Abstract
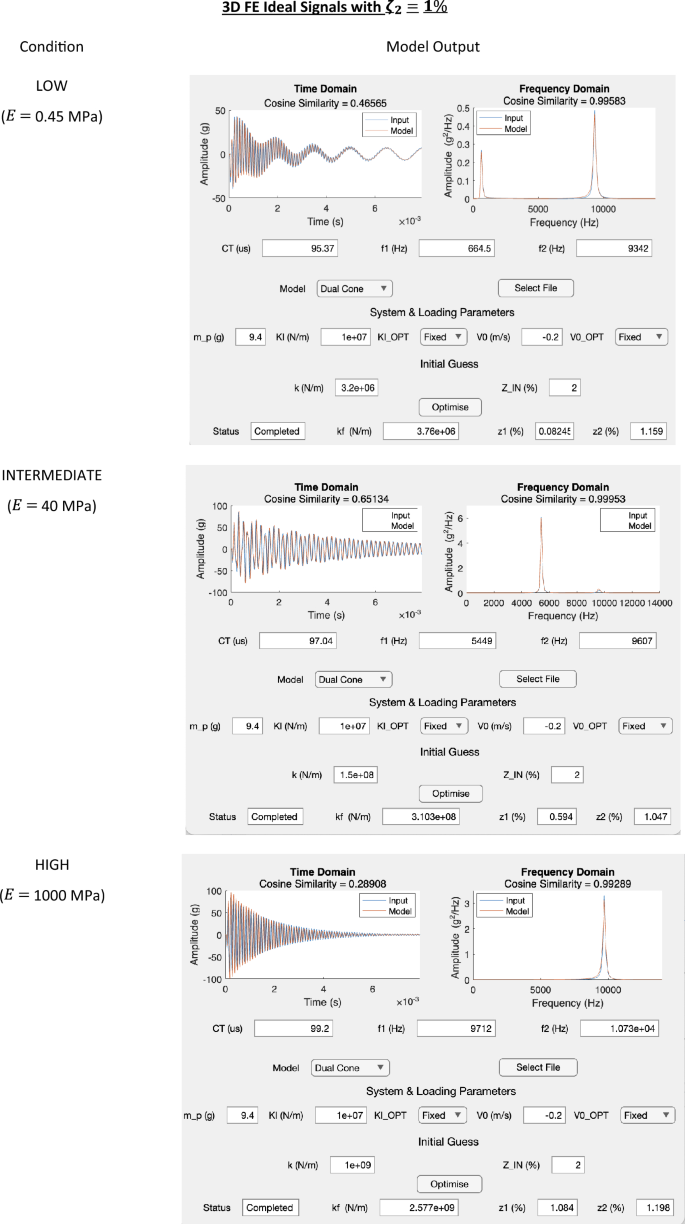
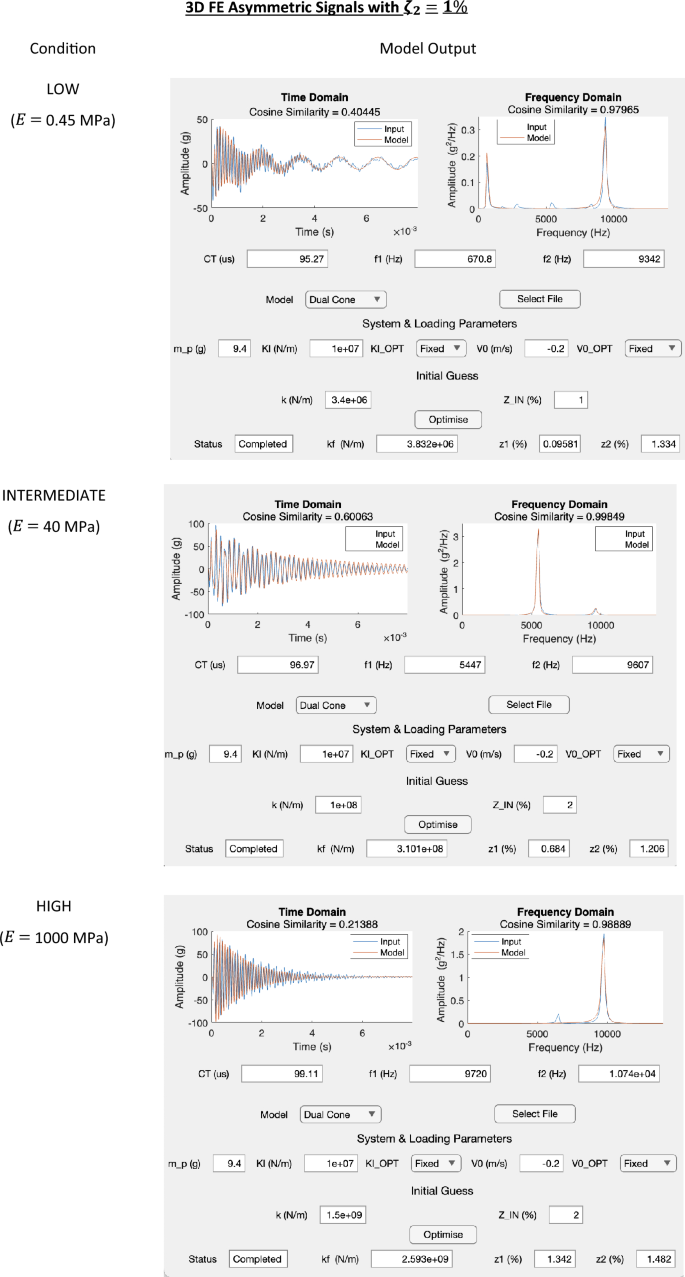
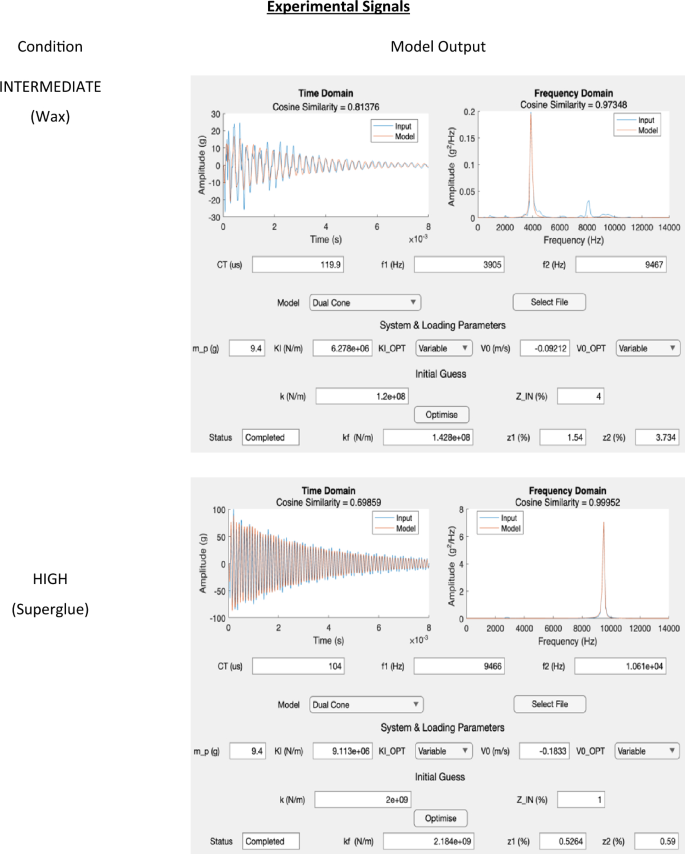
Evaluating the bone–implant interface (BII) properties of osseointegrated transfemoral (TFA) implants is important for early failure detection and prescribing loads during rehabilitation. The objective of this work is to derive and validate a 1D finite element (FE) model of the Osseointegrated Prosthetic Limb (OPL) TFA system that can: (1) model its dynamic behaviour and (2) extract the BII properties. The model was validated by: (1) comparing the 1D FE formulation to the analytical and 3D FE solutions for a simplified cylinder, (2) comparing the vibration modes of the actual TFA geometry using 1D and 3D FE models, and (3) evaluating the BII properties for three extreme conditions (LOW, INTERMEDIATE, and HIGH) generated using 3D FE and experimental (where the implant was embedded, using different adhesives, in synthetic femurs) signals for additional validation. The modes predicted by the 1D FE model converged to the analytical and the 3D FE solutions for the cylinder. The 1D model also matched the 3D FE solution with a maximum frequency difference of 2.02% for the TFA geometry. Finally, the 1D model extracted the BII stiffness and the system’s damping properties for the three conditions generated using the 3D FE simulations and the experimental INTERMEDIATE and HIGH signals. The agreement between the 1D FE and the 3D FE solutions for the TFA geometry indicates that the 1D model captures the system’s dynamic behaviour. Distinguishing between the different BII conditions demonstrates the 1D model’s potential use for the non-invasive clinical evaluation of the TFA BII properties.








Similar content being viewed by others
References
Brånemark, R., P. I. Brånemark, B. Rydevik, and R. R. Myers. Osseointegration in skeletal reconstruction and rehabilitation: a review. J. Rehabil. Res. Dev. 38(2):175–181, 2001.
Hagberg, K., and R. Brånemark. One hundred patients treated with osseointegrated transfemoral amputation prostheses—rehabilitation perspective. J. Rehabil. Res. Dev. 46(3):331–344, 2009. https://doi.org/10.1682/JRRD.2008.06.0080.
Maryniak, A., B. Laschowski, and J. Andrysek. Technical overview of osseointegrated transfemoral prostheses: orthopedic surgery and implant design centered. J. Eng. Sci. Med. Diagn. Ther. 1:1–7, 2018. https://doi.org/10.1115/1.4039105.
Hoellwarth, J. S., K. Tetsworth, S. R. Rozbruch, M. B. Handal, A. Coughlan, and M. Al Muderis. Osseointegration for Amputees. JBJS Rev. 8(3):1–10, 2020. https://doi.org/10.2106/jbjs.rvw.19.00043.
Al Muderis, M., W. Lu, K. Tetsworth, B. Bosley, and J. J. Li. Single-stage osseointegrated reconstruction and rehabilitation of lower limb amputees: the Osseointegration Group of Australia Accelerated Protocol-2 (OGAAP-2) for a prospective cohort study. BMJ Open. 7(3):1–4, 2017. https://doi.org/10.1136/bmjopen-2016-013508.
Al Muderis, M., et al. The osseointegration group of Australia accelerated protocol (ogaap-1) for two-stage osseointegrated reconstruction of amputated limbs. Bone Joint J. 98B(7):952–960, 2016. https://doi.org/10.1302/0301-620X.98B7.37547.
Hoellwarth, J. S., A. Oomatia, K. Tetsworth, E. Vrazas, and M. Al Muderis. Bone density changes after five or more years of unilateral lower extremity osseointegration: observational cohort study. Bone Rep. 2023. https://doi.org/10.1016/j.bonr.2023.101682.
Gao, X., M. Fraulob, and G. Haïat. Biomechanical behaviours of the bone—implant interface: : a review. J. R. Soc. Interface. 16:20190259, 2019.
Zanetti, E. M., G. Pascoletti, M. Cali, C. Bignardi, and G. Franceschini. Clinical assessment of dental implant stability during follow-up: What is actually measured, and perspectives. Biosensors (Basel). 8(68):1–18, 2018. https://doi.org/10.3390/bios8030068.
Tillander, J., K. Hagberg, Ö. Berlin, L. Hagberg, and R. Brånemark. Osteomyelitis risk in patients with transfemoral amputations treated with osseointegration prostheses. Clin. Orthop. Relat. Res. 475(12):3100–3108, 2017. https://doi.org/10.1007/s11999-017-5507-2.
Nebergall, A., C. Bragdon, A. Antonellis, J. Kärrholm, R. Brånemark, and H. Malchau. Stable fixation of an osseointegated implant system for above-the-knee amputees: titel RSA and radiographic evaluation of migration and bone remodeling in 55 cases. Acta Orthop. 83(2):121–128, 2012. https://doi.org/10.3109/17453674.2012.678799.
Hansen, R. L., B. L. Langdahl, P. H. Jørgensen, K. K. Petersen, K. Søballe, and M. Stilling. Does migration of osseointegrated implants for transfemoral amputees predict later revision? A prospective 2-year radiostereometric analysis with 5-years clinical follow-up. Orthop. Traumatol.: Surg. Res. 105(5):1013–1020, 2019. https://doi.org/10.1016/j.otsr.2019.05.010.
Westover, L., G. Faulkner, W. Hodgetts, and D. Raboud. Advanced system for implant stability testing (ASIST). J. Biomech. 49:3651–3659, 2016. https://doi.org/10.1016/j.jbiomech.2016.09.043.
Westover, L., G. Faulkner, W. Hodgetts, and D. Raboud. Comparison of implant stability measurement devices for bone-anchored hearing aid systems. J. Prosthet. Dent. 119(1):178–184, 2018. https://doi.org/10.1016/j.prosdent.2017.02.021.
Pattijn, V., C. Van Lierde, G. Van Der Perre, I. Naert, and J. Vander Sloten. The resonance frequencies and mode shapes of dental implants: rigid body behaviour versus bending behaviour. A numerical approach. J. Biomech. 39(5):939–947, 2006. https://doi.org/10.1016/j.jbiomech.2005.01.035.
Zanetti, E. M., et al. Modal analysis for implant stability assessment: sensitivity of this methodology for different implant designs. Dent. Mater. 34(8):1235–1245, 2018. https://doi.org/10.1016/j.dental.2018.05.016.
Mohamed, M., H. Pisavadia, and L. Westover. A finite element model for evaluating the effectiveness of the Advanced System for Implant Stability Testing (ASIST). J. Biomech. 2021. https://doi.org/10.1016/j.jbiomech.2021.110570.
Shao, F., W. Xu, A. Crocombe, and D. Ewins. Natural frequency analysis of osseointegration for trans-femoral implant. Ann. Biomed. Eng. 35(5):817–824, 2007. https://doi.org/10.1007/s10439-007-9276-z.
Cairns, N. J., M. J. Pearcy, J. Smeathers, and C. J. Adam. Simulating the bone-titanium interfacial changes around transfemoral osseointegrated implants using physical models and modal analysis. In: 1st International Workshop on Innovative Simulation for Health Care, IWISH 2012, Held at the International Multidisciplinary Modeling and Simulation Multiconference, I3M 2012, 2012, pp. 1–9.
Cairns, N. J., M. J. Pearcy, J. Smeathers, and C. J. Adam. Ability of modal analysis to detect osseointegration of implants in transfemoral amputees: a physical model study. Med. Biol. Eng. Comput. 51(1–2):39–47, 2013. https://doi.org/10.1007/s11517-012-0962-0.
Mohamed, M., D. Raboud, J. S. Hebert, and L. Westover. Stabillity assessment of osseointegrated transfemoral bone-implant systems using finite element modal analysis. Prog. Can. Mech. Eng. 2022. https://doi.org/10.7939/r3-s23c-as14.
Mohamed, M. Mathematical and Experimental Modelling of the Dynamic Response of the Transfemoral Bone Implant System and Bone Anchored Hearing Aids and its Potential Application to the Non-invasive Evaluation of Implant Stability, Thesis, University of Alberta, Edmonton, 2023.
Reddy, J. N. Introduction to the Finite Element Method, 4th ed. New York: McGraw Hill, 2019.
Rao, S. Vibration of Continous Systems, 2nd ed. Hoboken: Wiley, 2019.
Chopra, A. K. Dynamics of Structures Theory and Applications to Earthquake Engineering, 4th ed. Hoboken: Prentice Hall, 2012.
Huiskes, R. On the modelling of long bones in structural analyses. J. Biomech. 15(1):65–69, 1982. https://doi.org/10.1016/0021-9290(82)90036-7.
Mohamed, M., and L. Westover. Evaluating the dynamic behavior of bone anchored hearing aids using a finite element model and its applications to implant stability assessment. Med. Biol. Eng. Comput. 60:2779–2795, 2022. https://doi.org/10.1007/s11517-022-02607-y.
Smith, M. ABAQUS/Standard User’s Manual, Version 6.9. Dassault Systèmes Simulia Corp., 2009.
MatWeb, “Overview of materials for Cyanoacrylate Adhesives,” https://www.matweb.com/search/datasheet.aspx?matguid=d0d7dbec7666421caf8aa08724b634c5&ckck=1.
Hossain, M. E., C. Ketata, and M. R. Islam. Experimental study of physical and mechanical properties of natural and synthetic waxes using uniaxial compressive strength test. In: Proceedings of the Third International Conference on Modeling, Simulation and Applied Optimization, Sharjah, 2009.
Engineering Toolbox, Metals and Alloys-Densities. [Online]. https://www.engineeringtoolbox.com/metal-alloys-densities-d_50.html.
SAWBONES. Biomechanical Materials for Precise, Repeatable Testing. [Online]. https://www.sawbones.com/biomechanical-product-info. Accessed 21 Jan 2022.
Waide, V., L. Cristofolini, J. Stolk, N. Verdonschot, G. J. Boogaard, and A. Toni. Modelling the fibrous tissue layer in cemented hip replacements: experimental and finite element methods. J. Biomech. 37(1):13–26, 2004. https://doi.org/10.1016/S0021-9290(03)00258-6.
Ali, S. K., Z. M. Aydam, and B. M. Rashed. Similarity metrics for classification: a review. IOP Conf. Ser. Mater. Sci. Eng. 928(3):032052, 2020. https://doi.org/10.1088/1757-899X/928/3/032052.
Sennerby, L., and N. Meredith. Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontol. 47(1):51–66, 2000. https://doi.org/10.1111/j.1600-0757.2008.00267.x.
Meredith, N. A review of nondestructive test methods and their application to measure the stability and osseointegration of bone anchored endosseous implants. Crit. Rev. Biomed. Eng. 26(4):275–291, 1998.
Avitable, P. Modal Testing: A Practitioner’s Guide. Hoboken: Wiley, 2018.
Cairns, N. J., C. J. Adam, M. J. Pearcy, and J. Smeathers. Evaluation of modal analysis techniques using physical models to detect osseointegration of implants in transfemoral amputees. In: Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS, 2011, pp. 1600–1603.
Westover, L., G. Faulkner, W. Hodgetts, F. Kamal, E. Lou, and D. Raboud. Longitudinal evaluation of bone-anchored hearing aid implant stability using the advanced system for implant stability testing (ASIST). Otol. Neurotol. 39:e489–e495, 2018. https://doi.org/10.1097/MAO.0000000000001815.
Robertson, R. G. Multiple Impulse Method of Tooth Mobility Assessment. London: University of London, 1995.
Acknowledgments
The authors would like to express their gratitude to Professor Gary Faulkner for his work and support on this study. This research was supported and funded by MITACS, NSERC, Suncor Energy Inc. This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs through FY20 Peer-Reviewed Orthopaedic Research Program, endorsed by the Department of Defense under Award No. W81XWH-21-1-0857. Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the Department of Defense.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest to be reported for this article.
Additional information
Associate Editor Joel Stitzel oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A: Analytical Solution for a Uniform Cylinder
Parameter | Symbol | Magnitude |
|---|---|---|
Mode | \(N\) | \(1\) or \(2\) |
Length | \(L ({\text{m}})\) | \(0.1\) |
Elastic Modulus | \(E ({\text{Pa}})\) | \(100\times {10}^{9}\) |
Mass Density | \(\rho ({\text{Kg/{m}}}^{3})\) | 4400 |
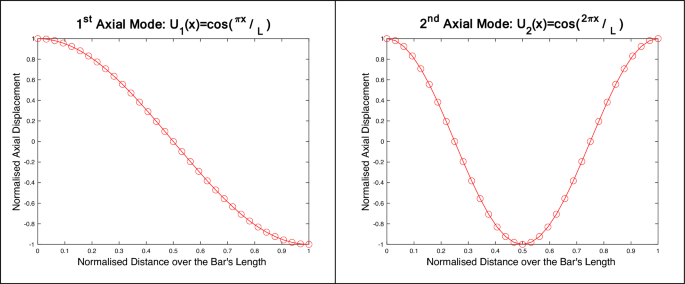
Appendix B: 1D FE Application Outputs
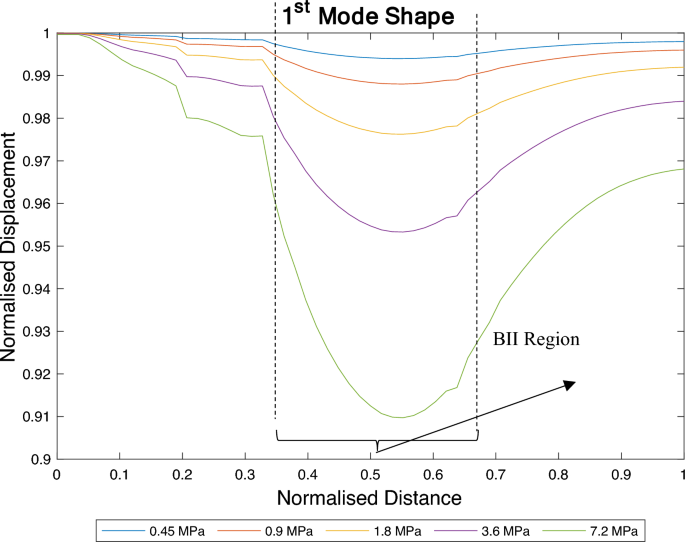
Appendix C: Nature of the 1st Mode Shape for Different BII Conditions
See Fig. 9.
Changes to the nature of the 1st axial mode for different interface conditions. As the interface stiffness increases, the BII introduces more resistance to the implant’s motion. The degree of relative sliding decreases as the stiffness of the BII increases and in turn the 1st mode of vibration becomes more observable
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mohamed, M., Beaudry, E., Shehata, A.W. et al. Evaluation of the Transfemoral Bone–Implant Interface Properties Using Vibration Analysis. Ann Biomed Eng (2024). https://doi.org/10.1007/s10439-024-03561-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10439-024-03561-6