Djènontin et al. Parasites & Vectors 2010, 3:83
http://www.parasitesandvectors.com/content/3/1/83
RESEARCH
Open Access
Culicidae diversity, malaria transmission and
insecticide resistance alleles in malaria vectors
in Ouidah-Kpomasse-Tori district from Benin
(West Africa): A pre-intervention study
Armel Djènontin1,2*, Sahabi Bio-Bangana1, Nicolas Moiroux2, Marie-Claire Henry2,4, Olayidé Bousari2, Joseph Chabi2,
Razaki Ossè1, Sébastien Koudénoukpo1, Vincent Corbel2, Martin Akogbéto1, Fabrice Chandre3
Abstract
Background: To implement an Insecticide Resistance Management (IRM) strategy through a randomized
controlled trial (phase III), 28 villages were selected in southern Benin. No recent entomological data being
available in these villages, entomological surveys were performed between October 2007 and May 2008, before
vector control strategies implementation, to establish baseline data.
Methods: Mosquitoes were sampled by human landing collection (16 person-nights per village per survey per village)
during 5 surveys. Mosquitoes were identified morphologically and by molecular methods. The Plasmodium falciparum
circumsporozoïte indexes were measured by ELISA, and the entomological inoculation rates (EIRs) were calculated.
Molecular detection of pyrethroid knock down resistance (Kdr) and of insensitive acetylcholinesterase were performed.
Results: 44,693 mosquitoes belonging to 28 different species were caught from October 2007 to May 2008.
Among mosquitoes caught, 318 were An. gambiae s.s., 2 were An. nili, 568 were An. funestus s.s., and one individual
was An. leesoni. EIR was 2.05 ± 1.28 infective bites per human per 100 nights on average, of which 0.67 ± 0.60
were from An. funestus and 1.38 ± 0.94 infective bites were from An. gambiae. Important variations were noted
between villages considering mosquito density and malaria transmission indicating a spatial heterogeneity in the
study area. The kdr allelic frequency was 28.86% in An. gambiae s.s. on average and significantly increases from
October 2007 (10.26%) to May 2008 (33.87%) in M molecular form of An. gambiae s.s. Ace 1 mutation was found in
S molecular of An. gambiae s.s at a low frequency (< 1%).
Conclusion: This study updates information on mosquito diversity and malaria risk in rural villages from south Benin.
It showed a high spatial heterogeneity in mosquito distribution and malaria transmission and underlines the need of
further investigations of biological, ecological, and behavioral traits of malaria vectors species and forms. This study is
a necessary prerequisite to cartography malaria risk and to improve vector control operations in southern Benin.
Background
Malaria remains a major cause of morbidity and mortality in sub-Saharan Africa and represents one of the most
critical public health challenges for Africa. In 2008, 243
million cases of malaria was estimated worldwide leading
to 863 000 deaths of which 89% were in the African
* Correspondence: armeldj@yahoo.fr
1
Centre de Recherche Entomologique de Cotonou (CREC), 06 BP 2604
Cotonou, Bénin
Full list of author information is available at the end of the article
Region [1]. Treatment with Artemisinin Combination
Therapy (ACT), the use of Indoor Residual Spraying
(IRS) and Insecticide Treated Nets (ITNs) represent the
main approaches of malaria control [1]. Household ITNs
ownership reached more than 50% in several high burden
African countries [1]. Pyrethroids are the only insecticides used for net impregnation because of their strong
efficacy, their fast acting effect at low doses and their low
toxicity for mammals [2]. Unfortunately, pyrethroids
resistance in malaria vectors has spread across Africa and
© 2010 Djènontin et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly cited.
�Djènontin et al. Parasites & Vectors 2010, 3:83
http://www.parasitesandvectors.com/content/3/1/83
is now present in most of countries where national
malaria control programmes (NMCP) are implementing
large scale distribution of Long Lasting Nets to populations at risk, i.e. children under five and pregnant women
[3]. Up to now, there is no evidence that pyrethroids
resistance reduce the effectiveness of ITNs for malaria
control at operational scale [4]. However, a small scale
field trial carried out in an area of resistance in southern
Benin (Ladji) and Burkina Faso (Kou Valley) showed a
reduction of personal protection and overall insecticidal
effect of ITNs in experimental huts [5-7].
It is then urgent to find ways to manage this resistance in malaria vectors. In this context, malaria vectors control and insecticide resistance management
tools based on the use (alone or in combination with
pyrethroid-treated mosquito nets) of alternative classes
of insecticides with different mode of action than pyrethroids were developed and have already been evaluated in experimental huts, with good results against
wild populations of strongly resistant An. gambiae
[6,7].
To validate these strategies, their impact on malaria
transmission and insecticide resistance dynamic in
malaria vectors must be accessed through randomized
controlled trials under phase III. For that purpose, 28
villages were selected in Ouidah-Kpomasse-Tori
(OKT) health district in southern Benin. No entomological data from OKT health district was available.
Recent data relative to Culicidae fauna of Benin go
back up to 1950s [8,9]. Thus, in order to collect baseline data relative to mosquito’s diversity and abundance, malaria transmission and the prevalence of
insecticide resistance alleles in malaria vectors, entomological surveys were performed between October
2007 and May 2008 in the study area before implementing the vector control strategies. This paper
reports these baseline data.
Methods
Study area
The study was carried out in OKT health district. Twenty
eight villages were selected considering a size between
250-500 inhabitants, a distance between two villages
higher than two kilometers and the absence of a local
health center. The OKT health district is one of 36 health
districts in Benin. This district has essentially a sub-equatorial climate, with two dry seasons (August-September
and December-March), and two rainy seasons (April-July
and October-November). The average annual rainfall is
around 1200 mm, of which 700-800 mm come in the
first rainy season and 400-500 mm come in the second
rainy season. The average monthly temperatures vary
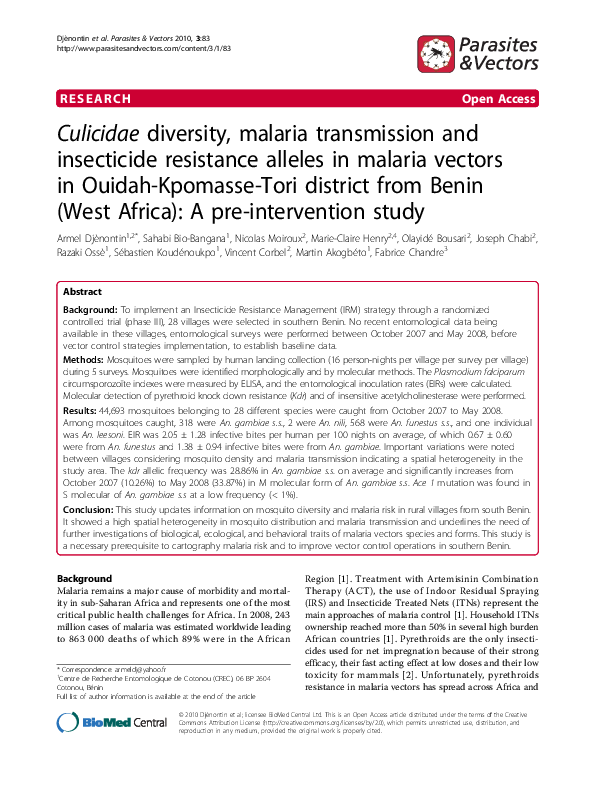
between 27 and 31°C. The northern part of the health
district is made of a plateau that drops into the Couffo
Page 2 of 7
valley and the Allada depression. The southern is watered
by several ramification arms of Toho Lake (Fig 1). The
study zone is totally cleared of the original equatorial forest. Currently, the vegetation is characterized by bushes
and isolated trees, associated with areas with more or less
densely populated areas with oil palm trees.
Mosquito’s collection and identification
Sampling of mosquitoes was done in 28 villages by
human landing catches using tubes that were plugged
with cotton. Mosquitoes collection was carried out during 5 surveys from October 2007 to May 2008 (2 in the
beginning of rainy periods and 3 in dry periods) every
6 weeks both indoors and outdoors at 4 sites per village
from 10 p.m. to 6 a.m. and for two consecutive nights
per survey (i.e. 16 person-nights per village per survey).
Teams of collectors were rotated among the collection
points on different collection nights to minimize sampling bias. Ethical clearance was given for the study by
the National Ethical Committee in Benin (Comité
National Provisoire d’Ethique pour la Recherche en
Santé) and IRD ethical committee (Comité Consultatif
de Déontologie et d’Ethique). Collectors gave prior
informed consent and they were vaccinated against yellow fever. Since study was done in area where malaria is
endemic, adult collectors that already acquired immunity against malaria parasites, did not received chemoprophylaxis, but were medically supervised by local
physicians in case of illness.
Mosquitoes were identified on the field to species level
using morphological criteria according to the identification keys [10-12]. All mosquitoes belonging to the
An. gambiae complex or An. funestus group were stored
in individual tubes with silica gel and preserved at -20°C
in the laboratory.
Determination of EIRs
Heads and thoraces of anopheline females were tested by
Enzyme-Linked Immunosorbent Assay (ELISA) for detection of P. falciparum circumsporozoite protein (CSP), as
previously described [13]. Samples having an optical density higher than 3 times the average of the optical density
of negative control were considered as positive. Those
having an optical density between 2 and 3 times this average were considered as doubtful and were retested.
The CSP index was calculated as the proportion of
mosquitoes found to be positive for CSP. Entomological
inoculation rates (EIRs) were estimated as the number
of infective bites per human per 100 nights.
Molecular analysis
All mosquitoes belonging to An. gambiae complex and
Anopheles funestus group were identified by polymerase
chain reaction (PCR) at the species levels [14,15].
�Djènontin et al. Parasites & Vectors 2010, 3:83
http://www.parasitesandvectors.com/content/3/1/83
Page 3 of 7
Figure 1 Map of the study area.
Molecular forms in Anopheles gambiae s.s. were also
identified [16].
Molecular characterizations of the Kdr (west-African
Leu-Phe mutation) and Ace1 mutations were carried out
on all mosquitoes belonging to An. gambiae complex as
previously described [17,18]
Statistical analysis
Chi-square tests were done to determine the odds of
association of the CSP index with malaria vectors An.
gambiae and An. funestus.
Data relative to mosquito’s density and EIRs according
to villages were analyzed using a Linear Mixed Effects
(LME) model implemented in R software and written as
follow:
Log (x) = b0 + b1i + ai, where:
x = means of mosquitoes number (or EIRs) per village
per survey
ß0 = estimated value of coefficient associated to the
reference village
ß 1i = estimated value of coefficient associated to a
village i
ai = intra-village variance
i = village index
Villages were grouped according to their homogeneity
for the entomological indicator considered taking into
account ßi and its P value. In each group, the average of
the number of mosquitoes caught per village per survey
(or the number of infective bites per human per 100
nights) was calculated with its 95% confidence interval.
The genotypic differentiation of kdr and Ace1 loci was
tested using the Fischer exact test implemented in GenePop software [19].
Results
Species diversity and density
A total of 44,693 mosquitoes belonging to 28 species
were caught (table 1). Mansonia Africana (44.84%),
Culex gr. decens (29.91%), Culex quinquefasciatus
(9.81%), and Culex nebulosis (6.22%) were the most
�Djènontin et al. Parasites & Vectors 2010, 3:83
http://www.parasitesandvectors.com/content/3/1/83
Page 4 of 7
Table 1 Mosquitoes species caught from October 2007 to
May 2008 in the study area
Species
Indoor
Outdoor
Total
%
Aedes aegypti
388
318
706
1.58
Aedes gr. palpalis
12
28
40
0.09
Aedes gr. tarsalis
Aedes luteocephalus
4
21
4
41
8
62
0.02
0.14
Aedes sp
13
37
50
0.11
Aedes vittatus
199
396
595
1.33
Anopheles brohieri
1
0
1
0.00
Anopheles coustani
3
5
8
0.02
Anopheles funestus
314
265
579
1.30
Anopheles gambiae
149
173
322
0.72
Anopheles nili
Anopheles pharoensis
1
60
1
135
2
195
0.00
0.44
Anopheles ziemanni
12
20
32
0.07
Culex annulioris
185
428
613
1.37
Culex duttoni
36
18
54
0.12
Culex fatigans
270
436
706
1.58
Culex gr. decens
4720
8649
13369
29.91
Culex nebulosis
1040
1738
2778
6.22
Culex perfuscus
Culex poicilipes
2
2
0
14
2
16
0.00
0.04
Culex quinquefasciatus
1170
3213
4383
9.81
Culex tigripes
17
38
55
0.12
Cx sp
17
17
34
0.08
Cx thalassius
10
16
26
0.06
Eretmapodites gr. quinquevittatus
0
3
3
0.01
7652
12390
20042
44.84
7
1
4
0
11
1
0.02
0.00
16306
28387
44693
Mansonia africana
Mansonia uniformis
Uranotaenia gr bilineata
Total
abundant species caught. The proportion of malaria vectors (Anopheles gambiae and Anopheles funestus) was
very low (~2%).
All mosquitoes belonging to Anopheles gambiae s.l.,
were An. gambiae s.s. (217 from S molecular form and
101 from M form). Concerning Anopheles funestus
group all mosquitoes were identified by PCR as Anopheles funestus s.s. except one individual which was An.
leesoni, caught in Tokoli-Vidjinangnimon village.
Large variations were observed between villages considering mosquito’s density. An average of 212 ± 46
Culicidae per village per survey and 531 ± 139 Culicidae
per village per survey were caught in two different
homogenous villages groups (Table 2). Concerning An.
gambiae s.l. on average 0.4 ± 0.2; 1.8 ± 0.6 and 7.4 ± 3.5
individuals were caught per village per survey in three
different homogenous villages groups (Table 3). In villages close to a arm of the Toho Lake, 13.48 ± 5.9 An.
funestus s.l. were caught on average per village per
Table 2 Average of Culicidae number caught per survey
per village from October 2007 to May 2008 with 95%
confidence intervals
Villages groups
Average Culicidea number per
survey per village with 95%
confidence intervals
Group 1: Agouako;
Assogbenoudaho; Guezohoue; Hla;
Todo; Zoume; Adjahassa; Satre;
Agadon; Aidjedo; Ayidohoue;
Dokanme; Tokoli Vidjinangnimon;
Hekandji; Hounkponouhoue;
Dekponhoue; Soko; Wanho; Tokoli;
Tanto
212 ± 46
Group 2 : Lokohoue; Tokoli
Vidjinangnimon; Manguevier;
Adjame-Allagbede; Amoulehoue;
Kindjitokpa; Abenihoue; Hinmandou
531 ± 139
survey, in contrast with 0.29 ± 0.1 in the others villages
(Table 4).
Vectors infection to CSP and malaria transmission risk
The CSP positivity rate was 9.63 ± 3.2% in An. gambiae
s.s. (5.94 ± 0.4% in M molecular form and 11.52 ± 0.2%
in S form) and 2.64 ± 1.3% in An. funestus s.l.. An. gambiae s.s. was more infected than An. funestus s.l. (OR =
4.00 (95%IC 2.13-7.54), P < 0.001). The average of EIR
from October 2007 to May 2008 was 2.05 ± 1.28 infective bites per human per 100 nights of which 0.67 ±
0.60 infective bites of An. funestus per human per 100
nights and 1.38 ± 0.94 infective bites of An. gambiae per
human per 100 nights. EIR was very variable according
to villages. Two homogenous villages groups with
respectively 0.7 ± 0.4 and 6.1 ± 3.4 infective bites per
human per 100 nights were observed (Table 5).
Table 3 Average of An. gambiae s.l. number caught per
survey per village from October 2007 to May 2008 with
95% confidence intervals
Villages groups
Average An. gambiae s.l.
number per survey per village
with 95% confidence intervals
Group 1: Adjame-Allagbede;
Agouako; Assogbenoudaho;
Kindjitokpa; Guezohoue;
Hinmandou; Hla; Abenihoue; Todo;
Zoume
0.4 ± 0.2
Group 2: Adjahassa; Satre;
Lokohoue; Agadon; Aidjedo;
Ayidohoue; Dokanme; Tokoli
Vidjinangnimon; Hekandji; Agokon;
Hounkponouhoue; Dekponhoue;
Manguevier
1.8 ± 0.6
Group 3: Amoulehoue; Soko;
Tokoli; Tanto; Wanho
7.4 ± 3.5
�Djènontin et al. Parasites & Vectors 2010, 3:83
http://www.parasitesandvectors.com/content/3/1/83
Table 4 Average of An. funestus s.l. number caught per
survey per village from October 2007 to May 2008 with
95% confidence intervals
Villages groups
Average An. funestus s.l. number
per survey per village with 95%
confidence intervals
Group 1: Adjame-Allagbede;
Agouako; Assogbenoudaho;
Guezohoue; Hinmandou; Hla;
Abenihoue; Todo; Zoume;
Adjahassa; Satre; Agadon; Agokon;
Aidjedo; Ayidohoue; Dokanme;
Hekandji; Hounkponouhoue;
Dekponhoue; Soko
0.29 ± 0.1
Group 2: Amoulehoue; Tokoli;
Tanto; Lokohoue; Manguevier;
Kindjitokpa; Tokoli Vidjinangnimon;
Wanho
13.48 ± 5.9
Page 5 of 7
Table 6 kdr in M and S molecular forms of An. gambiae
s.s. from October 2007 to May 2008 in the study area
October-December 2007
January-May 2008
M form
S form
M form
RR
0
10
13
S form
16
RS
SS
8
31
62
74
16
33
20
35
Total
39
146
62
71
Allelic frequency (%)
10.26a
28.08b
33.87b
36.62b
Kdr allelic frequency values carrying the same letter was not significantly
different (P > 0.05)
Kdr resistance gene status in An. gambiae.
The average of kdr allelic frequency from October 2007
to May 2008 was 28.86% in An. gambiae s.s. At the
beginning of the study (From October to December
2007), kdr allelic frequency was significantly higher in S
molecular form of An. gambiae s.s. (28.08%) compared
to the M molecular form (10.26%) (P = 0.001). This allelic frequency significantly increased in the M molecular
form and has reached 33.87% (P < 0.001) from January
to May 2008 (Table 6).
Insensitive acetylcholinesterase gene status in
An. gambiae s.l
The allelic frequency of this gene was less than 1%. Only
two heterozygous individuals was found in the S molecular form of An. gambiae s.s. at Tanto and Hekandji
during October 2007.
Discussion
The present study provides entomological baseline data
on OKT health district. Twenty eight different species
Table 5 Number of infective bites per human per 100
nights from October 2007 to May 2008 with 95%
confidence intervals
Villages groups
Number of infective bites per
human per 100 nights with
95% confidence intervals
Group 1 : Adjame; Agouako;
Aidjedo; Asogbenoudaho;
Ayidohoue; Adjahassa; Dokanme;
Kindjitokpa; Guezohoue;
Hinmandou; Hla; Hounkponouhoue;
Abenihoue; Dekponhoue;
Manguevier; Satre; Todo; Tokoli;
Wanho; Agadon; Zoume
Group 2 : Amoulehoue; Tokoli
Vidjinangnimon; Hekandji; Agokon;
Soko; Lokohoue; Tanto
0.7 ± 0.4
6.1 ± 3.4
were caught during surveys whereas Huttel (1950) and
Hamon (1954) had collected respectively 13 species
(adult’s collection in the dwellings) and 45 species (adult
and larval collection) in the south-east of Benin (Cotonou and Porto-Novo) [8,9]. If the Culicidae diversity is
lower in our study, we have identified 3 Anopheles species that was not mentioned in Hamon study: An. brohieri, An. coustani and An. nili. These 3 species were
present at very low densities, explaining why they were
not reported previously. More unexpected is the predominance in our study of Mansonia africana and the presence of Cx quinquefasciatus that were not reported by
Hamon. The relative abundance of Cx. quinquefasciatus
is particularly surprising for a species which is adapted
to polluted larval breeding sites and usually more familiar with urban environment than traditional villages
from this study. Results showed a high heterogeneity of
the study area in terms of Culicidae and especially
malaria vectors abundance. It could be due to the geographic pattern of this area that is characterized by a
northern part made of a plateau and the southern
watered by several ramification arms of Toho Lake. An.
funestus density was higher in villages close to arms of
Toho Lake (< 2 km), since some of its larval breeding
sites are the bank of lake or river with vegetation. In
most villages of the study area, the soil is made of a
thick bed of a mixture of sand and clay allowing a rapid
water infiltration after rain. This impedes the formation
of An. gambiae larval breeding sites that could explain
the low density of malaria vectors. However, on the 5
surveys conducted in each village, only two were conducted during a rainy period (in the beginning of the
rainy periods). This could explain the very low number
of anopheles vectors caught during the study. Further
studies conducted on a long period and taking into
account environmental factors are required to better
understand mosquito’s distribution determinants in this
area.
Anopheles gambiae s.s. and An. funestus s.s. were
shown to be the main vectors in the study area, confirming previous studies in West Africa [20-22]. The
�Djènontin et al. Parasites & Vectors 2010, 3:83
http://www.parasitesandvectors.com/content/3/1/83
relative abundance of An. funestus in the study area and
its CSP positivity rate (2.64 ± 1.3) indicate that this
mosquito is involved in malaria transmission in southern Benin. No data relative to resistance status and
mechanisms of this vector being available in Benin,
further studies about An. funestus populations and their
resistance mechanisms are required. The EIR, 2.05 ±
1.28 infective bites per human per 100 nights on average, indicates that in the study area, malaria is mesoendemic. These data agree with parasitological and clinical
data collected in the same way in these villages indicating an annual prevalence rate of 21.8% (19.1-24.4) in
young asymptomatic children and a clinical incidence of
Plasmodium falciparum malaria of 1.5 (1.2-1.9) per
child per year (Damien et al. 2010, unpublished data).
The kdr-w resistance allele was identified in An. gambiae populations examined in this study and have significantly increased from October 2007 to May 2008 in M
molecular form in contrast with S form, indicating probably that M and S molecular forms of this vector
undergo different selection pressures in the study area
and underlines the need of further studies taking into
account ecological and others factors. The presence of
the kdr-w allele in An. gambiae s.s. and the increase of
its frequency are worrying because this gene and metabolic resistance mechanisms in southern Benin appears
to have a significant impact on LLIN efficacy as demonstrated by recent experimental hut trial [23]. Many
other studies have showed a strong decrease of Pyrethroid-Treated Nets performance against pyrethroidresistant malaria vectors in Benin [5,6], Burkina Faso
[7], and Côte d’Ivoire [24].
Regarding carbamate resistance, we confirmed the low
allelic frequency of the ace-1R allele (< 1%) in An. gambiae s.s. in West Africa [25], showing that there is no
(or very low) selection pressure on this allele in the
study area. However, a monitoring of this resistance
gene is required considering the large scale implementation of Indoor Residual Spraying using bendiocarb by
President’s Malaria Initiative program in south Benin
that will inevitably increase the selection pressure on
vectors populations.
Conclusion
This study updates information on mosquito’s distribution and their role in malaria transmission in southern
Benin. It showed a high spatial heterogeneity in mosquitoes distribution and malaria transmission and then
underlines the need of further investigations of biological, ecological, and behavioral traits of malaria vectors
species and forms. That will allow to cartography
Page 6 of 7
malaria risk and then to improve vector control interventions in Benin.
Acknowledgements
We thank the Ministère Français des Affaires Etrangères for project REFS N°
2006-22 and the Institut de Recherche pour le Developpement, which
financially and materially supported the work. We thank populations of the
study area, OKT health district, for their collaboration. We also thank Seth
Irish for his linguistic assistance while drafting this manuscript.
Author details
1
Centre de Recherche Entomologique de Cotonou (CREC), 06 BP 2604
Cotonou, Bénin. 2Institut de Recherche pour le Développement (IRD/UR016),
01 BP 4414 Cotonou, Bénin. 3Laboratoire de lutte contre les Insectes
Nuisibles (LIN/IRD), 911 Ave Agropolis BP 64501, 34394 Montpellier Cedex 5,
France. 4Service de Coopération française, Ambassade de France, Cotonou,
Bénin.
Authors’ contributions
FC and M-CH conceived of the study. AD, JC and FC have participated in
the design of the study. Entomologic data was collected by AD, JC, RO, SK.
AD, SK and RO carried laboratory analysis. AD, FC, OB and VC have
participated in the analysis and interpretation of data. Maps were provided
by SBB and NM. The manuscript has been drafted by AD. AD, SBB, NM, MCH, OB, JC, RO, SK, VC, MA and FC have been involved in manuscript
revising. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Received: 14 July 2010 Accepted: 6 September 2010
Published: 6 September 2010
References
1. WHO: World Malaria Report 2009. World Health Organzation, Geneva 2009.
2. Zaim M, Aitio A, Nakashima N: Safety of pyrethroid-treated mosquito
nets. Med Vet Entomol 2000, 14:1-5.
3. Santolamazza F, Calzetta M, Etang J, Barrese E, Dia I, Caccone A,
Donnelly MJ, Petrarca V, Simard F, Pinto J, della Torre A: Distribution of
knock-down resistance mutations in Anopheles gambiae molecular forms
in west and west-central Africa. Malar J 2008, 7:74.
4. Henry MC, Assi SB, Rogier C, Dossou-Yovo J, Chandre F, Guillet P,
Carnevale P: Protective efficacy of lambda-cyhalothrin treated nets in
Anopheles gambiae pyrethroid resistance areas of Cote d’Ivoire. Am J
Trop Med Hyg 2005, 73:859-864.
5. N’Guessan R, Corbel V, Akogbéto M, Rowland M: Reduced efficacy of
insecticide-treated nets and indoor residual spraying for malaria control
in pyrethroid resistance area, Benin. Emerg Infect Dis 2007, 13:199-206.
6. Djènontin A, Chabi J, Baldet T, Irish S, Pennetier C, Hougard JM, Corbel V,
Akogbéto M, Chandre F: Managing insecticide resistance in malaria
vectors by combining carbamate-treated plastic wall sheeting and
pyrethroid-treated bed nets. Malar J 2009, 8:233.
7. Djènontin A, Chandre F, Dabiré KR, Chabi J, N’Guessan R, Baldet T,
Akogbéto M, Corbel V: The Indoor Use of Plastic Sheeting Impregnated
with Carbamate in Combination with Long Lasting Insecticidal Mosquito
Nets for the Control of Pyrethroid-resistant Malaria. Am J Trop Med Hyg
2010, 83:266-270.
8. Huttel J: Note sur la répartition des moustiques dans le Bas-Dahomey.
Bull Sot Path Exot 1950, 43:563-566.
9. Hamon J: Contribution à l’étude des Culicidés de la région de PortoNovo (Bas-Dahomey). Ann parasitologie 1954, 29:588-594.
10. Edwards F: Mosquitoes of the Ethiopian Region III. Culicine adults and
pupae. British Museum (Nat Hist), London 1941.
11. Gillies MT, De Meillon BL: The Anophelinae of Africa south of the Sahara
Publication of the South African Institute for Medical Research,
Johannesburg 1968, 54.
�Djènontin et al. Parasites & Vectors 2010, 3:83
http://www.parasitesandvectors.com/content/3/1/83
Page 7 of 7
12. Gillies MT, Coetzee M: A Supplement to the Anophelinae of Africa South of
the Sahara (Afrotropical Region) Publication of the South African Institute for
Medical Research, Johannesburg 1987, 55.
13. Wirtz RA, Zavala F, Charoenvit Y, Campbell GH, Burkot T, Schneider I,
Esser KM, Beaudoin RL, Andre RG: Comparative testing of monoclonal
antibodies against Plasmodium falciparum sporozoites for ELISA
development. Bull World Health Organ 1987, 65:39-45.
14. Scott JA, Brogdon WG, Collins FH: Identification of single specimens of
the Anopheles gambiae complex by the polymerase chain reaction. Am J
Trop Med Hyg 1993, 49:520-529.
15. Koekemoer LL, Kamau L, Hunt RH, Coetzee M: A cocktail polymerase chain
reaction assay to identify members of the Anopheles funestus (Diptera:
Culicidae) group. Am J Trop Med Hyg 2002, 66:804-811.
16. Favia G, Lanfrancotti A, Spanos L, Siden Kiamos I, Louis C: Molecular
characterization of ribosomal DNA polymorphisms discriminating among
chromosomal forms of Anopheles gambiae s.s. Insect Mol Biol 2001,
10:19-23.
17. Martinez-Torres D, Chandre F, Williamson MS, Darriet F, Berge JB,
Devonshire AL, Guillet P, Pasteur N, Pauron D: Molecular characterization
of pyrethroid knockdown resistance (kdr) in the major malaria vector
Anopheles gambiae s.s. Insect Mol Biol 1998, 7:179-184.
18. Weill M, Malcolm C, Chandre F, Mogensen K, Berthomieu A, Marquine M,
Raymond M: The unique mutation in ace-1 giving high insecticide
resistance is easily detectable in mosquito vectors. Insect Mol Biol 2004,
13:1-7.
19. Raymond M, Rousset F: GENEPOP (version 1.2): population genetics
software for exact tests and ecumenicism. J Heredity 1995, 86:248-249.
20. Akogbéto M: Entomological study on the malaria transmission in coastal
and lagoon areas: the case of a village built on a brackish lake. Ann Soc
Belg Med Trop 1995, 75:219-227.
21. Fontenille D, Simard F: Unravelling complexities in human malaria
transmission dynamics in Africa through a comprehensive knowledge of
vector populations. Comp Immunol Microbiol Infect Dis 2004, 27:357-375.
22. Louise A, Kelly-Hope L, Ellis McKenzie F: The multiplicity of malaria
transmission: a review of entomological inoculation rate measurements
and methods across sub-Saharan Africa. Malar J 2009, 8:19.
23. WHO: Report of the twelfth WHOPES Working group meeting. WHO/
HTM/NTD/WHOPES 2009, 1.
24. N’Guessan R, Darriet F, Doannio JM, Chandre F, Carnevale P: Olyset Net
efficacy against pyrethroid-resistant Anopheles gambiae and Culex
quinquefasciatus after 3 years’ field use in Côte d’Ivoire. Med Vet Entomol
2001, 15:97-104.
25. Djogbénou L, Dabire R, Diabate A, Kengne P, Akogbéto M, Hougard JM,
Chandre F: Identification and geographic distribution of the ACE-1R
mutation in the malaria vector Anopheles gambiae in south-western
Burkina Faso, West Africa. Am J Trop Med Hyg 2008, 78:298-302.
doi:10.1186/1756-3305-3-83
Cite this article as: Djènontin et al.: Culicidae diversity, malaria
transmission and insecticide resistance alleles in malaria vectors
in Ouidah-Kpomasse-Tori district from Benin (West Africa): A preintervention study. Parasites & Vectors 2010 3:83.
Submit your next manuscript to BioMed Central
and take full advantage of:
• Convenient online submission
• Thorough peer review
• No space constraints or color figure charges
• Immediate publication on acceptance
• Inclusion in PubMed, CAS, Scopus and Google Scholar
• Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
�
 Marie-claire Henry
Marie-claire Henry