REPORT
Biallelic Variants in UBA5 Link Dysfunctional
UFM1 Ubiquitin-like Modifier Pathway
to Severe Infantile-Onset Encephalopathy
Mikko Muona,1,2,3,4,27,28 Ryosuke Ishimura,5,6,28 Anni Laari,2,3,4,28 Yoshinobu Ichimura,5
Tarja Linnankivi,7 Riikka Keski-Filppula,8,9,10 Riitta Herva,11 Heikki Rantala,8,9,12 Anders Paetau,13
Minna Pöyhönen,14 Miki Obata,5 Takefumi Uemura,15 Thomas Karhu,2,3,4 Norihisa Bizen,16
Hirohide Takebayashi,16 Shane McKee,17 Michael J. Parker,18 Nadia Akawi,19 Jeremy McRae,19
Matthew E. Hurles,19 the DDD Study, Outi Kuismin,8,9,10 Mitja I. Kurki,1,20,21,22
Anna-Kaisa Anttonen,2,3,4,14 Keiji Tanaka,6 Aarno Palotie,1,19,21,22,23,24,25,26 Satoshi Waguri,15
Anna-Elina Lehesjoki,2,3,4,29,* and Masaaki Komatsu5,29,*
The ubiquitin fold modifier 1 (UFM1) cascade is a recently identified evolutionarily conserved ubiquitin-like modification system whose
function and link to human disease have remained largely uncharacterized. By using exome sequencing in Finnish individuals with severe epileptic syndromes, we identified pathogenic compound heterozygous variants in UBA5, encoding an activating enzyme for
UFM1, in two unrelated families. Two additional individuals with biallelic UBA5 variants were identified from the UK-based Deciphering
Developmental Disorders study and one from the Northern Finland Intellectual Disability cohort. The affected individuals (n ¼ 9) presented in early infancy with severe irritability, followed by dystonia and stagnation of development. Furthermore, the majority of individuals display postnatal microcephaly and epilepsy and develop spasticity. The affected individuals were compound heterozygous
for a missense substitution, c.1111G>A (p.Ala371Thr; allele frequency of 0.28% in Europeans), and a nonsense variant or c.164G>A
that encodes an amino acid substitution p.Arg55His, but also affects splicing by facilitating exon 2 skipping, thus also being in effect
a loss-of-function allele. Using an in vitro thioester formation assay and cellular analyses, we show that the p.Ala371Thr variant is hypomorphic with attenuated ability to transfer the activated UFM1 to UFC1. Finally, we show that the CNS-specific knockout of Ufm1 in
mice causes neonatal death accompanied by microcephaly and apoptosis in specific neurons, further suggesting that the UFM1 system
is essential for CNS development and function. Taken together, our data imply that the combination of a hypomorphic p.Ala371Thr
variant in trans with a loss-of-function allele in UBA5 underlies a severe infantile-onset encephalopathy.
Post-translational modifications through attachment of
ubiquitin or ubiquitin-like proteins (UBLs) are involved
in various biological processes.1 There are eight human
UBL-conjugating systems, in which each UBL is attached
to specific proteins or lipids usually through three-step cascades involving E1-, E2-, and E3-like enzymes.2 UBA5 is an
E1-like (activating) enzyme for the most recently identified
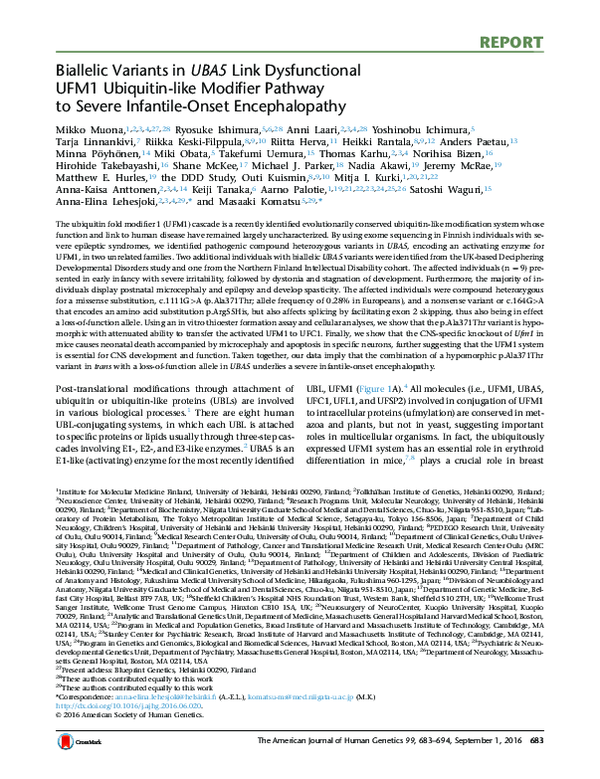
UBL, UFM1 (Figure 1A).4 All molecules (i.e., UFM1, UBA5,
UFC1, UFL1, and UFSP2) involved in conjugation of UFM1
to intracellular proteins (ufmylation) are conserved in metazoa and plants, but not in yeast, suggesting important
roles in multicellular organisms. In fact, the ubiquitously
expressed UFM1 system has an essential role in erythroid
differentiation in mice,7,8 plays a crucial role in breast
1
Institute for Molecular Medicine Finland, University of Helsinki, Helsinki 00290, Finland; 2Folkhälsan Institute of Genetics, Helsinki 00290, Finland;
Neuroscience Center, University of Helsinki, Helsinki 00290, Finland; 4Research Programs Unit, Molecular Neurology, University of Helsinki, Helsinki
00290, Finland; 5Department of Biochemistry, Niigata University Graduate School of Medical and Dental Sciences, Chuo-ku, Niigata 951-8510, Japan; 6Laboratory of Protein Metabolism, The Tokyo Metropolitan Institute of Medical Science, Setagaya-ku, Tokyo 156-8506, Japan; 7Department of Child
Neurology, Children’s Hospital, University of Helsinki and Helsinki University Hospital, Helsinki 00290, Finland; 8PEDEGO Research Unit, University
of Oulu, Oulu 90014, Finland; 9Medical Research Center Oulu, University of Oulu, Oulu 90014, Finland; 10Department of Clinical Genetics, Oulu University Hospital, Oulu 90029, Finland; 11Department of Pathology, Cancer and Translational Medicine Research Unit, Medical Research Center Oulu (MRC
Oulu), Oulu University Hospital and University of Oulu, Oulu 90014, Finland; 12Department of Children and Adolescents, Division of Paediatric
Neurology, Oulu University Hospital, Oulu 90029, Finland; 13Department of Pathology, University of Helsinki and Helsinki University Central Hospital,
Helsinki 00290, Finland; 14Medical and Clinical Genetics, University of Helsinki and Helsinki University Hospital, Helsinki 00290, Finland; 15Department
of Anatomy and Histology, Fukushima Medical University School of Medicine, Hikarigaoka, Fukushima 960-1295, Japan; 16Division of Neurobiology and
Anatomy, Niigata University Graduate School of Medical and Dental Sciences, Chuo-ku, Niigata 951-8510, Japan; 17Department of Genetic Medicine, Belfast City Hospital, Belfast BT9 7AB, UK; 18Sheffield Children’s Hospital NHS Foundation Trust, Western Bank, Sheffield S10 2TH, UK; 19Wellcome Trust
Sanger Institute, Wellcome Trust Genome Campus, Hinxton CB10 1SA, UK; 20Neurosurgery of NeuroCenter, Kuopio University Hospital, Kuopio
70029, Finland; 21Analytic and Translational Genetics Unit, Department of Medicine, Massachusetts General Hospital and Harvard Medical School, Boston,
MA 02114, USA; 22Program in Medical and Population Genetics, Broad Institute of Harvard and Massachusetts Institute of Technology, Cambridge, MA
02141, USA; 23Stanley Center for Psychiatric Research, Broad Institute of Harvard and Massachusetts Institute of Technology, Cambridge, MA 02141,
USA; 24Program in Genetics and Genomics, Biological and Biomedical Sciences, Harvard Medical School, Boston, MA 02114, USA; 25Psychiatric & Neurodevelopmental Genetics Unit, Department of Psychiatry, Massachusetts General Hospital, Boston, MA 02114, USA; 26Department of Neurology, Massachusetts General Hospital, Boston, MA 02114, USA
27
Present address: Blueprint Genetics, Helsinki 00290, Finland
28
These authors contributed equally to this work
29
These authors contributed equally to this work
*Correspondence: anna-elina.lehesjoki@helsinki.fi (A.-E.L.), komatsu-ms@med.niigata-u.ac.jp (M.K.)
http://dx.doi.org/10.1016/j.ajhg.2016.06.020.
Ó 2016 American Society of Human Genetics.
3
The American Journal of Human Genetics 99, 683–694, September 1, 2016 683
�A
G
ATP
E3-ligating
enzyme
UFBP1 Adaptor
of UFL1
G
G
UFM1
G
proUFM1 GSC
UFL1
UBA5
UFC1
E1-like
enzyme
E2-like
enzyme
UFM1
UFSP2
Targets
(e.g., ASC1)
UFM1
UFM1
Specific protease
for UFM1
Targets
(e.g., ASC1)
UFSP2
AMP
Mature UFM1
(UFM1ΔC2)
Function conversion
of targets
UFM1
G
Targets
(e.g., ASC1)
B
Family A
Family B
m1=c.164G>A (p.Arg55His)
m2=c.1111G>A (p.Ala371Thr)
m1=c.855C>A (p.Tyr285Ter)
m2=c.1111G>A (p.Ala371Thr)
A-3
m1/+
+/+
A-1*
+/+
m2/+
A-2*
m1/+
+/+
A-4*
m1/+
m2/+
A-5
+/+
m2/+
A-6
m1/+
m2/+
B-3*
m1/+
m2/+
Family C
C-3
NA
B-7
+/+
+/+
c.164G>A
c.181C>T
1
5’
UBA5/NM_024818.3
c.562C>T c.855C>A
2
B-9
m1/+
+/+
B-10
m1/+
m2/+
Family E
D-3*
m1/+
m2/+
C-5
NA
B-8*
m1/+
m2/+
m1=c.562C>T (p.Arg188Ter)
m2=c.1111G>A (p.Ala371Thr)
D-2*
m1/+
+/+
D-1*
+/+
m2/+
C
D
B-6
NA
Family D
C-2*
+/+
m2/+
C-4*
m1/+
m2/+
B-2*
m1/+
+/+
B-5
NA
m1=c.181C>T (p.Arg61Ter)
m2=c.1111G>A (p.Ala371Thr)
m1=c.562C>T (p.Arg188Ter)
m2=c.1111G>A (p.Ala371Thr)
C-1*
m1/+
+/+
B-4*
m1/+
+/+
B-1*
+/+
m2/+
6
Arg55
E-1*
+/+
m2/+
E-2*
m1/+
+/+
E-3*
m1/+
m2/+
E-4
NA
c.1111G>A
9 11
12
3’
Ala371
80 85 104
127
184
150
250
364
404
UBA5
Active site
ATP binding
domain
ATP binding
pocket
E
H.
P.
B.
M.
G.
X.
D.
D.
C.
A.
sapiens
troglodytes
taurus
musculus
gallus
tropicalis
rerio
melanogaster
elegans
thaliana
Arg55
Ala371
**********
SNPYSRLMALK
SNPYSRLMALK
SNPYSRLMALK
SNPYSRLMALK
SNPYSRLMALK
SNPYSRLMALK
SNPYSRLMALK
SNPYSRLMALQ
SNPYSRLMALQ
SNPYSRLMALQ
*:
EGITVAYTIPK
EGITVAYTIPK
EGIIVAYTVPQ
EGITVAYTVPK
VGITVAYTIPN
EGIKVAYTVPI
EGITVAYTIPEGLRLAYEAPE
TGLKFAYEPIK
EGLTRELPVAD
Transthiolation
domain
Figure 1. Compound Heterozygous Variants in UBA5
(A) A schematic of the UFM1 ubiquitin-like modifier cascade. UFM1 is synthesized in a precursor form and cleaved at the C terminus by
specific protease, UFSP2.3 The E1-like enzyme UBA5 activates mature UFM1 (UFM1DC2), forming a high-energy thioester bond. The activated UFM1 is then transferred to an E2-like (conjugating) enzyme, UFC1, through a similar thioester linkage.4 Finally, UFM1 is covalently conjugated (ufmylated) with cellular proteins such as UFM1-binding protein 1 (UFBP1, official symbol DDRGK1) and a nuclear
(legend continued on next page)
684 The American Journal of Human Genetics 99, 683–694, September 1, 2016
�cancer development,5 and is implicated in cellular stress
response8–11 (UFM1 system is reviewed in Daniel and Liebau12). However, the role of the UFM1 system in the central nervous system (CNS) has not been studied, and the
mechanism by which UFM1 system executes its functions
is largely unknown.
In this study, we identified pathogenic compound heterozygous UBA5 (MIM: 610552) variants in nine affected
individuals who are from five unrelated families and
show early infantile-onset encephalopathy. Functional
analysis of the mutants suggests that reduced UBA5
activity leading to impaired UFM1 system underlies this
syndrome.
As part of a study that aimed to identify genetic causes
underlying severe infantile-onset epileptic syndromes
in 30 Finnish individuals (A.L., unpublished data), we
exome sequenced an index case (A-4) and his parents in
family A (Figure 1B). Informed consent was obtained
from the parents and the study was approved by an institutional review board at the Helsinki University Central
Hospital. Whole-exome capture (Agilent SureSelect Human All Exon 50Mb V3), sequencing (Illumina HiSeq
2000; performed at the Wellcome Trust Sanger Institute),
sequence read alignment to hs37d5 reference genome
(based on GRCh37), and variant calling (Genome Analysis Tool Kit [GATK] HaplotypeCaller v. 3.3)13–15 was
done as described previously with minor modifications.16 Given that the index case subject A-4 has an
affected sister (A-6) in family A (Figure 1B), we analyzed
the exome data of A-4 (see Table S1 for sequencing
metrics) primarily for rare (<1% allele frequency) potentially deleterious autosomal-recessive variants including
missense, nonsense, splice site, in-frame insertion and
deletion, and frameshift variants based on Variant Effect
Predictor17 annotations in CCDS genes (Ensembl release
78). We also assessed the possibility of parental mosaicism
by calling de novo variants using DeNovoGear,18 and
additionally, we analyzed heterozygous, potentially deleterious variants absent from population variant databases
separately without using the de novo variant caller. The
following databases were used to determine population
allele frequencies: the ~60,000 exomes of the Exome
Aggregation Consortium (ExAC; v.0.3),19 phase 3 release
of the 1000 Genomes project20 (2,535 individuals), and
Exome Variant Server (EVS) of the NHLBI GO Exome
Sequencing Project (v.0.0.25; 6,503 individuals). All
candidate variants were confirmed by bidirectional Sanger
sequencing, and segregation analysis was performed on
available family members.
The only variants passing the filtering under recessive
model in affected individual A-4 were compound
heterozygous missense variants c.164G>A (p.Arg55His;
affects also splicing, see below) and c.1111G>A
(p.Ala371Thr) in UBA5 (GenBank: NM_024818.3, Ensembl: ENST00000356232; Figures 1B–1E and S1A, Tables
S2 and S3). Sanger sequencing of additional family members revealed that these variants were compound heterozygous also in the affected sister but not in two unaffected
sisters (Figure 1B). Analysis for variants causing the disease
in the two siblings due to parental mosaicism did not yield
any candidate variants (data not shown).
In addition to the above-mentioned cohort of 30
affected individuals sequenced at the Wellcome Trust
Sanger Institute, we have exome sequenced and analyzed
in-house six additional families (five of which are Finnish)
with severe epileptic syndromes. One of these (family B;
Figure 1B), ascertained by clinicians (H.R., M.P., R.K.-F.,
and R.H.) at the Oulu University Hospital Finland, has
four affected individuals with clinical features similar to
the affected individuals in family A. After informed
consent was given by parents of family B, exome capture
(Nimblegen SeqCap EZ Human Exome Library v.2.0),
sequencing (Illumina HiSeq 1500; performed at the Institute for Molecular Medicine Finland), sequence read alignment to hg19 (GRCh37), and variant calling (samtools)21
was done as described previously with minor modifications.22 Exome sequencing of two affected siblings (B-3
and B-8), their parents, and one unaffected sibling (B-4) revealed compound heterozygous UBA5 variants c.855C>A
(p.Tyr285Ter) and c.1111G>A (p.Ala371Thr) in the
affected siblings (Figures 1B–1E and S1B, Tables S1–S3).
No other variants passed filtering under the recessive
model (Table S2). No candidate variants were identified
when assessing the possibility of parental mosaicism
(data not shown). Sanger sequencing of one additional
affected individual and two additional unaffected siblings
confirmed autosomal-recessive segregation of the UBA5
variants with the disease in the family (Figure 1B).
To attempt to identify additional individuals with biallelic
UBA5 variants, we used GeneMatcher website23 and accessed
data on 178 exomes or whole genomes of epileptic encephalopathy cases generated in EuroEPINOMICS Rare Epilepsy
Syndromes consortium, 455 exomes from the Northern
Finland Intellectual Disability cohort, as well as the exomes
from the UK-based Deciphering Developmental Disorders
(DDD) study.24,25 In the DDD study with more than 4,000
exome-sequenced families with developmental disorders,
of which 3,072 were without genetic diagnosis after initial
receptor coactivator, ASC1 (official symbol TRIP4) via UFL1 (E3-ligating enzyme).5,6 The conjugates are cleaved by UFSP2,3 implying the
reversibility of the UFM1 conjugating system.
(B) Pedigrees of five families with biallelic variants in UBA5. Variants present in each family are shown above the pedigrees. Exomesequenced individuals are marked with asterisks. Plus sign (þ) indicates wild-type.
(C) A schematic of the exon structure of UBA5 showing the locations of the variants.
(D) A schematic of the domain structure of UBA5 protein.
(E) ClustalX alignment of the Arg55 and Ala371 residues of UBA5 in metazoa and plants. Asterisks (*) and colons (:) indicate fully
conserved and highly conserved residues, respectively.
The American Journal of Human Genetics 99, 683–694, September 1, 2016 685
�analysis,24 we identified two unrelated individuals (C-4 of
British and D-3 of Northern Irish and Romanian ancestry;
Figure 1B) who are similarly affected to siblings in families
A and B and are compound heterozygous for rare UBA5 variants. Exome data of C-4 and D-3 did not reveal other plausible candidate variants (data not shown). Families C and
D were included in the DDD study after informed consent,
and the study has an UK Research Ethics Committee
approval (10/H0305/83 granted by the Cambridge South
REC and GEN/284/12 granted by the Republic of Ireland
REC). Both C-4 and D-3 are compound heterozygous for
the c.1111G>A (p.Ala371Thr) variant and a nonsense
variant (C-4: c.562C>T [p.Arg188Ter]; D-3: c.181C>T
[p.Arg61Ter]) (Figures 1B and S2, Table S3). Finally, within
the Northern Finland Intellectual Disability cohort, we identified one affected individual (E-3) compound heterozygous
for c.1111G>A (p.Ala371Thr) and c.562C>T (p.Arg188Ter),
the same variant combination as in C-4 (Figures 1B and S2,
Table S3).
The p.Ala371Thr substitution, present in heterozygous
state in all five families, has an allele frequency of 0.19%
in the total of approximately 60,000 individuals in the
ExAC database, 0.28% in non-Finnish Europeans, and
0.46% in Finns, with no homozygotes identified. There is
one heterozygous carrier for p.Arg55His in ExAC and two
heterozygous carriers for p.Arg188Ter in EVS, whereas
the p.Arg61Ter and p.Tyr285Ter changes are novel. The
missense substitutions occur at residues conserved down
to C. elegans (p.Ala371Thr) or A. thaliana (p.Arg55His;
Figure 1E) and are predicted to be deleterious by all four
in silico methods used (Table S3).
Because p.Ala371Thr is present at low frequency in
the general population, we assessed the probability for
observing rare (<1%) biallelic UBA5 variants in five unrelated families in the study populations. We employed a
recently established method, recessiveStats, developed as
part of the DDD study,24 in which for a given gene, the
number of unrelated cases with one of three possible biallelic genotype classes is tallied after filtering exome variant
data for rare (<1%) variants. The three biallelic genotype
classes are loss-of-function/loss-of-function, loss-of-function/functional, and functional/functional, with functional variants defined as those altering amino acid
sequence but not likely to cause complete loss of function,
e.g., missense variants. Then the probability to observe n
number of unrelated individuals with such biallelic genotypes in the study cohort is determined after calculating
the expected frequency of the genotypes based on the
summed allele frequencies of rare (<1%), functional, or
loss-of-function variants in the ExAC database (see original
publication24 for methodological details and Table S4 for
analysis details in this study). The statistical analysis was
performed separately for the three genotype classes. For
observing four independent families (B–E) with compound
heterozygous functional (p.Ala371Thr) and loss-of-function variants, we obtained a p value of 3.30 3 10 10,
strongly indicating that our datasets are enriched for
causal, compound heterozygous UBA5 variants (Table
S4). The p value remains statistically significant after
conservative correction for multiple testing for the three
genotype classes and for the total number of annotatable
protein coding genes based on GENCODE release 19
(0.05/3/17,370 ¼ 9.60 3 10 7). Notably, even though
affected siblings in family A were not tallied in the
functional/loss-of-function genotype class, they have in
effect a combination of a missense and a loss-of-function
variant, because the second UBA5 variant in this family,
c.164G>A (p.Arg55His), encodes UBA5 mutant with
severely reduced enzymatic activity and also affects
splicing (see below). Finally, to exclude the presence of
p.Ala371Thr/loss-of-function variant genotype in the general population, we have queried genotype information in
>75,000 exomes of control individuals with no severe pediatric diseases (60,706 exomes in ExAC, 10,490 Finnish
exomes of which ~7,000 are not in ExAC, and ~8,000 parents from the DDD study). In these datasets, none of the
few carriers of loss-of-function variants in UBA5 also have
p.Ala371Thr.
All affected individuals in non-consanguineous families
A–E presented in early infancy with irritability, and most
had pronounced dystonic movements (e.g., axial hyperextension, head version, tonic upward gaze deviation, and
pronation of arms and legs) and truncal hypotonia and
they later developed spasticity (Table S5). In families A, B,
C, and E, epileptic seizures, including myoclonic jerks
(family A and B) and infantile spasms (A–C), started in
infancy. Individual D-3, who is currently 5 years and
7 months of age, has not had seizures and EEG has been
normal. The affected individuals did not reach any motor
milestones and had severe intellectual disability, besides
D-3 who is considered to have moderate intellectual
deficit. The siblings in family B and individual E-3
also showed progressive growth failure. All individuals
developed progressive microcephaly, besides E-3 who
had occipito-frontal circumference of 2 SD at 9 years,
which does not reach the applied diagnostic threshold
for microcephaly of 3 SD. The affected individuals
did not share any distinctive dysmorphic features, but individuals A-4 and C-4 presented with expressionless face,
tented upper lip, long and deep philtrum, micrognathia,
and puffy hands and feet with tapering fingers
(Figure S3). Brain MRI (performed in seven individuals)
findings were subtle and included mildly delayed myelination, slight T2-hyperintensity in thalami (Figure S4),
thalamic volume reduction, and mild cerebral or cerebellar
atrophy. Four out of nine affected individuals have died at
5, 12, 16, and 21 years of age, and five, aged 3–42 years, are
alive.
All affected individuals had normal karyotype. Microarray-based analyses on individuals A-4, A-6, C-4, and D-3
had yielded inherited microdeletions or microduplications
interpreted as benign. Sequencing of the SLC16A2 (MIM:
300095) and ARX (MIM: 300382) in case A-4 had not
revealed pathogenic variants.
686 The American Journal of Human Genetics 99, 683–694, September 1, 2016
�C
UFC1
1.2
0.8
0.6
0.4
0.2
0
C1
C2
A-4
B-3
Relative mRNA
1
1.6
1.4
1.2
1
0.8
0.6
0.4
0.2
0
DTT
UFM1
1.4
+
- + -
97
1.2
1
64
51
0.8
39
0.6
28
0.4
19
Uba5-Ufm1
Ufc1-Ufm1
0.2
0
14
C1
C2
A-4
B-3
**
**
C1
C2
A-4
B-3
UBA5
Uba5-/-
Uba5+/+
A
Ufm1
Anti-UFM1
51
(kDa)
Anti-ACTIN
B
C1
C2
A-4
B-3
C1
DTT + - + - + - + -
97
64
51
UBA5-UFM1
UBA5
C2
A-4
B-3
C1
C2
A-4
B-3
DTT + - + - + - + -
DTT + - + - + - + -
97
97
64
51
64
51
39
39
28
28
UFC1-UFM1
UBA5-UFM1
39
UFC1-UFM1
28
UFC1
19
19
14
14
19
14
(kDa)
Anti-UFM1
Anti-UFC1
Anti-UBA5
UFM1
(kDa)
51
(kDa)
Anti-ACTIN
0.6
0.4
0
C1
C2
A-4
B-3
0.2
0.8
0.6
0.4
0.2
0
1.2
**
*
1
0.8
0.6
0.4
0.2
0
C1
C2
A-4
B-3
0.8
1
**
**
UFC1-UFM1/ACTIN
1
1.2
C1
C2
A-4
B-3
**
**
UBA5-UFM1/ACTIN
UBA5/ACTIN
1.2
Figure 2. Defective E1 Activity of UBA5 in Fibroblasts Derived from Subjects with Pathogenic Biallelic UBA5 Variants
(A) Quantitative real-time PCR analyses of UBA5, UFC1 (MIM: 610554) and UFM1 (MIM: 610553) in case (A-4 and B-3) and control
(C1: female, age 26; C2: female, age 43) primary skin fibroblasts. Using a Transcriptor First Strand cDNA Synthesis Kit (Roche Applied
Science), cDNA was synthesized from 1 mg of total RNA extracted from indicated fibroblasts. Quantitative PCR was performed using
LightCycler 480 Probes Master (Roche Applied Science) in a LightCycler 480 (Roche Applied Science). Signals were assessed relative
to that of GAPDH (MIM: 138400). Values were normalized to the amount of mRNA in control C1. The experiments were performed three
times. The sequences of the primers are shown in Table S7. Statistical analysis was performed using the unpaired t test (Welch test). Data
are means 5 SE. **p < 0.01.
(B and C) Immunoblot analysis of UBA5, UFC1, and UFM1 with reducing and nonreducing samples that were prepared from fibroblasts
of affected individuals and human controls (B) and mouse embryonic fibroblasts (C). Indicated fibroblasts were lysed with ice-cold TNE
buffer (10 mM Tris-HCl [pH 7.5], 1% Nonidet P-40, 150 mM NaCl, 1 mM ethylenediaminetetraacetic acid [EDTA], and protease inhibitors). Samples were prepared with NuPAGE-loading buffer in presence or absence of DTT, separated using a NuPAGE system (Life Technologies) on 4%–12% Bis-Tris gels in MOPS-SDS buffer, and then transferred to a polyvinylidene difluoride (PVDF) membrane. Mouse
(legend continued on next page)
The American Journal of Human Genetics 99, 683–694, September 1, 2016 687
�The neuropathological findings in A-4, B-5, B-8, and B10 were mild and nonspecific (data not shown). White
matter volume seemed slightly reduced and corpus callosum was somewhat thin, but no signs of an ongoing leukodystrophy could be found. Slight diffuse atrophy could
be seen in thalami, brain stem, and cerebellum. The density of especially mediodorsal and reticular neurons was
diminished in thalami, and some postnecrotic calcified
neurons were seen. In the mesencephalon there was slight
neuronal loss and vacuolization in the periaqueductal gray
matter, pontine basis was slightly thinned, and cerebelloolivary fibers were thinned in medulla oblongata. Cerebellar cortex showed slightly narrowed molecular and
granular cell layers and marginal drop-out of Purkinje cells.
Dentate nucleus harbored several pyknotic neurons. Both
the clinical features and neuropathological findings were
non-specific, resembling the pattern seen in various progressive encephalopathies.
We studied the consequence of the UBA5 variants on
RNA level in primary skin fibroblasts obtained from
affected individuals A-4 and B-3, who are both heterozygotes for the missense substitution c.1111G>A
(p.Ala371Thr). The other variant in B-3, the nonsense
variant c.855C>A (p.Tyr285Ter) in the exon 9
(Figure 1C), is predicted to result in nonsense-mediated
decay (NMD). As expected, we noted an approximately
50% reduction in UBA5 mRNA levels in B-3 fibroblasts
(Figure 2A). Sequencing of UBA5 cDNA in B-3 fibroblasts
revealed that the only allele present on RNA level is
c.1111G>A (Figure S5A). We observed an approximately
30% reduction in mRNA levels also in fibroblasts of A-4
(Figure 2A), whose other heterozygous variant is
c.164G>A. This change, which is predicted to cause the
p.Arg55His substitution, occurs in the third nucleotide
in the 50 end of exon 2 (Figure S5B) and thus possibly
affects splicing. Capillary sequencing of cDNA amplified
using primers in exons 1 and 3 implied that the minority
of sequences are from the c.164G>A mutant allele
(Figure S5B). Suggesting that the variant facilitates exon 2
skipping, RT-PCR showed a weak band whose size and
sequence corresponds to a UBA5 transcript where exon 2
is skipped (Figures S5C and S5D). This would lead to a
frameshift and consequent NMD. Confirming further
that the UBA5 allele with c.164G>A is expressed at lower
levels, cDNA sequencing of exon 11 revealed that the
majority of UBA5 mRNA has c.1111G>A (Figure S5B).
We observed that expression of not only the UBA5
mRNA but also the UBA5 protein was lower in fibroblasts of
affected individuals than of control subjects (Figure 2B). By
immunoblot analysis with non-reducing samples, we detected the intermediates of UFM1-UBA5 and of UFM1UFC1. As expected, the level of UFM1-UBA5 intermediates
was significantly lower in fibroblasts of affected individuals
compared to control subjects (Figure 2B). Likewise, the
formation of the UFM1-UFC1 intermediate declined
(Figure 2B). Surprisingly, UFM1 conjugates were hardly detected in human fibroblasts regardless of the genotypes
(Figure 2B). We confirmed a similar pattern in mouse
embryonic fibroblasts (Figure 2C).
To test whether the missense variants affect the E1-like
activity of UBA5 in cells, we used a UBA5 mutant in which
the active site, cysteine (Cys250), was substituted with
serine (termed UBA5Cys250Ser). When the cysteine residue
at the active site of E1 and E2 enzymes is replaced with
serine, an O-ester bond instead of a thioester bond is
formed with its respective modifier proteins, and the intermediates become stable even under reducing conditions.4
In addition, to exclude the effect of endogenous UBA5,
UBA5 in HEK293T cells was deleted by CRISPR/Cas9 technology (Figures 3A and S6). We expressed a FLAG-tagged
UBA5Cys250Ser (FLAG-UBA5Cys250Ser) together with MYCtagged UFM1DC2, a mature form of UFM1 with the glycine
residue at the C terminus (Figure 1A), in UBA5-deficient
HEK293T cells, and analyzed the cell lysates by immunoblot assay. An intermediate between FLAG-UBA5Cys250Ser
and MYC-UFM1DC2 was clearly recognized (Figure 3A).
We next analyzed UBA5 constructs carrying both
p.Cys250Ser and one of the missense variants observed
in affected individuals (FLAG-UBA5Arg55His/Cys250Ser or
FLAG-UBA5Ala371Thr/Cys250Ser). FLAG-UBA5Arg55His/Cys250Ser
had lower ability to form the intermediate with MYCUFM1DC2 than UBA5Cys250Ser (Figure 3A). With FLAGUBA5Ala371Thr/Cys250Ser, we did not observe a statistically
significant decrease in the intermediate formation
(Figure 3A). Next, we examined the effect of UBA5 mutants
on transferring the activated UFM1 to the E2 enzyme
UFC1 (see Figure 1A) because the Ala371 residue is located
within the C-terminal transthiolation domain critical for
the transfer of UFM1 to UFC1 (Figure 1D).26 We detected
the intermediate between FLAG-UFC1Cys116Ser and MYCUFM1DC2 when wild-type UBA5 was expressed in
UBA5 / HEK293T cells (Figure 3B). By contrast, in the
case of expressing either UBA5Arg55His or UBA5Ala371Thr
mutant, formation of such intermediates was suppressed
(Figure 3B).
In good agreement with these results, in vitro thioester
formation assay with recombinant proteins revealed the
decreased E1 activity of UBA5Arg55His and UBA5Ala371Thr
monoclonal anti-actin antibody (Chemicon International cat# MAB1501R), rabbit monoclonal anti-UFM1 antibody (Abcam cat#
ab109305, RRID: AB_10864675), anti-UBA5 antibody,4 and anti-UFC1 antibody4 were used for immunodetection. The immunoreactive
bands were detected by LAS-4000 (GE Healthcare UK). In the cases of samples prepared without DTT, the intermediates corresponding to
UBA5-UFM1 and UFC1-UFM1 were clearly detected. Bar graphs indicate the quantitative densitometric analyses using Multi Gauge
Version 3.2 Image software (Fuji Film) of UBA5, UBA5-UFM1, and UFC1-UFM1 intermediates relative to ACTIN.
Statistical analysis was performed using the unpaired t test (Welch test). The data represent the means 5 SE of five separate experiments.
*p < 0.05 and **p < 0.01.
688 The American Journal of Human Genetics 99, 683–694, September 1, 2016
�Crude
wt
+
-
+
-
+
-
r
Th
is
wt
+
+
+
+
-
71
5H
97
+
+
-
+
+
+
+
+
+
-
+
+
64
64
FLAG-UBA5MYC-UFM1ΔC2
51
FLAG-UBA5
51
FLAG-UFC1MYC-UFM1ΔC2
39
28
FLAG-UFC1
Ar
FLAG-UBA5Cys250Serg
MYC-UFM1ΔC2 /ACTIN
Al 55H Cy
a3 is s2
71 /C 50
Th ys Se
r/C 25 r
ys 0Se
25 r
0S
er
1.2
*
19
1
19
MYC-UFM1ΔC2 /ACTIN
28
FLAG-UFC1Cys116Ser-
39
0.8
14
0.6
Anti-FLAG
0.4
51
Anti-FLAG
0.2
Ar
g
C 55H
ys is
Al 250
a3 A
71 la
Th
r
Anti-ACTIN
C
wt wt
+ + +
- + +
+
+
D
UBA5 wt wt
UFC1 + + +
+
+
51
0
UFM1ΔC2 + +
ATP - +
97
(kDa)
Ar
g5
C 5H
ys is
2
Al 50
a3 Al
71 a
Th
r
+
+
+
+
+
+
+
+
Anti-ACTIN
E
UBA5 +/+ -/- -/UFSP2 +/+ +/+ -/- MYC-UBA5 - FLAG-UFM1ΔC2 - MYC-UFL1 - UFBP1-MYC 188
97
1.2
**
1
0.8
0.6
0.4
0.2
0
wt
Ar
g
Al 55H
a3 is
71
Th
r
(kDa)
UBA5
UFM1ΔC2
ATP
-
a3
MYC-UBA5
MYC-UFM1ΔC2 +
FLAG-UFC1 +
FLAG-UFC1Cys116Ser -
+
g5
+
Al
-
Ar
25
0S
A e
C rg r
ys 55
25 H
0 is
A Se /
C la3 r
ys 7
25 1T
0S hr
er /
-
Crude
ys
FLAG-UBA5
MYC-UFM1ΔC2
B
C
A
-/+/+
+
+
+
+
-/-/+
+
+
+
98
64
64
UBA5-UFM1ΔC2
51
64
51
39
UBA5-UFM1ΔC2
UBA5
51
UBA5
39
28
39
28
28
19
14
19
UFM1ΔC2
(kDa)
FLAG-UFM1ΔC2conjugates
UFC1-UFM1ΔC2
19
UFC1
14
14
FLAG-UFM1ΔC2
Endo. UFM1
UFM1ΔC2
(kDa)
Anti-UFM1
51
(kDa)
- - wt
- + + +
- + + +
- + + +
MYC-UBA5
FLAG-UFM1ΔC2
MYC-UFL1
UFBP1-MYC
+
+
+
188
-
+
+
+
wt
+ + +
+ + +
+ + +
188
98
FLAG-UFM1ΔC2
Endo. UFM1
Anti-UFM1
51
39
28
0.6
19
0.4
14
0.2
0
wt
Anti-UFBP1
1.2
***
*
1
0.8
0.6
0.4
0.2
0
wt
g
Al 55H
a3 is
71
Th
r
14
FLAG-UFM1ΔC2
-UFBP1-MYC
UFBP1-MYC
Endo. UFBP1
Ar
19
64
51
0.8
g5
5
a3 His
71
Th
r
28
1
Ar
39
p=0.056
**
1.2
Al
FLAG-UFM1ΔC2
-conjugates
FLAG-UFM1ΔC2 conjugates
/ACTIN
98
64
51
(kDa)
-
FLAG-UFM1ΔC2- UFBP1-MYC
/ACTIN
-
g
Al 55H
a3 is
71
Th
r
MYC-UBA5
FLAG-UFM1ΔC2
MYC-UFL1
UFBP1-MYC
UBA5 +/+ -/- -/- -/- -/- -/UFSP2 +/+ -/- -/- -/- -/- -/-
Ar
G
UBA5 +/+ -/- -/- -/- -/- -/UFSP2 +/+ -/- -/- -/- -/- -/-
Ar
g
Al 5 5 H
a3 i s
71
Th
r
F
Anti-ACTIN
Anti-ACTIN
Figure 3. Impaired Function of UBA5 Mutants
(A and B) Immunoblot assay of UBA5 mutant p.Cys250Ser and double mutants p.Arg55His/p.Cys250Ser and p.Ala371Thr/p.Cys250Ser
in UBA5 / HEK293T cells. Indicated constructs (0.1 mg for UBA5, 0.5 mg for UFC1, and 2 mg for UFM1DC2) were expressed in UBA5-deficient HEK293T cells. 24 hr after transfection, the cell lysates were subjected to immunoblot analysis with indicated antibodies as
described in Figure 2B. Bar graphs indicate the quantitative densitometric analyses of UBA5-UFM1 and UFC1-UFM1 intermediates
(legend continued on next page)
The American Journal of Human Genetics 99, 683–694, September 1, 2016 689
�mutants. As shown in Figure 3C, the UBA5-UFM1DC2 intermediate was formed in an ATP-dependent manner
in vitro. Although both mutants still had ability to form
the intermediate, their activity was weaker compared to
that of wild-type UBA5 (Figure 3C). In addition, the
UBA5Arg55His and UBA5Ala371Thr mutants failed to transfer
the activated UFM1 to UFC1 in the initial stage of reaction
(Figure 3D). In vitro kinetics analysis of multiple time
points up to 60 min of reaction revealed that the UFC1UFM1DC2 intermediate was formed in the case of both
mutants, but that, compared to wild-type UBA5, their
reaction rates were slower (Figure S7). Whereas the activity
of UBA5Arg55His was approximately half of that with wildtype UBA5, UBA5Ala371Thr had approximately 70%–80%
activity (Figure S7).
Finally, we examined whether UBA5Arg55His and
UBA5Ala371Thr mutants suppress the UFM1 conjugate formation in cells. HEK293T cells deficient for both UBA5
and UFSP2, of which latter is the unique de-conjugating
enzyme for UFM1 conjugates (see Figure 1A), were generated by CRISPR/Cas9 technology (UBA5 / ;UFSP2 / ;
Figure S8). As shown in Figure 3E, only a few UFM1 conjugates were detected when we expressed E3-ligating enzyme
UFL1, its adaptor protein UFBP15 (see Figure 1A), and
UFM1DC2 together with wild-type UBA5 in single
knockout UBA5 / HEK293T cells. Remarkably, concomitant loss of the de-conjugating enzyme UFSP2 dramatically
increased both number and amount of UFM1 conjugates
in the UBA5-deficient HEK293T cells, indicating that
most UFM1 conjugates are de-conjugated by UFSP2. We
next evaluated the effect of UBA5 mutants (p.Arg55His
or p.Ala371Thr) in this experimental setting. The
UFM1 conjugate formation in the UBA5 / ;UFSP2 /
double knock-out (DKO) cells expressing UBA5Arg55His
was markedly suppressed (Figure 3F) (p ¼ 0.002; ratio of
actin-normalized quantity of UFM1 conjugates with
UBA5Arg55His to that with wild-type: 0.77, with 95% CI
0.72–0.82), whereas UBA5Ala371Thr only showed suggestive
decrease (p ¼ 0.056; ratio of actin-normalized quantity of
UFM1 conjugates with UBA5Ala371Thr to that with wildtype: 0.91, with 95% CI 0.79–1.02) (Figure 3F). Because
ufmylation of UFBP1 is required for its tight binding to
UFL1 and in turn for promotion of the E3 ligase activity,5
we further examined the level of the UFM1-UFBP1
conjugate in the DKO cells. We found that the conjugate
formation was impaired in both DKO cells expressing
either UBA5Arg55His (p ¼ 0.0005; ratio of actin-normalized
quantity of UFM1-UFBP1 conjugate with UBA5Arg55His to
that with wild-type: 0.76, with 95% CI 0.70–0.82) or
UBA5Ala371Thr (p ¼ 0.013; ratio of actin-normalized quantity of UFM1-UFBP1 conjugate with UBA5Ala371Thr to that
with wild-type: 0.86, with 95% CI 0.79–0.93) (Figure 3G).
Taken together, we conclude that the UBA5 mutants
exhibit decreased E1 activity with attenuated ability to
transfer the activated UFM1 to UFC1, which might cause
impaired UFM1 conjugate formation, with p.Arg55His exhibiting more pronounced defects.
Germline Uba57 or Ufm1 (M.K., unpublished data)
knockout is embryonic lethal in mice. We generated conditional knockout mice for Ufm1 (Ufm1f/f) and crossed
them with transgenic mice expressing Cre recombinase
under the control of the nestin promoter27 (nestin-Cre)
to create CNS-specific Ufm1 knockout (Ufm1f/f;nestinCre) mice (Figure S9). The Ufm1f/f;nestin-Cre mice
allowed us to examine the neuronal pathology associated
with deficiency of the UFM1 system in vivo. At embryonic
day (E) 14.5, UFM1 protein was almost absent in brain of
Ufm1f/f;nestin-Cre but not of control (Ufm1f/þ;nestin-Cre)
relative to ACTIN. Statistical analysis was performed using the unpaired t test (Welch test). The data represent the means 5 SE of four
separate experiments. *p < 0.05 and **p < 0.01.
(C and D) In vitro thioester formation assay of UFM1 by UBA5 (C) and of UFM1 by UFC1 (D). Recombinant GST-UFM1DC2, GST-UFC1,
and GST-UBA5, as well as UBA5 mutants p.Arg55His (GST-UBA5Arg55His), p.Ala371Thr (GST-UBA5Ala371Thr), and p.Cys250Ala (negative
control; GST-UBA5Cys250Ala) were produced in E. coli and the recombinant proteins were purified by chromatography on Glutathione
Sepharose 4B (GE Healthcare UK). After digestion of GST by PreScission Protease (GE Healthcare UK), the recombinant proteins were
dialyzed against 50 mM BisTris (pH 6.5), 100 mM NaCl, 10 mM MgCl2, and 0.1 mM DTT (reaction buffer). Most thioester formation
reactions contained reaction buffer with 0.8 mg UFM1DC2 and some of the following: 5 mM ATP, 0.08 (for UFC1-UFM1 thioester formation assay) or 0.8 (for UBA5-UFM1 thioester formation assay) mg UBA5 or UBA5 mutants, and 0.8 mg UFC1. Reactions were incubated for
5 min at 25� C and stopped by the addition of NuPAGE-loading buffer lacking reducing agent, followed by 10 min incubation at 37� C,
NuPAGE (4%–12% acrylamide gradient), and Coomassie brilliant blue staining. Data shown are representative of three separate
experiments.
(E) Immunoblot assay to detect UFM1 conjugates. MYC-UBA5 (0.1 mg) was expressed in combination with indicated constructs (each
1 mg) in UBA5-deficient or UBA5-UFSP2 double-deficient HEK293T cells. Cells were lysed by 200 mL of TNE, and the lysate was then centrifuged at 10,000 3 g for 10 min at 4� C to remove debris. The supernatant was subjected to immunoblot analyses with indicated
antibodies.
(F) Immunoblot assay to study the effect of UBA5 mutants on UFM1 conjugate formation. MYC-UBA5 or MYC-UBA5 mutants (0.1 mg)
were expressed in combination with indicated constructs (each 1 mg) in UBA5-UFSP2 double-deficient HEK293T cells. Cells were lysed by
200 mL of TNE, and the lysate was then centrifuged at 10,000 3 g for 10 min at 4� C to remove debris. The supernatant was subjected to
immunoblot analyses with indicated antibodies. Bar graph indicates the quantitative densitometric analyses of FLAG-UFM1 conjugates
relative to ACTIN. Statistical analysis was performed using the unpaired t test (Welch test). The data represent the means 5 SE of six
separate experiments. *p < 0.05.
(G) Immunoblot assay to study the effect of UBA5 mutants on UFM1-UFBP1 conjugate formation. Transfection and subsequent immunoblot analysis were conducted as shown in (F). Bar graph indicates the quantitative densitometric analyses of FLAG-UFM1-UFBP1-MYC
relative to ACTIN. Rabbit polyclonal anti-UFBP1 antibody6 was used for immunodetection. Statistical analysis was performed using the
unpaired t test (Welch test). The data represent the means 5 SE of six separate experiments. *p < 0.05 and ***p < 0.001.
690 The American Journal of Human Genetics 99, 683–694, September 1, 2016
�re
re
-C
-C
1 f/f
;n
es
tin
es
tin
1 f/+
;n
B
U
fm
U
fm
1 f/f
U
fm
1 f/+
U
fm
A
0
Ufm1
Relative length of sagittal axis
0.2 0.4 0.6 0.8 1.0 1.2 1.4
f/f
Ufm1f/+
191
97
64
51
Conjugate
Uba5Ufm1
39
Conjugate
Ufc1Ufm1
28
Ufm1f/f
*
Ufm1f/+; nestin-Cre
Ufm1f/f; nestin-Cre
Ufm1f/f; nestin-Cre
19
0
Relative length of coronal axis
0.2 0.4 0.6 0.8 1.0 1.2 1.4
Ufm1f/+
14
Ufm1f/f
Ufm1
***
Anti-UFM1
Ufm1f/+; nestin-Cre
51
Ufm1f/f; nestin-Cre
(kDa)
Anti-ACTIN
C
D
*
No. of cleaved caspase-3+ cells
/mm2 in occipital cortex
100
90
80
70
60
50
40
30
20
10
0
E
Cleaved caspase-3
βIII-Tubulin
Ctrl
cKO
Merged
Figure 4. Loss of UFM1 in Central Nervous System Causes Microcephaly
(A) Immunoblot analysis of UFM1 in mice with indicated genotypes. Mice were delivered by caesarean section at E18.5, and then mouse
brains were homogenized in 0.25 M sucrose, 10 mM 2-[4-(2-hydroxyethyl)-1-piperazinyl]ethanesulfonic acid (HEPES) (pH 7.4), and
(legend continued on next page)
The American Journal of Human Genetics 99, 683–694, September 1, 2016 691
�mice (Figure S10). Although a few UFM1 conjugates were
detected in brains of control mice by immunoblotting
with an anti-UFM1 antibody at E18.5, they were weak or
undetectable in brains of mutant mice (Figure 4A). These
results indicate impairment of the UFM1 conjugation system in the CNS of Ufm1f/f;nestin-Cre mice. Ufm1f/f;nestinCre mice were viable at birth and indistinguishable in
appearance from their littermates. However, all Ufm1f/f;
nestin-Cre mice died within 1 day of birth (Table S6).
Macroscopic anatomical analysis of the brains of mice
that were delivered by Caesarean section at E18.5 revealed
that Ufm1f/f;nestin-Cre mice had microcephaly (Figure 4B).
Both transverse and longitudinal distances in the mutant
brains were significantly shorter than those of control
brains (Figure 4B). Histological analysis using Karachi’s hematoxylin and eosin staining showed that some parts of
the brain, such as the occipital region of neopallium,
midbrain, and thalamus, of Ufm1f/f;nestin-Cre mice
were consistently smaller than those of control mice
(Figure 4C). However, no apparent abnormality in cellular
organization was found in the mutant brain. To examine
whether loss of UFM1 causes cell death, we carried out
immunohistochemical analysis using an antibody against
cleaved Caspase-3, a hallmark of apoptosis. A marked
increase in the number of cleaved Caspase-3-positive cells
was noted in the occipital region of neopallium in the
Ufm1f/f;nestin-Cre mice at E18.5 (Figure 4D), compared
with control mice. Double immunofluorescence analysis
with antibodies against bIII Tubulin, a neuronal marker,
and cleaved Caspase-3 revealed that neurons underwent
apoptosis (Figure 4E). We hardly detected such apoptotic
cells in other brain regions of Ufm1f/f;nestin-Cre mice at
E18.5 (data not shown). Taken together, findings in
the Ufm1f/f;nestin-Cre mice suggest that an intact
UFM1 system is pivotal for neuronal development and
survival.
Here, we combined genetic, statistical, phenotypic,
and functional data to show that the hypomorphic
p.Ala371Thr variant in trans with a loss-of-function
change in UBA5 causes a severe, early-onset encephalopathy. The likelihood for observing biallelic missense/lossof-function UBA5 variants only by chance in the assessed
disease cohorts was determined to be negligible. The
assessment of UBA5 in fibroblasts of the affected individuals and the biochemical analyses with mutant UBA5 proteins corresponding to the two missense variants indicated
that the compound heterozygous status in the affected individuals is not accompanied by a complete loss of UBA5
function. The p.Ala371Thr variant, which is present in
all five families with altogether nine affected individuals,
encodes UBA5 with only mildly reduced enzymatic activity. In contrast, the impact of the c.164G>A (p.Arg55His)
variant on UBA5 function in family A is more pronounced.
This variant is causing aberrant splicing, but this effect
does not appear to be complete in cells of the affected individuals. However, given the low enzymatic activity of
p.Arg55His UBA5 mutant protein, the function of UBA5
can be predicted to be severely compromised from this
allele also when the gene is normally spliced. The
nonsense variant p.Tyr285Ter in family B seems to undergo NMD based on analysis of UBA5 mRNA expression
and is thus likely to result in severely compromised enzymatic activity. It is likely that the gene product is degraded
also in individuals C-4, D-3, and E-3 with nonsense variants. Thus, the affected individuals seem to have one
variant with a major and one with a milder, hypomorphic
effect on UBA5 function. It is plausible that biallelic, complete loss-of-function variants in UBA5 would not be
compatible with life as observed in the Uba5 / mice.7
Interestingly, the p.Ala371Thr variant with only mildly
compromised UBA5 activity is present in considerable frequencies in Finns (0.46% allele frequency in ExAC) and
1 mM dithiothreitol (DTT). The homogenates were subjected to immunoblot analysis with indicated antibodies. Samples prepared from
three mice with indicated genotype were loaded.
(B) A dorsal view of brains of Ufm1f/f and Ufm1f/f;nestin-Cre mice delivered by Caesarean section at E18.5. Graphs show axial distance
(from the anterior edge of cerebrum to posterior edge of mid brain) and maximal lateral distance of brains of indicated genotype
mice. Data presented as mean 5 SE of Ufm1f/þ (n ¼ 4), Ufm1f/f (n ¼ 4), Ufm1f/þ;nestin-Cre (n ¼ 5), and Ufm1f/f;nestin-Cre (n ¼ 6).
Statistical analysis was performed using the unpaired t test. *p < 0.05 and ***p < 0.001.
(C) Histological analyses of brains of Ufm1f/þ;nestin-Cre (Ctrl) and Ufm1f/f;nestin-Cre (cKO) mice. Embryos at E18.5 were delivered by
Caesarean section, and their heads were fixed by immersion in 0.1 M phosphate buffer (pH 7.4) containing 4% paraformaldehyde
and 4% sucrose. Each brain was carefully dissected and processed for paraffin embedding, and then 3 mm sagittal sections were prepared
for haematoxylin and eosin staining. Images were captured with BZ-9000 (Keyence) and BX51 microscopes (Olympus). Boxed regions a
and b in the neopallium are magnified and shown on the right as indicated. Note that the occipital region (b) of neopallium in the
mutant brain is thinner than that in control, while the difference in the parietal region (a) is less apparent. Scale bars are 2 mm and
0.1 mm. Abbreviations are as follows: Np, neopallium; Mb, midbrain; Th, thalamus; IZ, intermediate zone; CP, cortical plate.
(D) Apoptotic cells in the occipital region of neopallium of Ufm1f/þ;nestin-Cre (Ctrl) and Ufm1f/f; nestin-Cre (cKO) mice at E18.5. Sections
prepared as described in (C) were immunostained by rabbit polyclonal anti-cleaved caspase-3 antibody (Cell Signaling Technology [CST]
cat# 9661, RRID: AB_2314091; 1:500) as described previously.28 Images were captured with BX53 microscope (Olympus). Each inset is a
magnified image. Scale bars represent 100 mm. For quantification, the number of cleaved caspase-3-positive cells per unit area was calculated in each occipital cortex, which was defined as the cerebral cortex located posterior to the hippocampus. Statistical analysis was
performed using the unpaired t test (n ¼ 3 animals for each group). Data represent the means 5 SE. *p < 0.05. The area was measured
by NIH Image/ImageJ.
(E) Double-immunofluorescence analysis. Section of cKO brain (occipital region of neopallium) prepared as described in (C) was doubleimmunostained with anti-cleaved-caspase-3, mouse monoclonal anti-bIII Tubulin antibody (clone 5G8, Promega, 1:1,000), goat antimouse Alexa Fluor 594, and goat anti-rabbit Alexa Fluor 488 (Molecular Probes, 1:1,000). Images were captured with confocal
FV1200 microscope (Olympus). Scale bar represents 20 mm.
692 The American Journal of Human Genetics 99, 683–694, September 1, 2016
�other Europeans (0.28%). This implies that the syndrome
associated with deficient UBA5 function should be
encountered in the European population. Indeed, in addition to the five families identified in this study, individuals
from two families of European ancestry with biallelic compound heterozygous variants in UBA5 and a disease manifestation comparable to the affected individuals in our
study have the p.Ala371Thr variant in combination with
a loss-of-function UBA5 variant (D. Bonneau, personal
communication).
Notably, given its relatively mild effect on UBA5 function, the phenotypic consequences of p.Ala371Thr when
occurring in homozygosity could be predicted to be mild.
To search for individuals homozygous for p.Ala371Thr
(no homozygotes were present in the databases used in
exome data filtering, see above), we queried ~10,490
exomes from various Finnish population-based and disease
cohorts (see SISu in Web Resources). In the exome data
from the FINRISK cohort,29 we identified one homozygous
individual (V. Salomaa, personal communication) who is
in his fifties and, based on data gathered from National
Health registers, does not have any hospitalizations or
chronic medication for any neurological or neuropsychiatric diseases. This observation suggests that, as described
in this paper, p.Ala371Thr indeed contributes to a severe
neurological phenotype only when it is in trans with a severe loss-of-function variant. This observation also has
relevance for filtering strategies of exome variant data,
because it exemplifies that homozygosity for a relatively
rare missense variant in ‘‘control’’ individuals does not
necessarily mean non-pathogenicity. During the review
of this paper, Duan and colleagues reported a family with
two siblings with compound heterozygous variants in
UBA5 (p.Lys310Glu and p.Arg246Ter) and a childhoodonset neurological disease with ataxia as the primary
symptom.30 Altogether, the existing data on different combinations of biallelic UBA5 variants both in humans and in
mouse models suggest that the phenotypic consequences
range from embryonic lethality (biallelic loss-of-function
in knockout mice), severe infantile-onset encephalopathy
(this study), childhood-onset neurological disease (Duan
et al.30), to possibly no or very mild phenotype.
The symptoms in individuals with biallelic UBA5
variants are predominantly related to CNS. Previously,
however, we and other groups have reported the function
of the ubiquitously expressed UFM1 system outside the
CNS.5,7–11 For example, mice with a germline deletion
of Uba5,7 Ufm1 (M.K., unpublished data), or Ddrgk1
(Ufbp1)8 are embryonic lethal and show a severe defect of
erythroid differentiation. The affected individuals in our
study, with partial loss of UBA5 function, do not present
with anemia, suggesting that the remaining UBA5 activity
is sufficient for normal hematopoiesis. Finally, to further
support the role of UFM1 system beyond CNS, a suggestive
association of a UFSP2 (MIM: 611482; UFM1-specific
peptidase) variant with Beukes hip dysplasia was recently
established.31
Consistent with imaging and neuropathological observations in affected individuals, the analysis of CNS-specific
Ufm1 knockout mice revealed that dysfunction of the
UFM1 system causes atrophy in several regions of the brain
and results in neonatal death. Our data imply compromised UFM1 conjugate formation in the brains of the
CNS-specific Ufm1 knockout mice with neuronal apoptosis
in restricted regions (i.e., the occipital region of neopallium). Therefore it is possible that spatiotemporally regulated and cell-specific ufmylation is necessary not only
for prevention of neuronal cell death but also for neuronal
development. Further studies assessing the specific function of UFM1 conjugation to its target proteins in CNS
and elsewhere are warranted.
Accession Numbers
The raw aligned sequence reads of family A were submitted to the
European Genome-phenome Archive by Wellcome Trust Sanger
Institute under study accession IDs EGAS00001000190 and
EGAS00001000386. Exome sequencing data from the DDD study
are downloadable under study accession ID EGAS00001000775.
Supplemental Data
Supplemental Data include ten figures, seven tables, and Supplemental Acknowledgments and can be found with this article online at http://dx.doi.org/10.1016/j.ajhg.2016.06.020.
Received: January 26, 2016
Accepted: June 22, 2016
Published: August 18, 2016
Web Resources
1000 Genomes, http://www.1000genomes.org
Clustal: Multiple Sequence Alignment, http://www.clustal.org/
European Genome-phenome Archive (EGA), https://www.ebi.ac.
uk/ega
ExAC Browser, http://exac.broadinstitute.org/
GATK, https://www.broadinstitute.org/gatk/
GenBank, http://www.ncbi.nlm.nih.gov/genbank/
NHLBI Exome Sequencing Project (ESP) Exome Variant Server,
http://evs.gs.washington.edu/EVS/
OMIM, http://www.omim.org/
RRID, https://scicrunch.org/resources
SISu Project, www.sisuproject.fi
Variant Effect Predictor, http://useast.ensembl.org/Homo_sapiens/
Tools/VEP
References
1. van der Veen, A.G., and Ploegh, H.L. (2012). Ubiquitin-like
proteins. Annu. Rev. Biochem. 81, 323–357.
2. Schulman, B.A., and Harper, J.W. (2009). Ubiquitin-like protein activation by E1 enzymes: the apex for downstream signalling pathways. Nat. Rev. Mol. Cell Biol. 10, 319–331.
3. Kang, S.H., Kim, G.R., Seong, M., Baek, S.H., Seol, J.H., Bang,
O.S., Ovaa, H., Tatsumi, K., Komatsu, M., Tanaka, K., and
Chung, C.H. (2007). Two novel ubiquitin-fold modifier 1
The American Journal of Human Genetics 99, 683–694, September 1, 2016 693
�4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
(Ufm1)-specific proteases, UfSP1 and UfSP2. J. Biol. Chem.
282, 5256–5262.
Komatsu, M., Chiba, T., Tatsumi, K., Iemura, S., Tanida, I.,
Okazaki, N., Ueno, T., Kominami, E., Natsume, T., and Tanaka,
K. (2004). A novel protein-conjugating system for Ufm1, a
ubiquitin-fold modifier. EMBO J. 23, 1977–1986.
Yoo, H.M., Kang, S.H., Kim, J.Y., Lee, J.E., Seong, M.W., Lee, S.W.,
Ka, S.H., Sou, Y.S., Komatsu, M., Tanaka, K., et al. (2014). Modification of ASC1 by UFM1 is crucial for ERa transactivation and
breast cancer development. Mol. Cell 56, 261–274.
Tatsumi, K., Sou, Y.S., Tada, N., Nakamura, E., Iemura, S., Natsume, T., Kang, S.H., Chung, C.H., Kasahara, M., Kominami,
E., et al. (2010). A novel type of E3 ligase for the Ufm1 conjugation system. J. Biol. Chem. 285, 5417–5427.
Tatsumi, K., Yamamoto-Mukai, H., Shimizu, R., Waguri, S., Sou,
Y.-S., Sakamoto, A., Taya, C., Shitara, H., Hara, T., Chung, C.H.,
et al. (2011). The Ufm1-activating enzyme Uba5 is indispensable for erythroid differentiation in mice. Nat. Commun. 2, 181.
Cai, Y., Pi, W., Sivaprakasam, S., Zhu, X., Zhang, M., Chen, J.,
Makala, L., Lu, C., Wu, J., Teng, Y., et al. (2015). UFBP1, a key
component of the Ufm1 conjugation system, is essential for
ufmylation-mediated regulation of erythroid development.
PLoS Genet. 11, e1005643.
Hertel, P., Daniel, J., Stegehake, D., Vaupel, H., Kailayangiri, S.,
Gruel, C., Woltersdorf, C., and Liebau, E. (2013). The ubiquitin-fold modifier 1 (Ufm1) cascade of Caenorhabditis elegans.
J. Biol. Chem. 288, 10661–10671.
Lemaire, K., Moura, R.F., Granvik, M., Igoillo-Esteve, M., Hohmeier, H.E., Hendrickx, N., Newgard, C.B., Waelkens, E.,
Cnop, M., and Schuit, F. (2011). Ubiquitin fold modifier 1
(UFM1) and its target UFBP1 protect pancreatic beta cells
from ER stress-induced apoptosis. PLoS ONE 6, e18517.
Zhang, Y., Zhang, M., Wu, J., Lei, G., and Li, H. (2012). Transcriptional regulation of the Ufm1 conjugation system in
response to disturbance of the endoplasmic reticulum homeostasis and inhibition of vesicle trafficking. PLoS ONE 7, e48587.
Daniel, J., and Liebau, E. (2014). The ufm1 cascade. Cells 3,
627–638.
McKenna, A., Hanna, M., Banks, E., Sivachenko, A., Cibulskis,
K., Kernytsky, A., Garimella, K., Altshuler, D., Gabriel, S., Daly,
M., and DePristo, M.A. (2010). The Genome Analysis Toolkit:
a MapReduce framework for analyzing next-generation DNA
sequencing data. Genome Res. 20, 1297–1303.
Van der Auwera, G.A., Carneiro, M.O., Hartl, C., Poplin, R.,
Del Angel, G., Levy-Moonshine, A., Jordan, T., Shakir, K.,
Roazen, D., Thibault, J., et al. (2013). From FastQ data to
high confidence variant calls: the Genome Analysis Toolkit
best practices pipeline. Curr. Protoc. Bioinformatics 43, 1–33.
DePristo, M.A., Banks, E., Poplin, R., Garimella, K.V., Maguire,
J.R., Hartl, C., Philippakis, A.A., del Angel, G., Rivas, M.A.,
Hanna, M., et al. (2011). A framework for variation discovery
and genotyping using next-generation DNA sequencing data.
Nat. Genet. 43, 491–498.
Muona, M., Berkovic, S.F., Dibbens, L.M., Oliver, K.L., Maljevic, S., Bayly, M.A., Joensuu, T., Canafoglia, L., Franceschetti,
S., Michelucci, R., et al. (2015). A recurrent de novo mutation
in KCNC1 causes progressive myoclonus epilepsy. Nat. Genet.
47, 39–46.
McLaren, W., Pritchard, B., Rios, D., Chen, Y., Flicek, P., and
Cunningham, F. (2010). Deriving the consequences of
genomic variants with the Ensembl API and SNP Effect Predictor. Bioinformatics 26, 2069–2070.
18. Ramu, A., Noordam, M.J., Schwartz, R.S., Wuster, A., Hurles,
M.E., Cartwright, R.A., and Conrad, D.F. (2013). DeNovoGear:
de novo indel and point mutation discovery and phasing. Nat.
Methods 10, 985–987.
19. Lek, M., Karczewski, K., Minikel, E., Samocha, K., Banks, E.,
Fennell, T., O’Donnell-Luria, A., Ware, J., Hill, A., Cummings,
B., et al. (2015). Analysis of protein-coding genetic variation in 60,706 humans. bioRxiv http://dx.doi.org/10.1101/
030338.
20. Abecasis, G.R., Auton, A., Brooks, L.D., DePristo, M.A., Durbin, R.M., Handsaker, R.E., Kang, H.M., Marth, G.T., and
McVean, G.A.; 1000 Genomes Project Consortium (2012).
An integrated map of genetic variation from 1,092 human
genomes. Nature 491, 56–65.
21. Li, H., Handsaker, B., Wysoker, A., Fennell, T., Ruan, J., Homer,
N., Marth, G., Abecasis, G., Durbin, R., and Subgroup,
G.P.D.P.; 1000 Genome Project Data Processing Subgroup
(2009). The Sequence Alignment/Map format and SAMtools.
Bioinformatics 25, 2078–2079.
22. Sulonen, A.-M., Ellonen, P., Almusa, H., Lepistö, M., Eldfors,
S., Hannula, S., Miettinen, T., Tyynismaa, H., Salo, P., Heckman, C., et al. (2011). Comparison of solution-based exome
capture methods for next generation sequencing. Genome
Biol. 12, R94.
23. Sobreira, N., Schiettecatte, F., Valle, D., and Hamosh, A.
(2015). GeneMatcher: a matching tool for connecting investigators with an interest in the same gene. Hum. Mutat. 36,
928–930.
24. Akawi, N., McRae, J., Ansari, M., Balasubramanian, M., Blyth,
M., Brady, A.F., Clayton, S., Cole, T., Deshpande, C., Fitzgerald,
T.W., et al.; DDD study (2015). Discovery of four recessive developmental disorders using probabilistic genotype and phenotype
matching among 4,125 families. Nat. Genet. 47, 1363–1369.
25. Deciphering Developmental Disorders Study (2015). Largescale discovery of novel genetic causes of developmental disorders. Nature 519, 223–228.
26. Xie, S. (2014). Characterization, crystallization and preliminary X-ray crystallographic analysis of the human Uba5 C-terminus-Ufc1 complex. Acta Crystallograph. Sect. F Struct. Biol.
Cryst. Commun. 70, 1093–1097.
27. Tronche, F., Kellendonk, C., Kretz, O., Gass, P., Anlag, K.,
Orban, P.C., Bock, R., Klein, R., and Schütz, G. (1999). Disruption of the glucocorticoid receptor gene in the nervous system
results in reduced anxiety. Nat. Genet. 23, 99–103.
28. Horie, M., Watanabe, K., Bepari, A.K., Nashimoto, J., Araki, K.,
Sano, H., Chiken, S., Nambu, A., Ono, K., Ikenaka, K., et al.
(2014). Disruption of actin-binding domain-containing Dystonin protein causes dystonia musculorum in mice. Eur. J.
Neurosci. 40, 3458–3471.
29. Borodulin, K., Vartiainen, E., Peltonen, M., Jousilahti, P., Juolevi, A., Laatikainen, T., Männistö, S., Salomaa, V., Sundvall, J.,
and Puska, P. (2015). Forty-year trends in cardiovascular risk
factors in Finland. Eur. J. Public Health 25, 539–546.
30. Duan, R., Shi, Y., Yu, L., Zhang, G., Li, J., Lin, Y., Guo, J., Wang,
J., Shen, L., Jiang, H., et al. (2016). UBA5 mutations cause a
new form of autosomal recessive cerebellar ataxia. PLoS ONE
11, e0149039.
31. Watson, C.M., Crinnion, L.A., Gleghorn, L., Newman, W.G.,
Ramesar, R., Beighton, P., and Wallis, G.A. (2015). Identification of a mutation in the ubiquitin-fold modifier 1-specific
peptidase 2 gene, UFSP2, in an extended South African
family with Beukes hip dysplasia. S. Afr. Med. J. 105, 558–563.
694 The American Journal of Human Genetics 99, 683–694, September 1, 2016
�