Ecg assessment of ihd
- 1. Presented by Aser mohamed kamal
- 2. 1842- Italian scientist Carlo Matteucci realizes that electricity is associated with the heart beat 1876- Irish scientist Marey analyzes the electric pattern of frog’s heart 1895 - William Einthoven , credited for the invention of EKG 1906 - using the string electrometer EKG, William Einthoven diagnoses some heart problems
- 3. 1924 - the noble prize for physiology or medicine is given to William Einthoven for his work on EKG 1938 -AHA and Cardiac society of great Britan defined and position of chest leads 1942- Goldberger increased Wilson’s Unipolar lead voltage by 50% and made Augmented leads 2005- successful reduction in time of onset of chest pain and PTCA by wireless transmission of ECG on his PDA.
- 6. An electrocardiogram (EKG or ECG) is a test that checks for problems with the electrical activity of your heart. An EKG translates the heart's electrical activity into line tracings on paper. The spikes and dips in the line tracings are called waves. The heart is a muscular pump made up of four chambers .
- 7. Sinoatrial node AV node Bundle of His Bundle Branches Purkinje fibers
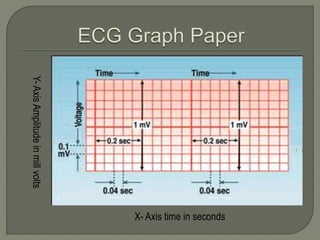
- 8. X- Axis time in seconds Y-AxisAmplitudeinmillvolts
- 9. X-Axis represents time - Scale X-Axis – 1 mm = 0.04 sec Y-Axis represents voltage - Scale Y-Axis – 1 mm = 0.1 mV One big square on X-Axis = 0.2 sec (big box) Two big squares on Y-Axis = 1 milli volt (mV) Each small square is 0.04 sec (1 mm in size) Each big square on the ECG represents 5 small squares = 0.04 x 5 = 0.2 seconds 5 such big squares = 0.2 x 5 = 1sec = 25 mm One second is 25 mm or 5 big squares One minute is 5 x 60 = 300 big squares
- 10. P wave PR Interval QRS complex ST segment T Wave QT Interval RR Interval
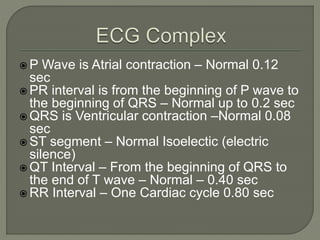
- 11. P Wave is Atrial contraction – Normal 0.12 sec PR interval is from the beginning of P wave to the beginning of QRS – Normal up to 0.2 sec QRS is Ventricular contraction –Normal 0.08 sec ST segment – Normal Isoelectic (electric silence) QT Interval – From the beginning of QRS to the end of T wave – Normal – 0.40 sec RR Interval – One Cardiac cycle 0.80 sec
- 13. # of Boxes DurationThe Wave or Interval (3)0.12 secP wave : Atrial contraction (5)0.20 secPR interval – P to begin. of QRS (2)0.08 secQRS complex - Ventricular IsoelectricST segment - Electrical silence (3)0.12 secT wave - repolarization (2)0.08 secQRS interval – Ventricular cont. (10)0.40 secQT interval - From Q to T end (5)0.20 secTP segment - Electrical silence
- 14. 1 2 3 4 5 6 7 8
- 15. 1. P wave – Atrial contraction = 0.12 sec (3 small boxes) 2. PR Interval – P + AV delay = 0.20 sec (5 small boxes) 3. Q wave – Septal = < 3 mm, < 0.04 sec (1 small box) 4. R wave – Ventricular contraction < 15 mm 5. S wave – complimentary to R < 15 mm 6. ST segment – Isoelectric – decides our fate 7. T wave – ventricular repolarization – friend of ST 8. TP segment – ventricular relaxation – shortened in tachycardia
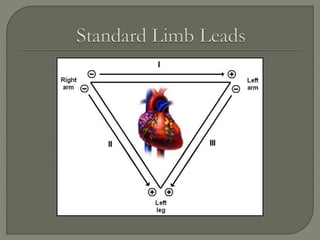
- 16. which measure the difference in electrical potential between two points 1. Bipolar Leads: Two different points on the body 2. Unipolar Leads: One point on the body and a virtual reference point with zero electrical potential, located in the center of the heart
- 17. + + + - - - R L F R F L
- 18. Standard ECG is recorded in 12 leads Six Limb leads – L1, L2, L3, aVR, aVL, aVF Six Chest Leads – V1 V2 V3 V4 V5 and V6 L1, L2 and L3 are called bipolar leads L1 between LA and RA L2 between LF and RA L3 between LF and LA
- 19. ++ + Lead aVR Lead aVL Lead aVF R L F
- 20. Standard ECG is recorded in 12 leads Six Limb leads – L1, L2, L3, aVR, aVL, aVF Six Chest Leads – V1 V2 V3 V4 V5 and V6 aVR, aVL, aVF are called unipolar leads aVR – from Right Arm Positive aVL – from Left Arm Positive aVF – from Left Foot Positive
- 21. The standard EKG has 12 leads: 3 Standard Limb Leads 3 Augmented Limb Leads 6 Precordial Leads
- 29. Precardial (chest) Lead Position V1 Fourth ICS, right sternal border V2 Fourth ICS, left sternal border V3 Equidistant between V2 and V4 V4 Fifth ICS, left Mid clavicular Line V5 Fifth ICS Left anterior axillary line V6 Fifth ICS Left mid axillary line
- 36. Professor Chamberlains 10 rules of normal:-
- 37. PR interval should be 120 to 200 milliseconds or 3 to 5 little squares
- 38. The width of the QRS complex should not exceed 110 ms, less than 3 little squares
- 39. The QRS complex should be dominantly upright in leads I and II
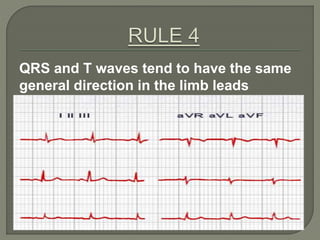
- 40. QRS and T waves tend to have the same general direction in the limb leads
- 41. All waves are negative in lead aVR
- 42. The R wave must grow from V1 to at least V4 The S wave must grow from V1 to at least V3 and disappear in V6
- 43. The ST segment should start isoelectric except in V1 and V2 where it may be elevated
- 44. The P waves should be upright in I, II, and V2 to V6
- 45. There should be no Q wave or only a small q less than 0.04 seconds in width in I, II, V2 to V6
- 46. The T wave must be upright in I, II, V2 to V6
- 47. Correct Lead placement and good contact Proper earth connection, avoid other gadgets Deep inspiration record of L3, aVF Compare serial ECGs if available Relate the changes to Age, Sex, Clinical history Consider the co-morbidities that may effect ECG Make a xerox copy of the record for future use Interpret systematically to avoid errors
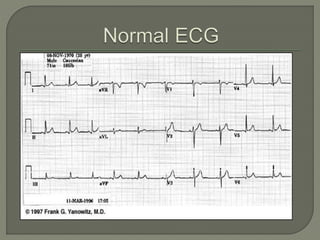
- 49. Standardization – 10 mm (2 boxes) = 1 mV Double and half standardization if required Sinus Rhythm – Each P followed by QRS, R-R constant P waves – always examine for in L2, V1, L1 QRS positive in L1, L2, L3, aVF and aVL. – Neg in aVR QRS is < 0.08 narrow, Q in V5, V6 < 0.04, < 3 mm R wave progression from V1 to V6, QT interval < 0.4 Axis normal – L1, L3, and aVF all will be positive ST Isoelectric, T waves ↑, Normal T↓ in aVR,V1, V2
- 50. Normal Resting ECG – cannot exclude disease Ischemia may be covert – supply / demand equation Changes of MI take some time to develop in ECG Mild Ventricular hypertrophy - not detectable in ECG Some of the ECG abnormalities are non specific Single ECG cannot give progress – Need serial ECGs ECG changes not always correlate with Angio results Paroxysmal events will be missed in single ECG
- 51. May have slight left axis due to rotation of heart May have high voltage QRS – simulating LVH Mild slurring of QRS but duration < 0.09 J point depression, early repolarization T inversions in V2, V3 and V4 – Juvenile T ↓ Similarly in women also T↓ Low voltages in obese women and men Non cardiac causes of ECG changes may occur
- 52. Always positive in lead I and II Always negative in lead aVR < 3 small squares in duration < 2.5 small squares in amplitude Commonly biphasic in lead V1 Best seen in leads II
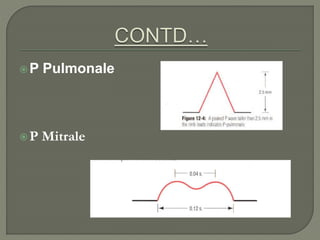
- 53. -Tall (> 2.5 mm), pointed P waves (P Pulmonale)
- 54. Notched/bifid (‘M’ shaped) P wave (P ‘mitrale’) in limb leads
- 56. WPW (Wolff- Parkinson-White) Syndrome Accessory pathway (Bundle of Kent) allows early activation of the ventricle (delta wave and short PR interval)
- 57. First degree Heart Block
- 58. Nonpathological Q waves may present in I, III, aVL, V5, and V6 R wave in lead V6 is smaller than V5 Depth of the S wave, should not exceed 30 mm Pathological Q wave > 2mm deep and > 1mm wide or > 25% amplitude of the subsequent R wave
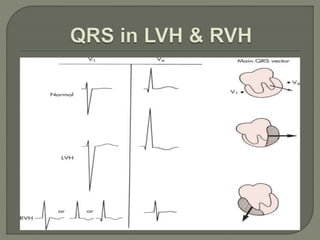
- 60. Sokolow & Lyon Criteria S in V1+ R in V5 or V6 > 35 mm An R wave of 11 to 13 mm (1.1 to 1.3 mV) or more in lead aVL is another sign of LVH
- 61. ST Segment is flat (isoelectric) Elevation or depression of ST segment by 1 mm or more “J” (Junction) point is the point between QRS and ST segment
- 63. Normal T wave is asymmetrical, first half having a gradual slope than the second Should be at least 1/8 but less than 2/3 of the amplitude of the R T wave amplitude rarely exceeds 10 mm Abnormal T waves are symmetrical, tall, peaked, biphasic or inverted. T wave follows the direction of the QRS deflection.
- 65. 1. Total duration of Depolarization and Repolarization 2. QT interval decreases when heart rate increases 3. For HR = 70 bpm, QT<0.40 sec. 4. QT interval should be 0.35 0.45 s, 5. Should not be more than half of the interval between adjacent R waves (RR interval).
- 67. Rule of 300/1500 10 Second Rule
- 68. Count the number of “big boxes” between two QRS complexes, and divide this into 300. (smaller boxes with 1500) for regular rhythms.
- 69. EKGs record 10 seconds of rhythm per page, Count the number of beats present on the EKG Multiply by 6 For irregular rhythms.
- 70. (300 / 6) = 50 bpm
- 71. (300 / ~ 4) = ~ 75 bpm
- 72. 33 x 6 = 198 bpm
- 73. (300 / 1.5) = 200 bpm
- 78. Is a Coronary artery disease is most commonly caused by obstructive atherosclerosis of epicardial coronary arteries. This leads to an inadequate perfusion of the myocardium and causes an imbalance between myocardial tissue oxygen supply and demand (myocardial ischemia). Ischaemic (or ischemic) heart disease is a disease characterized by reduced blood supply to the heart. It is the most common cause of death in most western countries. Ischaemia means a "reduced blood supply". The coronary arteries supply blood to the heart muscle and no alternative blood supply exists, so a blockage in the coronary arteries reduces the supply of blood to heart muscle.
- 79. Most ischaemic heart disease is caused by atherosclerosis, usually present even when the artery lumens appear normal by angiography. Initially there is sudden severe narrowing or closure of either the large coronary arteries and/or of coronary artery end branches by debris showering downstream in the flowing blood. It is usually felt as angina, especially if a large area is affected. The narrowing or closure is predominantly caused by the covering of atheromatous plaques within the wall of the artery rupturing, in turn leading to a heart attack (Heart attacks caused by just artery narrowing are rare). A heart attack causes damage to heart muscle by cutting off its blood supply.
- 80. 1.Poor R wave progression : Loss of gradual progression (increase) in amplitude of R waves in chest leads from V1V6 if this gradual increase is lost this is sign of IHD . 2.Q waves: Presence of deep Q waves in related leads (inferior , antoroseptal and lateral ) donates old MI.
- 81. 3. T wave inversion in related leads MAY BE a sign of IHD . Other causes : - LVH - stroke -pericardaities -normal in V1,V2 (in female)
- 82. 4. ST segment : Elevation :- - acute MI . - acute percardities . -early repolarization pattern in young age Depression :- -horizontal depression IHD(angina). -down sloping depression IHD(angina).
- 83. 5. Lost of R wave progression : Ischemic cardiomyopathy .
- 84. 1.LA: a) Wide P wave in limb leads . b) Biphasic P wave in V1: -ve component deeper than +ve component . 2.LV: a) R amplitude in aVL >13mm. b) Tallest R wave + deepest >35mm . c) R wave or S wave > 25mm .
- 85. 3. RA: tall peaked P wave in limb leads. 4. RV: tall R waves in V1 , V2 .