwendyNo ratings yet
- Kents New RemediesDocument168 pagesKents New RemediesluckyNo ratings yet
- MATERIA MEDICA1 - UpdatedDocument26 pagesMATERIA MEDICA1 - UpdatedJerald BaliteNo ratings yet