PAPERS
Comparison of enalapril and nifedipine in treating non-insulin
dependent diabetes associated with hypertension: one year analysis
J C N Chan, C S Cockram, M G Nicholls, C K Cheung, R Swaminathan
Departments of Clinical
Pharmacology, Medicine,
and Chemical Pathology,
Abstract
Objectives-To compare the efficacy, safety, and
tolerance of enalapril and nifedipine in hypertensive
patients with non-insulin dependent diabetes.
Design-One year double blind follow up of
patients randomly allocated to either enalapril or
nifedipine with matching placebos for the alternative
drug.
Setting-Metabolic Investigation Unit, Hong
Kong.
Subjects-102 patients were randomised: 52 to
nifedipine and 50 to enalapril. At baseline 44 patients
had normoalbuminuria, 36 microalbuminuria, and
22 macroalbuminuria.
Main outcome measures-Blood pressure,
albuminuria, and parameters of renal function and
glycaemic control.
Results-In patients who completed one year's
treatment the median dose required by the nifedipine
group (n=49) was 60 mg/day; seven (14%) required
additional diuretics. Of 41 patients given enalapril,
37 required the maximum dose (40 mg/day) and 27
(76%) required diuretics. At one year mean arterial
blood pressures were similar in both groups.
Albuminuria fell by 54% in the enalapril group and
/in the nifedipine group (p=0 006). Fractional
11%
albumin clearance ratio fell by 47% in the enalapril
deterioration in kidney function in patients with
insulin dependent diabetes mellitus.' Angiotensin II
has potent vasoconstrictive effects on the efferent renal
arteriole2; thus angiotensin converting enzyme
inhibitors might reduce filtration pressure and
preserve renal function more successfully than alternative antihypertensive drugs. Indeed, animal data
suggest that this may be so.34 The antiproteinuric and
renal protective effects of long term treatment with
angiotensin converting enzyme inhibitors have
recently been reported in insulin dependent diabetes.)
Nevertheless, non-insulin dependent diabetes, which
is the more prevalent form of diabetes, particularly
among non-whites,6 contributes importantly to the
patient population with end stage renal failure.7 To
date, only a few clinical trials have studied the effects of
angiotensin converting enzyme inhibitors in patients
with non-insulin dependent diabetes and the results
have been inconclusive.8-'6
We conducted a study to compare the long term
effects of the angiotensin converting enzyme inhibitor
enalapril with the calcium channel blocker nifedipine
in the treatment of non-insulin dependent diabetes
associated with hypertension.
group and increased by 3% in the nifedipine group
(p=0.009). Creatinine clearance fell similarly in both
STUDY PROTOCOL
The study was approved by the ethics committee of
Patients and methods
StUDY PROTOCoL
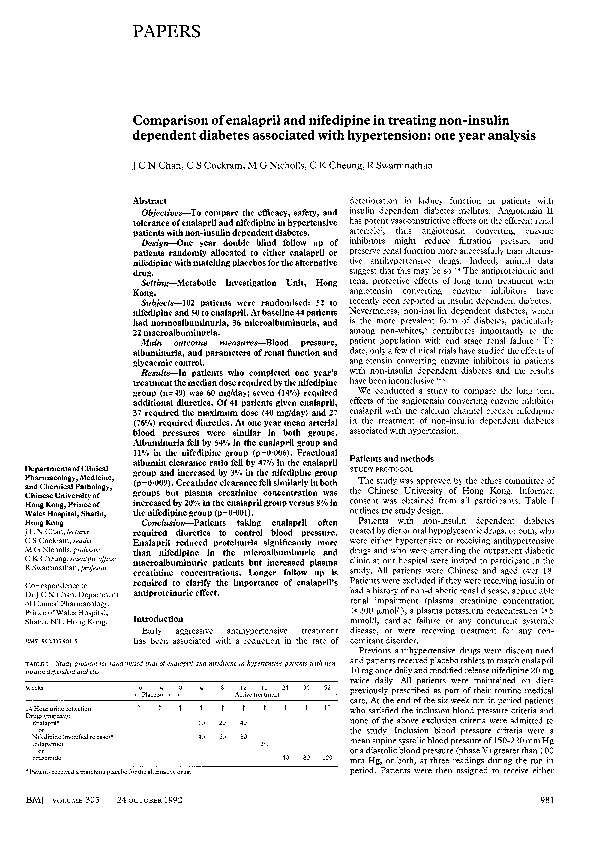
TABL.E i-Study protocol for randornised tnial of enalapril anid nzifedipine in hypertensive patients with notzinsulin dependent diabetes
12
i6 24 36 52
4
8
-6
0
Weeks
-4
Active treatment
Placebo-8
24 Hour urine collection
1 111
1
1
1
1
1
11
Dsrugs (mg/day):.
10 20 40
Enalapril*
or
8060
40
Nifedipine (modified release)*
2-5
Indapamide
or
40 80 120
Frusemide
the Chinese University of Hong Kong. Informed
consent was obtained from all participants. Table I
outlines the study design.
Patients with non-insulin dependent diabetes
treated by diet or oral hypoglycaemic drugs, or both, who
were either hypertensive or receiving antihypertensive
drugs and who were attending the outpatient diabetic
clinic at our hospital were invited to participate in the
study. All patients were Chinese and aged over 18.
Patients were excluded if they were receiving insulin or
had a history of non-diabetic renal disease, appreciable
renal impairment (plasma creatinine concentration
¢ 200 Vmol/l), a plasma potassium concentration > 5
mmol/l, cardiac failure or any concurrent systemic
disease, or were receiving treatment for any concomitant disorder.
Previous antihypertensive drugs were discontinued
and patients received placebo tablets to match enalapril
10 mg once daily and modified release nifedipine 20 mg
twice daily. All patients were maintained on diets
of thi otn
eia
eia
previously prescribed as part o hi otn
care. At the end of the six week run in period patients
who satisfied the inclusion blood pressure criteria and
none of the above exclusion criteria were admitted to
the study. Inclusion blood pressure criteria were a
mean supine systolic blood pressure of 150-220 mm Hg
or a diastolic blood pressure (phase V) greater than 100
mm Hg, or both, at three readings during the run in
*Patients received a matching placebo for the altemnative
period. Patients were then assigned to receive either
Chinese University of
Hong Kong, Prince of
Wales Hospital, Shatin,
Hong Kong
J C N Chan, lecturer
C S Cockram, reader
M G Nicholls, professor
C K Cheung, scientific officer
R Swaminathan, professor
Correspondence to:
Dr J C N Chan, Department
of Clinical Pharmacology,
Prince of Wales Hospital,
Shatin, NT, Hong Kong.
BAI1992;305:981-5
BMJ VOLUME 305
groups but plasma creatinine concentration was
increased by 20% in the enalapril group versus 8% in
the nifedipine group (p= 000l).
Conclusion-Patients taking enalapril often
required diuretics to control blood pressure.
Enalapril reduced proteinuria significantly more
than nifedipine in the microalbuminuric and
macroalbuminuric patients but increased plasma
creatinine concentrations. Longer follow up is
required to clarify the importance of enalapril's
antiproteinuric effect.
Introduction
Early aggressive antihypertensive treatment
has been associated with a reduction in the rate of
24 OCTOBER 1992
drug.
981
�enalapril or modified release nifedipine with matching
placebo tablets for the alternative drug according to a
random allocation schedule. A schedule of 102 allocation numbers corresponding to similarly numbered
drug supplies was provided for this purpose. Both the
patients and the staff measuring blood pressure and
biochemical indices were blinded to treatment.
Based on the mean value of three measurements
of 24 hour urinary albumin excretion during the
run in period, 44 patients had normoalbuminuria
(< 30 mg/day), 36 microalbuminuria (30-300 mg/day),
and 22 macroalbuminuria (> 300 mg/day).',
Drug doses were increased over 12 weeks to a
maximum of enalapril 40 mg once daily or nifedipine
40 mg twice daily if supine systolic blood pressure
remained above 140 mm Hg (table I). Indapamide 2 5
mg/day was added if the blood pressure remained high
and, if necessary, this was replaced by frusemide (up to
120 mg/day) to achieve the target supine systolic blood
pressure. Follow up visits were scheduled between
8 am and 10 am, at which time the blood pressure
was measured, and venous blood was sampled for
measurements of renal function, glycated haemoglobin, plasma fructosamine, and fasting plasma
glucose concentration, and serum angiotensin
converting enzyme activity. Twenty four hour urine
samples were collected for estimation of albumin
excretion. At the end of one year two 24 hour urine
samples were collected within two weeks.
week of collection for albumin concentration by
immunoturbidimetry using a modification of a
published technique.'8 Intra-assay and interassay
coefficients of variation were 3.3% and 6-7% respectively within the range 1-2-80 mg/l. The lowest
detection limit was 1-2 mg/l. Plasma and urine
creatinine concentrations were measured by the Jaffe
method on an Astra-8 Chemistry Analyser (Beckman
Instrument, Palo Alto, California). Glycated haemoglobin concentration (HbA1) was measured by gel
electrophoresis (Ciba Coming Diagnostics, Alto,
California) with a reference range of 6-5-8 5%. Plasma
glucose concentration was measured by a glucose
oxidase method (Diagnostic Chemicals reagent kit) and
plasma fructosamine, by published methods."'.Serum
angiotensin converting enzyme activity was measured
by a modified spectrophotometric method2" and the
intra-assay and interassay coefficients of variation
were less than 50/n.
For presentation of skewed data that were analysed
as logarithms, the mean was back transformed
(antilogged) to give the geometric mean and the 95%
confidence intervals obtained for the mean of the log
data were also antilogged.
MEASUREMENTS
excretion. The mean (SD) or geometric mean (antilog
of SD) values for all variables measured during the
last two visits of the run in period were taken as
baseline values. Doses of drugs administered are
given as median. Fractional albumin clearance
ratios were calculated as 24 hour urinary albumin concentrationxplasma creatinine concentration/plasma
albumin concentrationx24 hour urinary creatinine
concentration. Plasma creatinine concentration,
creatinine clearance, fractional albumin clearance
ratio, and urinary albumin excretion and serum
angiotensin converting enzyme concentration were
log transformed before analysis because of skewed
distributions. The mean value from two measurements
of urinary albumin excretion, fractional albumin
clearance ratio, and creatinine clearance estimated at
the end of one year were compared with baseline values
and differences were compared between treatment
groups. Mean (95% confidence interval) differences
between the two treatment groups were examined by
Student's two tailed t test. The antilog of a difference
between two means was transformed into relative
changes expressed as ratios compared with baseline
95* confidence intervals. Fisher's exact
values with
test was used to compare the rates of conversion from
Blood pressure was measured by a single research
nurse using a Hawksley random zero sphygmomanometer after the patient had rested for five minutes
in the supine position and also after two minutes of
standing. The mean of two readings for each body
position was recorded. Mean arterial blood pressure
was calculated as diastolic blood pressure plus one
third of the difference between systolic and diastolic
blood pressure and was shown as a mean of supine and
standing values unless otherwise stated. All urine
samples were stored at 4°C and analysed within one
TABLE 11-Clinical characteristics of patienits and mean biochenmical
data fronm the last two visits of the rnti in period. Values are nmeans
(SD) uniless stated otherwise
Nifedipine
group
(n-52)
Enalapril
group
(n=50)
No of men
No ofwomen
21
31
20
30
Age (years)
56 1 (9 9)
60 1 (9 2)
Duration of diabetes (years)
5 6 (4 6)
Duration of hypertension (years)
(°) with retinopathy
No (°) with neuropathy
Body mass index (kg/m2)
53 (47)
No
5 5 (4 8)
56 (53)
22 (42)
17 (34)
14 (27)
15 (30)
24 8 (3 0)
25 2 (2 9)
174/92 (17/13)
Supine blood pressure (mm Hg)
166/91 (16/9)
Erect blood pressure (mm Hg)
167/94 (16/12) 171/94 (19/14)
Mean arterial blood pressure (mm Hg)
Glycatedhaemoglobin (%/)
Plasma fructosamine (mmol/l)
Fasting plasma glucose(mmol/l)
Geometric mean (antilog SD) plasma
creatinine (tLmol/l)
Geometric mean (antilog SD) urinarw
albumin excretion (mg/day)
Geometric mean (antilog SD) creatinine
clearance (ml/min)
117 (9)
9 8 (1-7)
2 3 (0Q23)
120 (12)
10-4 (1 7)
80 9 (1-4)
83-0 (1 3)
69-5 (6 8)
64 7 (6 6)
70*0 (1 6)
65-5 (1 5)
152 (9 6)
1 5 3 (7 4)
80 (21)
2 3 (0-23)
83 (25)
Geometric mean (antilog SD) fractional
albumin clearance ratio (x 10-c)
T"ABLE ill-Severity
of proteinuria at baseline
anld
the number of patienlts
who1 comwpleted onue year of
treatment in each categor
STATrISTICS
The study required 51 patients in each treatment
group to have a 90% power at the 5% level (two tailed)
to show that one drug was at least twice as
effective as the other in reducing urinary albumin
normoalbuminuria to abnormal albuminuria between
the treatment groups. Repeated measures analysis of
variance was used to test for the effects of treatment
and its duration. Only data from patients who completed the one year study were included for these
comparisons. Statistical analysis was performed with
the packages ABstat (Anderson-Bell, Colorado,
United
States 1989) and SPSS Significance was taken
U
as p < 0 05 (two tailed).
Results
I'OPUIATION CHARACTERISTICS
Of 123 patients recruited, 102 fulfilled all inclusion
Category
Normoalbuminuria
Microalbuminuria
Macroalbuminuria
_____
982
____
____
Urinarv albumin
excretion(mg/day)
WeekO0
Week 52
< 30
24
24
30-300
15
13
> 300
____
____
____
____
____
WeekO0
Week 52
20
18
21
9
15
10
____
criteria and were randomised to active treatment.
Enalapril group
Nifedipine group
____
____
____
16
7
____
____
Table II shows the baseline clinical characteristics and
mean biochemical data from the last two visits of the
run in period. Table III shows the level of albuminuria
a aeieadtenme fptet h opee
a aeleadtenme fptet h opee
one year of treatment in the subgroups. Forty nine of
BMJ VOLUME 305
24 OCTOBER 1992
�IAABLE 1V-Changes in urinarv albumlinl excretion, fracictwnal albumiinl clearance, endogenous creatinine clearance, plasmiia creatinine
concentration, and arterial blood pressuire in1 pati'ents aftetr onze year of treatment zith
eaniftedipime or enalapril
Urinarv albumin cxcretio;'*:
Enalapril
Nifedipine
p Value
Fractional albumin clearance ratio*:
Enalapril
Nifedipine
p Value
Creatinine clearance*:
Enalapril
Nifedipine
p Value
Plasma creatinine*:
Enalapril
Nifedipillc
pV'aluc
Mlean arterial pressuret:
Enalapril
Nifedipine
pValue
Wholc group
Normoalbuminuria
Microalbuminuria
Mlacroalbuminuria
0 46 (0Q32 to 0-67)
0(89 (0-66 to 1-2)
0006
0-88 (0 59 to 1 34)
0 81 (0 55 to 12)
0 7151
0Q27 (0 15 to 0-46)
0-85 (0 43 to 0 88)
0(013
0 29 (0 1 I to 0 77)
1 15 (0 85 to 1 54)
0 006
0 53 (0)37 to 0 77)
1 03 (0(75 to 1 43)
0 009
0-95 (0 58 to 1 72)
0 96 (0 63 to 1-45)
0 773
0 28 (0l18 to 0 44)
0-99 (0 43 to 2 3)
0 012
0 38 (0l16 to 088)
1 3 ( to 1 66)
0 005
0 85 (0n75 to 0 97)
0 85 (0 79 to 0 92)
0 989
0 86 (0-72 to 103)
0 85 (0( 77 to 0 93)
0 841
0 89 (0 71 to 11)
0 88 (0 75 to 1.04)
0 989
0-76 (0 52 to 1 12)
0 83 (0 7 to 098)
0 675
1l2 (114to 126)
1 08 (1-05 to 1 12)
0(001
1 15 (109to 123)
1-06 (1 01 to 1 12)
0 034
1l26(117to 136)
1 06 (1 01 to 1 1)
1 17 (0 98to 1 4)
1 19 (1l08 to 1 3)
0 904
-21 2 (-248 to - 16 3)
-20 1(-24 1 to -18 4)
0 759
- 18 9 (-24.1 to - 13 8)
-17 5 (-20 9 to -14 1)
0 633
<0 001
-21 6 (-292 to - 13 9)
-251 (-31l1 to -19 1)
0 481
-22.0 (-34.3 to -9 7)
-24-5 (-29S5 to -19 4)
0 685
*iN\ean relative change expressed as ratios compared with baseline values (95% confidence intervals).
tMlean difference (95% confidence intervals).
p Values are for comparisons bersveen changes in the tsvo treatment groups (Student's two tailed t test).
TABLE \-Mean (95% confidence inter-val) chaniges in glycaemic inldices during 52 weeks' treatnmetnt with
enalapril or niifedipinle
Enalapril
group
Glycaemic index
Glycatedhaemoglobin ('%Io)
Plasma fructosamine (mmol/l)
Nifedipine
group
012 (-0 3 to 0(57)
0-00 (-0 07 to 0 09)
0 48 (-0 8 to 1 7)
063 (-02 to 47)
0( 14 (0-0 to 0 27)
0-42 (-0 6 to 1 5)
Plasma glucose (mmoUl)
p Value
0253
0 089
0 93
the 52 patients randomised to nifedipine completed
one year of treatment compared with 41 of 50 randomised to enalapril. Of the nine patients taking enalapril
who did not complete one year, three were withdrawn
because of cough, three were withdrawn because of
1
)s ofr blood
* * * pressure, one died
- 1 ofr
inadequate control
myocardial infarction, one developed angina, and
one defaulted. Of the three patients who received
nifedipine, one had inadequate blood pressure control,
onehad
uberculouslymphaone
had tuberculous
lymphaonenitishad angina, and one
denitis.
140
E
E
120
(
oo
E 11 \
100
R
l
c,
N
T
-
80
,
100
a
>
t-
.: S
Q t 10-
*b4 E
FIG 1-Bloodpressure
and
an.oeniduringcovrtn
activity
with
treatmnentenym.
entalapril () or nifedipine (0).
activity wasplotted on
logarithnaicscl. en
(geometric means) are shown
0
j
0
with SD values drawn as error
bars
BMJ VOLUME 305
diuretic treatment (20 took indapamide and
1
frusemide). The median dose of nifedipine was 60 mg/
day and 14% of patients (7/49) required additional
diuretics (four indapamide and three frusemide).
Although at one year the reduction in and the achieved
levels of mean arterial pressures were similar in both
treatment groups (table IV), blood pressure was
significantly higher overall in the enalapril group than
Il~~~~~n
ference
the nifedipine group (p< 0 -001I for drug diffrne
p<0 001 for time trend, and p=0 001 for time and
drug interaction). The relative change in serum angiot
c
e
a
tersin patint
eceiving
(0 12
getri
ainsrciigeaarl(-2(5
confidence interval 01 to 0 15)) than in those receiving
nifedipine (0 71(0 63 to 0 81), p<0001; fig 1).
Body mass index fell by 0 28 (-0 58 to 0 01) kg/m2
over 12 months in the enalapril group and 0 25 (-0 48
to -0.02) kg/mi in the nifedipine group (p=0 841).
The haemoglobin concentration fell by 7 5 (-11-5 to
-36) g/l in the enalapril group compared with a
reduction of 2 4 (-0 5 to 0 6) g/l in the nifedipine
group (p=0w035). At week 4, before the addition of
diuretics, the plasma glucose concentration had fallen
by 0 98 (-17 to -0 31) mmol/I in the patients
receiving enalapril compared with 0 09 (-0 57 to 0 38)
mmol/l
r < in those receiving nifedipine (p=0033). However, glycaemic indices were similar in the two treatment groups at one year and overall changes were not
significantly different between the groups (table V).
wenalapril
(95%/a
ALBUMINURIA AND RENAL FUNCTION
*t a)
Angiotenain converting enzyme
At one year, 90% (37/41) of the patients receiving
enalapril required the maximum dose of enalapril (40
mg/day) and 76%/o (31/41) required the addition of
I
300
E
o
T
BLOOD PRESSURE, BODY WEIGHT, AND GLYCAEMIC
CONTROL
24 OCTOBER 1992
Table IV summarises changes in mean arterial blood
pressure, urinary albumin excretion, fractional
- . A\ i 9 _ albumin clearance ratio, creatinine clearance, and
plasma creatinine concentration in the two treatment
_
1
>-1 a
F--groups. Treatment with enalapril reduced proteinuria,
the fractional albumin clearance ratio significantly
__
_
_
~~~~~~~~~and
more than treatment with nifedipine, in all patients
__
_ _ ~~~~~andalso in the microalbuminuric and macroserum
,,-albuminuric groups separately. In normoalbuminuric
patients,
urinary albumin excretion remained less than
30m/a nalo h 8ptet ie nlpi
0m/a nalo h 8ptet ie nlpi
whereas two of the 23 patients receiving nifedipine
developed abnormal albuminuria (p=0-62 1). Figure 2
I
I
l
l
shows changes in urinary albumin excretion in
12
36
iniiulptesdrngoeya oframn.
48
52
nvdulptet drigoeya oframn.
Creatinine clearance fell to a similar extent in both
-Weeks
E
T
.983
�TABIT V -The
cffrcts of additiOnal diuretic
on
renal
fiuction
and blood pressure in patients receiving
No diurctics
(n= 10)
Mean (95",, confidence interval) arterial pressure
(mmHg)
Diuretics
(n= 31)
-201 (-289to-11 1) -206(-255to-158)
Urinarv albumin excretion rate*
Fractional albumiin clearance ratio (x 10")*
Plasma creatinine (,umoUI)*
Creatinine clearance (ml/min)*
0765 (0 38 to 1709)
0 42 (0(27 to 065)
0 77 (0-34 to 7 1)
1 08 (0 98 to 1 18)
0Q90 (0 67 to 1 2)
0-47 (0-31 to 0-71)
124 (118
more effectively than f3 adrenoceptor blocking drugsf
prevalent form of diabetes, particularly among non-
0 84 (0-72 to 097)
whites,, and accounts for a considerable proportion of
7
pat.ents with end stage renal disease, few trials have
*MNean relative change expressed as ratios compared with baseline values (95% confidence intervals).
groups of patients but plasma creatinine concentration
was increased to a greater extent by treatment with
enalapril (table IV).
The effects of adding diuretics (indapamide or
frusemide) were analysed (table VI). There was no
difference in changes in urinary albumin excretion
between patients who received enalapril alone and
those requiring the addition of a diuretic. The rise in
plasma creatinine concentration was significantly
greater in patients receiving combined enalapril and
diuretic compared with that in those treated with
enalapril alone,
Normoalbuminuria
p=0.751
10
10000
Microalbuminuria
p=0.013
E
1000
been reported comparing angiotensin converting
enzyme inhibitors with alternative antihypertensive
drugs in such patients.5'5 Some of the longer term
studies suggest there is little difference between
antihypertensive drugs with regard to their effects on
urinary protein excretion"' whereas Ferder et al
reported that enalapril had a superior antiproteinuric
action to nifedipine in hypertensive patients."' We
studied a homogeneous population of 102 Chinese
patients with hypertension and non-insulin dependent
diabetes to compare the effects of an angiotensin
converting enzyme inhibitor, enalapril, with a calcium
channel blocker, nifedipine, on blood pressure, renal
function, and glycaemic control.
The antihypertensive effects of treatment with
enalapril and nifedipine were similar at one year, but
the fall in blood pressure was slower with the angiotensin converting enzyme inhibitor, as has been
reported previously in elderly white patients with
essential hypertension.2 Furthermore, more patients
receiving enalapril required a diuretic to achieve the
goal systolic blood pressure (140 mm Hg in the supine
position) than patients receiving nifedipine. These
apparent differences in antihypertensive effectiveness
might reflect the fact that full comparative dose
response (drug and blood pressure) curves were not
assessed, that the full antihypertensive action of
enalapril may require more than 12 weeks to develop
under the conditions of the study, and that racial
factors might modify the antihypertensive efficacy of
the drugs chosen-as is the case for 1 adrenoceptor
blockers and diuretics in black, compared with white,
patients.22
ALBUMINURIA
0
.j
Considerable attention has been directed to the
potential renal protective effects of angiotensin converting enzyme inhibitors in insulin dependent
diabetes, and recent data suggest that these drugs may
slow the rate of decline in glomerular filtration rate
Although non-insulin dependent diabetes is the more
1 31)t
tp=001.
100
Discussion
Despite a higher overall level of blood pressure,
patients receiving enalapril showed the greater
100
D'
_ 10
N
\
.:
Macroalbuminuria
10000
\ p=0.006
)
fall in urinary albumin excretion. A significant
antiproteinuric action of enalapril, compared with
nifedipine, was observed in patients who initially
exhibited macroalbuminuria or microalbuminuria.
rates of conversion from normoalbuminuria to
~~~~~~~~~~The
microalbuminuria were not different between the two
study groups after one year. As diuretics were required
by most patients receiving enalapril it is possible that
the diuretics, rather than the angiotensin converting
enzyme inhibitor, accounted for the fall in urinary
albumin excretion, especially since indapamide has
recently been shown
\
1000
FIG 2-Urinary albumin
excretion, expressed on
logarithmic scales, at weeks 0
and 52
in
microalbuminuria, and
macroalbuminuria. p Values are
shown for differences in changes
in urinaiy albumin excretion
between patients treated with
enalapril (a) and niffedipine
(0)
984
o
<
-
100
patients
to
have
an
hypertensive
~~~~~~in
patients.23
antiproteinuric action
non-insulin dependent diabetic
Further analysis of our data, however,
2
showed similar antiproteinuric effects of enalapril
whether or not a diuretic was added. Our data,
\\\ therefore, agree with the findings of Ferder et al, who
<reported that fixed dose enalapril (40 mg/day) for one
year in 18 hypertensive non-insulin dependent diabetic
patients reduced urine excretion significantly whereas
withfiedoenfdpn(4mgdyfaldtatruiay
normoalbuminuria,fiedoenfdpn(4mgdyfaldtatruiay
protein output in 12 patients.'5
-Endogenous creatinine clearance fell to a similar
extent in the two treatment groups. By contrast,
10
0
52
0
Weeks
52
plasma creatinine rose to a greater extent in patients
treated with enalapril. This discrepancy may be largely
due to the greater coefficient of variation inherent in
BMJ VOLUME 305
24 OCTOBER 1992
�the measurement of endogenous creatinine clearance,
as it is dependent not only on determination of plasma
creatinine concentrations but also on measurements of
urinary creatinine concentration and urine volume.24
Furthe'r analysis of our data showed that pla'sma
creatinine concentrations rose more in patients taking
enalapril who received concomitant diuretics than in
patients taking only enalapril. The higher plasma
creatinine concentration in the enalapril group might
therefore reflect the greater number of patients requiring a diuretic. In severe cardiac failure the combination of a diuretic and angiotensin converting enzyme
inhibitor often induces a rise in plasma creatinine
concentration 25-2 which, on prolonged treatment,
usually falls again.25 Bjorck et al also reported an early
fall in glomerular filtration rate in patients with insulin
dependent diabetes after the introduction of enalapril
but stabilisation occurred after six months. Whether
such a biphasic pattern in glomerular filtration rate
occurs in our patients, remains to be seen.
EFFECT ON GLYCAEMIC CONTROL AND HAEMOGLOBIN
Hypoglycaemia consequent on initiation of treatment with angiotensin converting enzyme inhibitors
has been reported in both insulin dependent and noninsulin dependent diabetic patients.28230 Furthermore,
the angiotensin converting enzyme inhibitors have
been shown to improve insulin sensitivity,"' perhaps as
a result of the accumulation of bradykinin, which has
an insulin-like action.32 Early in our study, the mean
fasting plasma glucose concentration fell significantly
in patients receiving enalapril, but not in those receiving nifedipine. Subsequent indices of glycaemic control were similar in the two groups, presumably
because the addition of diuretics, which are known to
worsen glucose tolerance,3" countered any beneficial
effect of the angiotensin converting enzyme inhibitor.
We observed a small but significant fall in haemoglobin concentration during treatment with enalapril.
Angiotensin converting enzyme inhibitors have also
been noted to reduce haemoglobin concentration in
patients with insulin dependent diabetes,5 congestive
heart failure, chronic renal failure, and kidney transplants."3 This effect may be partly due to a fall in
angiotensin II concentration, which is known to
stimulate erythropoietin under certain circumstances.33"
Chinese hypertensive patients with non-insulin
dependent diabetes treated with enalapril often
required additional diuretic therapy to control blood
pressure. Despite similar blood pressure responses in
the two groups at the end of one year, enalapril reduced
proteinuria more effectively than nifedipine. The
reduction in proteinuria occurred in patients with both
microalbuminuria and macroalbuminuria. Plasma
creatinine concentration increased in both groups but
to a greater extent in the enalapril group, particularly
in those requiring diuretics. Withdrawal from the
study was more common with enalapril, mostly
because of cough or inadequate control of blood
pressure. A longer period of treatment is required to
establish the significance of the reduction of proteinuria with enalapril and to determine whether this
will be translated into a beneficial effect on glomerular
filtration rate. Our study will continue for a further two
years. Until more information is available it is premature, in our view, to suggest that any one group of
antihypertensive drugs is superior to any other in the
treatment of non-insulin dependent diabetes associated with hypertension.
The study was sponsored by Merck, Sharpe, and Dohme.
We thank Ms Margaret Cheung and Ms Angela Wong, our
two research nurses for their dedication; Dr Denis Leung
from the Centre for Clinical Trials and Epidemiological
BMJ
VOLUME
View publication stats
305
24 OCTOBER 1992
Research, Chinese University of Hong Kong, for help with
the statistical analysis; and Dr J A J H Critchley, reader of the
department of clinical pharmacology, Chinese University of
Hong Kong, for critical appraisal of the manuscript.
I Parsing HH, Andersen AR, Smidt UM, Svendsen PAa. Early aggressive
antihypertensive treatment reduces rate of decline in kidney function in
diabetic nephropathv. Lanscet 1983;li: 1 175-9.
2 Hella J, Horacek V. Angiotensin II: preferential efferent constriction. Renal
Phvsiol 1986;9:357-65.
3 Jackson B, Johnston CI. The contribution of systemic hypertension to
progression of chronic renal failure in the rat remnant kidney: effect of
treatment with an ACE inhibitors or a calcium inhibitor. 7 Hperteoso
1 988;6:495-50 1.
4 vMyers BD, Meyer TW. Angiotensin-converting enzyme inhibitors in the
prevention of experimental diabetic glomerulopathv. Am J Kidnevs Dis
1 989;13:20-4.
5 Bj6irck S, Mulec H, Johnsen SA, N6rden G, Aurell M. Renal protective effect
of enalapril in diabetic nephropathy. BMJ 1992;304:339-43.
6 Zimmet P. Type 2 (non-insulin-dependent) diabetes-an epidemiological
oversiew. Diabetologia 1982;22:399-41 1.
7 Mogensen CE. Angiotensin converting enzyme inhibitors and diabetic
nephropathy. BAIJ 1992;304:327-8.
8 Melbourne Diabetic Nephropathy Study Group. Comparison between
perindopril and nifedipine in hypertensive and normotensive diabetic
patients with microalbuminuria. BAIM 1991;302:210-6.
9 Baba T, Murabavashi S, Takebe K. Comparison of the renal effects of ACE
inhibitors and calcium antagonist in hypertensive type 2 (non-insulindependent) diabetic patients with microalbuminuria: a randomized
controlled trial. Diabbetologia 1989;32:40-4.
10 Valvo E, Bedogna V, Casagrande P, Antiga L, Zamboni M, Bommartini F,
et al. Captopril in patients with type II diabetes and renal insufficiency:
systemic and renal hemodynamic alterations. AmJ1fed 1988;85:344-8.
11 Stornello M, Valvo EV, Vasques E, Leone S, Scapellato L. Systemic and renal
effects of chronic angiotensin converting enzyme inhibition with captopril in
hypertensive diabetic patients. _flvipts)tes 1989;7(suppl): PS65-7.
12 Ueda Y, Aoi W, Yamachika S, Shikaya T. Beneficial effects of angiotensinconverting enzyme inhibitor on renal function and glucose homeostasis in
diabetics with hypertension. Nephron 1990;55(suppl 1):85-9.
13 Matthews DM, Wathen CG, Bell D, Collier A, Roulston JE, Clarke BF, et al.
The use of captopril and captopril plus frusemide as antihypertensive agents
in non-insulin dependent diabetes. _Hton Hsperte)ts 1987;1: 19-23.
14 Stomello M, Valvo EV, Scapellato L. Persistent albuminuria in normotensive
non-insulin-dependent (type II) diabetic patients: comparative effects of
angiotensin-converting enzyme inhibitors and fl-adrenoceptor blockers.
Clint Sci 1992;82:19-23.
15 Ferrier C, Ferrari P, Weidmann P, Keller U, Beretta-Piccoli C, Riesen WF.
Anihypertensise therapy with calcium antagonist, verapamil and/or ACE
inhibitor enalapril in NIDDM patients. Diabetes Care 1991;14:91 1-4.
16 Ferder L, Daccordi H, Martello M, Panzalis M, Inserra F. Angiotensin
converting enzyme inhibitors versus calcium antagonists in the treatment of
diabetic hypertensive patients. Hyperte?isio?i 1 992;19(suppl II):237-42.
17 Rowe DJF, Dawnay A, Watts GF. Microalbuminuria in diabetes mellitus:
review and recommendations for the measurement of albumin in urine.
Anini Clii, Biochemi 1990;27:297-312.
18 Cheung CK, Swaminathan R. Automated immunoturbidimetric method for
the determination of retinol binding protein, prealbumin and transferrin in
urine. CliGu Biochemii 1989;22:425-7.
19 MacDonald D, Pang CP, Cockram CS, Swvaminathan R. Fructosamine
measurements in serum and plasma. Clin, Chewt Acta 1987;168:247-52.
20 McGuire GA, Price CP. A continuous monitoring spectophotometric method
for the measurement of ACE in human serum. Ami Cli?i Biocheni 1985;22:
204-10.
21 Gilchrist NL, Nicholls MG, Ewer rC, Livesey JH, Sainsbury R. A
comparison of long acting nifedipine and enalapril in elderly hypertensives:
arandomised, single-blind, cross-over study._ Hun, Hipertens 1988;2:33-9.
22 Veterans Administration Cooperative Study group on Antihypertensive
Agents. Comparison of propranolol and hydrochlorthiazide for the initial
treatment of hypertension. I. Results of short-term titration with emphasis
on racial differences in response.7AMA 1982;248:1996-2003.
23 Gambardella S, Frontoni S, Lala A, Felici MG, Spallone V, Scoppala A, et al.
Regression of microalbuminuria in type II diabetic hypertensive patients
after long-term indapamide treatment. Aiii HeartJf 1991;122:1232-8.
24 Payne RB. Creatinine clearance: a redundant clinical investigation. A,ill Cliii
Biochenii 1986;23:243-50.
25 Cleland JGF, Dargie HJ, Hodsman GP, Ball SG, Robertson JIS, Morton JJ,
et al. Captopril in heart failure. A double blind controlled trial. Br Heart J
1 984;52:530-5.
26 Mujais SK, Fouad FM, Textor SC, Tarazi RC, Bravo EL, Hart N, et al.
Transient renal dysfunction during initial inhibition of converting enzyme
in congestive heart failure. Br HeartJ 1984;52:63-7 1.
27 Nicholls MG. Overview: angiotensin, angiotensin converting enzyme
inhibition, and the kidney-congestive heart failure. Kidney lilt 1987;31
(suppl 20):S200-2.
28 Ferriere M, Lachkar H, Richard J-L, Bringer J, Orsetti A, Mirouze J.
Captopril and insulin sensitivity.'Ani Intern Med 1985;102:134-5.
29 Arauz-Pacheco C, Ramirez LC, Rios J, Raskin P. Hypoglycemia induced by
anglotensin-converting enzyme inhibitors in patients with non-insulindependent diabetes receiving sulfonylurea therapy. Anm J Med 1990;89:
811-3.
30 Chan JCN, Cockram CS. Drug-induced disturbances of carbohydrate
metabolism. Adverse Drug Reactions Toxicological Review 1991;10: 1-29.
31 Pollare T, Lithell H, Berne C. A comparison of the effects of hydrochlorothiazide and captopril on glucose and lipid metabolism in patients
with hypertension. NEnzglj7Med 1989;321:868-73.
32 Jauch KW, Hartl W, Guenther B, Wicklmayr M, Rett K, Dietze G. Captopril
enhances insulin responsiveness of forearm muscle tissue in non-insulin-
dependent diabetes mellitus. EurJCliiz Ittvest 1987;17:448-54.
33 Lai KN, Lui SF. Renin and erythropoietin. In: Robertson JIS, Nicholls MG,
eds. Renini-angiotensin systemn textbook. London: Gower (in press).
34 Kamper A-L, Nielsen OJ. Effect of enalapril on hemoglobin and serum
erythropoietin in chronic nephropathy. Scand 7 Cliii Lab Invest l990;50:
611-8.
(Accepted 2O August 1992)
985
�
 Ramasamyiyer Swaminathan
Ramasamyiyer Swaminathan