Paper 2
Paper 2
Uploaded by
Romah Cliquers LelledCopyright:
Available Formats
Paper 2
Paper 2
Uploaded by
Romah Cliquers LelledOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Paper 2
Paper 2
Uploaded by
Romah Cliquers LelledCopyright:
Available Formats
January 2013, Vol-4, Issue -1
Research Article ISSN NO:0976-6723
DESIGN, DEVELOPMENT AND EVALUATION OF FLOATING DRUG
DELIVERY SYSTEM USING FAMOTIDINE FOR THE TREATMENT OF
DUODENAL ULCER
PawanJalwal1*, AnupamaDiwan2
1.Ph.D. Scholar, Department of Pharmaceutical Sciences, Baba Mastnath University,
Asthal Bohar, Rohtak-124001
2.Professor and Programme Director, School of Pharmaceutical Sciences, ApeejayStya
University, Gurgaon, Haryana, India.
ABSTRACT
In the present work, floating gastro retentive formulation of Famotidine was formulated to sustained
release of Famotidine above its site of absorption.Famotidine is histamine H2 receptor antagonist in
treating gastric ulcer, duodenal ulcer, Zollinger Ellison syndrome, gastroesophegal reflux disease and
erosive esophagitis. It inhibits acid production by reversibly competing with histamine for binding to
H2 receptors on the basolateral membrane of parietal cells. It competitively inhibits histamine action
at all H2 receptors but their main clinical use is as inhibition of gastric acid secretion. It inhibited
histamine stimulation and gastrin stimulated acid secretion. It decreases both basal and food
stimulated acid secretion by 90% or more, but promote healing of duodenal ulcer. The swelling of
the polymers used (HPMC K15M, Ethyl cellulose, Xanthan Gum) were determined by water uptake
of the tablet. The percent swelling of the tablet was determined for 12 h at different time intervals.
Increase in percent swelling was found with increasing concentration of polymers.
Key words:Famotidine, Zollinger Ellison syndrome, duodenal ulcer, gastrin, histamine.
INTRODUCTION
competing with histamine for binding to H2
Famotidine is histamine H2 receptor antagonist
receptors on the basolateral membrane of
in treating gastric ulcer, duodenal ulcer,
parietal cells. It competitively inhibits
Zollinger Ellison syndrome, gastroesophegal
histamine action at all H2 receptors but their
reflux disease and erosive esophagitis. It
main clinical use is as inhibition of gastric
inhibits acid production by reversibly
acid secretion. It inhibited histamine
PawanJalwal et al Page 680
January 2013, Vol-4, Issue -1
stimulation and gastrin stimulated acid Alcohol, Practically insoluble in ether and in
secretion. It decreases both basal and food Ethyl Acetate. It is preserve in well closed
stimulated acid secretion by 90% or more, but container, Protected from light. The structure
promote healing of duodenal ulcer. The of famotidine is given below (figure 1)
chemical name of famotidine is
Figure 1: The structure of Famotidine
Propanimidamide, N-(aminosulfonyl)-3 [[[ 2-
[(diaminomethylene)-amino]-4- thiazolyl]
methyl] thio]- [ 1-amino-3- [[[2- [
(diaminomethylene) amino]-4- [thiazolyl]-
methyl] thio] propylidene] sulfamide. The The major therapeutic use of famotidine is
molecular formula and molecular weight of promoting healing for gastric and duodenal
famotidine are C8H15N7O2S3 and 337.445 ulcer, treatment of uncomplicated
respectively. It is a white or Yellowish- white, Gastroesophageal reflux disease (GERD) and
crystalline powder or crystals having melting for prophylactic treatment of stress ulcer. In
point is 163-169oC. It is freely Soluble in addition, it employed in combination with
Dimethyl Formamide and in Glacial Acetic antibiotics to treat infection with Helicobector
Acid, slightly soluble in Methyl Alcohol, very pylori i.e in treatment of Gastritis.
slightly soluble in water and in Dehydrated
Pharmacokinetics
Table 1: Pharmacokinetics of Famotidine
Bioavailability 40-45%
Plasma Half Life 2.5h-3.5hrs.
Plasma Protein Binding 15- 20%
Peak Plasma Concentration
1- 3 hours
(Cmax)
Excretion Renal Excretion (65-70%)
Metabolic Excretion ( 30-35%)
Renal Clearance 250-450ml/min
Drug Interaction It does not inhibit hepatic microsomal enzyme CYTP450 system and
hence does not interact with drugs which are substrate for CYTP450
systems like Warfarin, Pheytoin, Quinidine, Caffiene etc. It does not
block androgen receptors and do not causeGynaecomastia and
impotence like Cimetidine.
MATERIAL AND METHODS Dibasic Calcium Phosphate were received as a
gift from Central Drug House, Mumbai.
Famotidine was received as a gift sample from
Povidone and HCl were received as a gift
BelcoPharma, Bahadurgarh, Haryana, India.
sample from Merck SpecialitiesPvt Ltd,
Hypromellose (HPMC), Xanthan Gum, Ethyl
Mumbai. Isopropyl Alcohol was perchased
Cellulose, Microcrystalline Cellulose, and
from Nice Chemicals Pvt Ltd, Cochin.
PawanJalwal et al Page 681
January 2013, Vol-4, Issue -1
Magnesium stearate and talc were perchased 2. The ingredients were weighed accurately
as a gift from Qualikems Fine Chemicals Pvt and mixed thoroughly.Tablets of Famotidine
Ltd, Delhi. Lactose was perchased from were prepared by direct compression& wet
Central Drug House (P) Ltd. New Delhi, compression method and their release profiles
India.All other ingredients used were of were compared to select the manufacturing
analytical grade. process for further studies.
Experimental methods Selection of manufacturing process
Batches were prepared with HPMC K15M
Preparation of Floating Tablets of Famotidine
using wet granulation method and direct
The composition of different formulations of compression method and their release profiles
Famotidine floating tablets was shown in table were compared. Formula is given in Table 2.
Table 2: Formulation of Famotidine using HPMC K15M with direct compression and wet
granulation methods
Batch No. F1 (Wet Granulation) F2 (Direct Compression)
Ingredients Name mg/tab mg/tab
Famotidine 80 80
HPMC K15M 90 90
Sodium bicarbonate 70 70
Citric Acid 30 30
Lactose 109 -
Microcrystalline Cellulose - 124
Povidone 15 -
Isopropyl Alcohol q.s. -
Magnesium Stearate 3 3
Talc 3 3
Total 400 400
Formulation of batches with different ratio proportion of Sodium bicarbonate and Citric
of Sodium bicarbonate and Citric acid Acid and their release profiles were compared.
Batches were prepared with HPMC K15M Formula is given in Table 3
using wet granulation method to select the
Table 3: Formulation of batch with different ratio of Sodium bicarbonate and Citric acid
Batch No. F1 F3 F4
Ingredients mg/tab mg/tab Mg/tab
Famotidine 80 80 80
HPMC K15M 90 90 90
Sodium bicarbonate 70 80 90
Citric Acid 30 20 10
PawanJalwal et al Page 682
January 2013, Vol-4, Issue -1
Lactose 109 109 109
Povidone 15 15 15
Isopropyl Alcohol q.s. q.s. q.s.
Talc 3 3 3
Magnesium Stearate 3 3 3
Total 400 400 400
Preparation of trial batches with different polymers with different concentration
Formulation batches were prepared using different polymers (HPMC K15M, Xanthan gum, and
Ethyl Cellulose). Formula is given in Table 4
Table 4: Formulation of different batches with different polymer concentration
Batch no. F4 F5 F6 F7 F8 F9 F10
Ingredients mg/tab mg/tab mg/tab mg/tab Mg/tab mg/tab mg/tab
Famotidine 80 80 80 80 80 80 80
HPMC K15M 90 110 130 90 90 90 90
Ethyl Cellulose - - - - - 25 40
Xanthan Gum - - - 25 40 - -
Sodium 90 90 90 90 90 90 90
bicarbonate
Citric Acid 10 10 10 10 10 10 10
DCP - - - 84 69 84 -
Lactose 109 89 69 - - - 69
Povidone 15 15 15 15 15 15 15
Isopropyl q.s. q.s. q.s. q.s. q.s. q.s. q.s.
Alcohol
Talc 3 3 3 3 3 3 3
Magesium 3 3 3 3 3 3 3
Stearate
Total 400 400 400 400 400 400 400
Effect of various diluents with their elastic and Lactose and compared to select the best
or plastic properties: diluent for further formulations. Formula is
Formulations were prepared using different given in Table 5.
diluents such as Dibasic calcium phosphate
PawanJalwal et al Page 683
January 2013, Vol-4, Issue -1
Table 5: Formulation of Famotidine by Bulk density (g/ml) = Weight of powder (g)
using different diluents with their elastic or / Bulk volume (ml)
plastic properties Tapped density (TD)
Batch no. F8 F11 After the initial volume Vawas observed, the
Ingredients mg/tab mg/tab cylinder containing the sample was
Famotidine 80 80 mechanically tapped by raising the cylinder
HPMC K15M 90 90 and allowing it to drop under its own weight
Xanthum Gum 40 40 onto a hard surface from the height of 2.5 cm
Sodium 90 90 at 2 second intervals. The tapping was
bicarbonate continued until no further changes was
Citric Acid 10 10 observed in volume was noted and tapped
Lactose 69 - volume Vb was noted. The tapped density was
DCP - 69 calculated from the formula given below:
Povidone 15 15 Tapped Density (g/ml) = Weight (g) /
Isopropyl Alcohol q.s. q.s. Tapped volume (ml)
The flow properties of granules before
Talc 3 3
compression were characterized in terms of
Magnesium 3 3
angle of repose, Carrs index and Hausner
Stearate
ratio. For determination of angle of repose, the
Total 400 400
granules were poured through the walls of a
funnel, which was fixed at a position such that
In Vitro evaluation
its lower tip was at a height of exactly 2.0cm
1. Evaluation of granules
above hard surface. The granules were poured
Bulk Density (BD)
till the time when upper tip of the pile surface
Bulk density was determined according to
touched the lower tip of the funnel. The tan-1
Method I as reported in USP XXXII. The drug
of the (height of the pile/ radius of its base)
powder was passed through BSS # 25 screens
gave the angle of repose. Granules were
to break up agglomerates. The drug powder
poured gently through a glass funnel into a
was introduced into a dry 100 ml tarred
graduated cylinder cut exactly to 10ml mark.
measuring cylinder. The powder was then
Excess granules were removed using a spatula
carefully labeled, if necessary, without the
and the weight of the cylinder with pellets
application of force and the unsettled volume
required for filling the cylinder volume was
(bulk volume) was noted. The weight of the
calculated. The cylinder was then tapped from
powder was also noted and the bulk density
a height of 2.0cm until the time when there
was calculated as:
PawanJalwal et al Page 684
January 2013, Vol-4, Issue -1
was no more decrease in the volume. Bulk Carrs Index (%Compressibility Index) =
density and tapped density were calculated. [100 (TD-BD)]/TD
Hausners Ratio = Tapped density / Bulk
density
Table 6: Results of flow properties of granules
Batch No. Bulk Tapped Angle of Hausners Carrs index
Density Density Repose ratio
F1 0.392 0.542 37.8,(fair) 1.38,( poor) 27.67,( poor)
F2 0.388 0.573 35.6, (fair) 1.47, (poor) 32.28, (poor)
F3 0.390 0.593 38.2, (fair) 1.52, (poor) 34.23, (poor)
F4 0.398 0.485 39.4, (fair) 1.21, (fair) 17.9, (fair)
F5 0.372 0.492 36.3, (fair) 1.32, (passable) 24.3, (passable)
F6 0.380 0.511 34.2, (good) 1.34, (passable) 25.6, (poor)
F7 0.386 0.495 37.3, (fair) 1.28, (passable) 22.02, (passable)
F8 0.394 0.482 33.5, (good) 1.22, (fair) 18.25, (fair)
F9 0.381 0.493 33.8, (good) 1.29, (passable) 22.7, (passable)
F10 0.376 0.532 36.2, (fair) 1.41, (poor) 29.32, (poor)
F11 0.385 0.480 37.7, (fair) 1.24, (fair) 19.7, (fair)
2. Evaluation of colon targeted matrix drum for a fixed time (100 revolutions) and
tablets weighed (W) again. Percentage friability was
(1) Weight variation tests of tablets calculated from the loss in weight as given in
Weight variation of the formulation was equation as below. The weight loss should not
performed as per USP. 20 tablets were be more than 1% w/w.
weighed using a Scale-Tec electronic balance % Friability = (W0-W)/W0 100
individually and compared with the average (4) Thickness Test:
weight of the twenty tablets. The Thickness of the tablets was determined
(2) Hardness of the tablets by using verniercalliper. Five tablets were
The hardness of five tablets was determined used, and average values were calculated.
using Pfizer type hardness tester and the (5) Assay:
average values were calculated. Five tablets were weighed and triturated, from
(3) Friability of tablets that transfer an accurately weighed portion of
The friability of the tablets was measured in a the powder equivalent to about 80 mg of
Roche friabilator. Tablets of a known weight Famotidine to a 100 ml volumetric flask
(W0) or a sample of tablets were dedusted in a
PawanJalwal et al Page 685
January 2013, Vol-4, Issue -1
containing 0.1 N HCl and then concentration On immersion in 0.1 N HCl solutions (pH 1.2)
is measured at maxi.e. 265 nm. at 37 C, all the tablets first sank in the release
(6) In vitro buoyancy studies medium and then they float to the surface. All
the tablets remained buoyant up to 24 h.
Table 7: Results of evaluation of parameters of tablets from different batches
Batch Average Thickness Friability Hardness Assay Floating lag Floating
no. weight(mg) (mm) % (kp) time (sec)s Duration (h)
F1 403 3.7 0.04 5 97.62 120 24 h
F2 398 4.2 0.06 6 98.87 135 24 h
F3 402.3 4.0 0.03 4 97.37 110 24 h
F4 399 3.8 0.06 6 99.65 90 24 h
F5 397 3.5 0.02 5 101.25 120 24 h
F6 401 3.6 0.07 6 98.72 240 24 h
F7 399 3.7 0.05 6 99.56 90 24 h
F8 399.6 3.8 0.03 5 101.12 60 24 h
F9 401 4.2 0.01 4 97.89 40 24 h
F10 402 3.5 0.04 5 102.67 120 24 h
F11 401.3 3.7 0.02 4 98.52 30 24 h
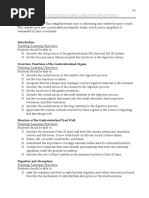
(7) Swelling Behavior studies concentration of polymers. The percent
The swelling of the polymers used (HPMC swelling of F11 was found to be higher
K15M, Ethyl cellulose, Xanthan Gum) were (131.20%) than that of other formulations
determined by water uptake of the tablet. The (Fig. 2). The percent swelling increased
percent swelling of the tablet was determined gradually up to 12 h. Results of swelling index
for 12 h at different time intervals. Increase in shown in Table 8
percent swelling was found with increasing
Table 8: Results of swelling index
Time F3 F4 F5 F6 F7 F8 F9 F10 F11
(hr)
1 52.11 55.47 54.87 47.79 59.66 60.65 57.32 59.21 60.65
2 59.17 62.20 59.60 56.89 67.25 69.52 62.58 69.52 72.56
3 67.81 66.54 66.03 67.08 72.44 76.12 67.96 75.01 79.32
4 75.63 79.28 79.8 75.44 78.32 80.01 77.63 80.35 88.01
5 86.06 88.06 87.70 86.66 83.05 88.47 84.01 86.22 95.09
6 - 96.50 96.80 95.05 89.12 93.94 89.52 90.56 100.51
7 - - 115.02 109.44 93.26 98.20 95.02 96.04 106.84
8 - - 125.54 116.6 99.54 106.21 103.12 100.55 111.36
9 - - - 126.52 108.56 112.05 109.75 106.51 119.20
PawanJalwal et al Page 686
January 2013, Vol-4, Issue -1
10 - - - 128.60 118.62 120.61 117.26 110.24 124.25
11 - - - - - 125.41 - 123.42 129.05
12 - - - - - 129.50 - - 131.20
Figure 2:Swelling indices of various batches Vs. Time
140
120 F3
F4
100 F5
% Swelling
80 F6
F7
60
F8
40 F9
F10
20
F11
0
0 5 10 15
Time (hrs)
(8) Dissolution studies: RPM : 50 rpm
Dissolution studies were conducted to Time point : 1, 2, 3, 4, 5, 6, 7, 8, 9,
determine the release pattern of the product. 10, 11, 12 hrs.
Dissolution test for Famotidine was carried Temperature : 37C 0.5C
out as per USP method for dissolution test for Volume of sample withdrawal: 10 ml
tablets using apparatus-II. maxfor absorbance : 265 nm
Dissolution parameters The drug release profiles obtained were fitted
Medium : 0.1 N HCl (pH 1.2) into several mathematical models and drug
Volume : 900 ml release mechanism was determined from the
Apparatus : USP-II (Paddle) matrix tablet.
Table 9: Release profiles of formulations using different polymers in different concentrations
Time % Drug release
(hr) F4 F5 F6 F7 F8 F9 F10
1 52.1 25.27 22.14 26.14 25.62 26.14 29.50
2 65.7 40.67 40.32 34.21 32.32 33.37 38.11
3 76.9 49.90 46.71 45.58 48.66 47.06 45.16
4 85.4 60.09 58.32 48.50 59.47 56.49 58.17
5 93.7 68.99 68.54 52.31 65.24 60.21 63.25
6 100.7 78.21 75.42 62.91 69.89 68.37 68.71
7 - 87.44 85.46 69.40 76.27 78.83 74.21
8 - 98.55 90.50 75.30 82.60 89.40 77.65
9 - - 95.63 85.40 89.21 93.20 88.80
PawanJalwal et al Page 687
January 2013, Vol-4, Issue -1
10 - - 99.50 92.13 93.12 99.93 97.40
11 - - - 99.83 98.56 - 105.51
12 - - - - 103.36 - -
Fig 3: Dissolution profile of formulations with different Polymers
120
100 F4
F5
% drug release
80
F6
60 F7
F8
40
F9
20 F10
0
0 5 10 15
Time (hr)
SUMMARY blood flow, prostaglandins(PG), nitric oxide).
Gastric ulcer, one of the most widespread, is The goals of treating peptic ulcer disease are
believed to be due to an imbalance between to relieve pain, heal the ulcer and prevent ulcer
aggressive and protective factors. The gastric recurrence.
mucosa is continuously exposed to potentially Various types of treatment are available for
injurious agents such as acid, pepsin, bile the treatment of gastric ulcer Proton pump
acids, food ingredients, bacterial products inhibitor, Anticholinergics, Antacids,
(Helicobacter pylori) and drugs. These agents Prostaglandin analogues and H2
have been implicated in the pathogenesis of Antihistamines. H2 antihistamines are widely
gastric ulcer, including enhanced gastric acid used in the management of gastric ulcer,
and pepsin secretion, inhibition of Zollinger- Ellison Syndrome and
prostaglandin synthesis and cell proliferation Gastroesophgeal reflux disease. Three types of
growth, diminished gastric blood flow and histamine receptor are known H1, H2, and H3.
gastric motility. Drug treatment of peptic H1 is located in smooth muscles and blood
ulcers is targeted at either counteracting vessels. H2 receptors are located in gastric
aggressive factors (acid, pepsin, active glands, heart and uterus. H3 receptors are
oxidants, platelet aggravating factor PAF, located in brain, lungs and spleen.
leukotrienes, endothelins, bile or exogenous Controlled release drug delivery systems are
factors including NSAIDs) or stimulating the developed to modulate the apparent absorption
mucosal defences (mucus, bicarbonate, normal or alter the site of release of drugs, in order to
PawanJalwal et al Page 688
January 2013, Vol-4, Issue -1
achieve specific clinical objectives that cannot prolongation in release of Famotidine with
be attained with conventional dosage forms. HPMC: Xanthum gum. Concentration of
Unlike immediate-release preparations, in sodium bicarbonate and citric acid affect the
which the total amount of drug is rapidly floating lag time and all the formulation float
available after ingestion, controlled-release upto 24 hours. Effect of diluent on drug
formulations are designed to release specific release was also studied by comparing lactose
amounts of drug over a certain time period. and dibasic calcium phosphate. Dibasic
The major benefits include improved calcium phosphate had maximum retarding
pharmacokinetics (e.g., less variation between capacity followed by lactose. The release
peaks and troughs), less frequent dosing, and kinetics of all the batches were carried out and
improved patient adherence optimized it was found final batch followed Higuchi
performance, a greater selectivity of activity or kinetic model. The optimized formulation has
new indications. drug release profile up to 12 hours.
In present work an attempt was made to CONCLUSION
prepare the Floating Tablet of Famotidine 1. The absorbance maxima of Famotidine
using different polymers by wet granulation were found as 265 nm which was selected
and direct compression method with Lactose, for UV analysis.
DCP and MCC as diluents, citric acid and 2. The physical compatibility study at
Sodium bicarbonate as gas generating agent. 40oC/75% RH showed that Famotidine
It was found that wet granulation method and excipients used found to be
facilitated greater efficiency in controlling physically compatible.
Famotidine release behavior from the 3. FTIR spectra data showed that
matrices. Hence, all further formulations were Famotidine and excipients used found to
prepared with wet granulation technique. be compatible.
FTIR studies shows that there was no 4. Melting point of Famotidine was found to
incompatibility between drug, polymer and be 165oC.
co-excipients. All the prepared formulations 5. Formulation was prepared with two
were evaluated for hardness, friability, processes i.e. direct compression and wet
uniformity of weight, thickness, in vitro granulation; it was found that wet
buoyancy study, assay and in vitro release. granulation method facilitated greater
Batches were prepared by HPMC and HPMC efficiency in controlling Famotidine
K15M+ EC, HPMC K15M+Xanthum gum. release behaviour from the matrices as
Ratio of polymers in formulation played major compared to direct compression.
role in controlling the release rate of
Famotidine, which is evident from the
PawanJalwal et al Page 689
January 2013, Vol-4, Issue -1
6. Characterization of granules prepared by Kanig JL. Eds. 3rd; Varghese Pub.
selected manufacturing processes like House: Bombay, 2003. P. 293 294.
bulk density, tapped density, Carrs 3. Das NG, Das SK. Controlled-release of
index, Hausners ratio, Angle of repose oral dosage forms. Pharm. Technol. 2010.
was done and found to have good flow 2(2): 90-96.
and compressibility. 4. Brahamanker DM, Jaiswal SB.
7. The tablets prepared were found to be Biopharmaceutics and
within the limits with respect to hardness, Pharmacokinetics.VallabhPrakashan:
average weight, %friability and thickness. 2004. Delhi. P. 335.
8. From the different polymers used in 5. Robinson JR, Vincent HL. Controlled
polymer selection batches, combination drug delivery: Fundamentals and
of HPMC and Xanthum gum were found applications, New York: Marcel Dekker
to be satisfactory. Inc, Vol. 29; 2002. P. 3-61.
9. Dibasic calcium phosphate was found to 6. Patil J M, Hirlekar R S, Gide P S, Kadam
be the best diluent in controlling the V J. Trends in Floating Drug Delivery
release rate of drug and thus helps in Systems. J Scientific& Industrial
extending the release profile. Res.2006; 65:11-21.
10. Under the study of kinetic models, five 7. Etyan AK, Eran L, Michel F. Hoffman A.
models have been studied namely Zero Expandable gastroretentive dosage forms.
Order, First Order, Higuchi, Hixon- J. Cont. Rel.2003. 909: 143-162.
Crowell, Korsmeyer-Peppas model. It 8. Shiva Kumar HG, VishakanteGowda D,
was found that the drug release model of Kumar Pramod T.M., Floating Controlled
final batch followed Higuchi kinetic Drug Delivery System for Prolonged
model (having maximum R2 value of Gastric Residence: A Review. Indian J.
0.9966). pharm. Educ. 2004. 38(4) : 172-179
REFERENCES 9. Jain NK. Pharmaceutical product
1. Chien YW. Oral drug delivery and development. 2nd Ed. Bangalore & New
delivery systems, Fundamentals of Rate Delhi: CBS publisher, 2004. P.40-45.
Controlled Drug Delivery. In: Novel 10. Ponchel G, Irache JM. Specific and non-
Drug Delivery Systems. New York: specific bioadhesive particulate system
Marcel Dekker Inc; 1992. P. 43-137 for oral delivery to the gastrointestinal
2. Banker GS, Anderson NR. Tablets: The tract. Adv Drug Deliv Rev. 1998; 34:
theory and practice of industrial 191-219.
pharmacy.Lachman L, Lieberman HA, 11. Srivastav M., Prabhakar B., Omray A.
Extended Release Tablet Technologies-
PawanJalwal et al Page 690
January 2013, Vol-4, Issue -1
Matrix, Melt Granulation and Delivery System for Prolonged Gastric
Multiparticulates: An Overview. Residence: A Review. Indian J. pharm.
International Journal of Universal Educ. 2004. 38(4): 172-179.
Pharmacy and Life Sciences. 2011. 1(2): 19. Narang N, An updated review on:
331-354. Floating Drug Delivery system; Int.
12. Sampath KP, Bhownik D, Chandira M, Journal of Applied Pharmaceutics. 2011.
Tripathi KK. Innovations in Sustained 3(1): 1-7.
Release Drug Delivery System and its 20. Chen J, Blevins WE, Park H, Park K.
Market Opportunities. Journal of Gastric retention properties of
Chemical and Pharmaceutical Research. superporous hydrogel compositions. J
2010. 2(1): 349-360. Control Release. 2000; 65: 73-82.
13. Ansel HC, Allen LV, Popovich NC, 21. Arunachalam A, Karthikeyan M, Konam
Pharmaceutical dosage forms and drug K, Pottabathula HP, Sethuraman S,
th
delivery systems, 7 Ed. Lippincott Ashutoshkumar S, Manidipa S. Floating
Williams and Wilkins; Baltimore; 2000. Drug Delivery System: A Review; Int.
P. 231-240. Jounral of Res. Pharm. Sci. 2011. 2(1):
14. Jayanthi B, Manna PK, Madhusudhan S, 76-83.
Mohanta GP, Manavalan R. Oral 22. Saha SH, Patel JK, Pundarikakshudu N,
Extended Release Product: An Overview. Patel NV. An Overview of
Applied Journal of Pharmaceutical Gastroretentive floating drug Delivery
Science. 2011. 1(2): 50-55. system. Asian Journal of Pharmaceutical
15. Deshpande A A, Shah NH, Christoper Sciences 2009. 4(1): 65-80.
TR, Malik W. Development of Novel 23. Nayak AK, Maji R, Das B.
Controlled Release System for Gastric Gastroretentive Drug Delivery System: A
Retention. Pharm. Res.1997. 14: 815-819. Overview. Asian Journal of
16. Yeole PG, Khan S, Patel VF. Floating Pharmaceutical and Clinical Research.
Drug Delivery System: Need and 2010. 3(1) : 2-10
Development. Ind. J. Pharm. Sci. 2005. 24. Sanjay S, Joshi V, Barpete KP,
67: 265-272. Gastroretentive Drug Delivery System:
17. Arora S, Ali J, Ahuja A, Khar RK, Current Approaches. Joural of Pharmacy
Baboota S. Floating drug delivery system: Research. 2009.2 (5) : 881-886
A Review. AAPS Pharm Sci. Tech. 2005. 25. Jamil F, Kumar S, Sharma S,
6 (3):E372- E373. Vishvakarma P., Singh L. Review on
18. Shivakumar HG, Vishakante GD, Kumar Stomach Specific Drug Delivery System:
Pramod TM, Floating Controlled Drug Development and Evaluation.
PawanJalwal et al Page 691
January 2013, Vol-4, Issue -1
International Journal of Research in 28. Gangadharappa HV, Kumar Pramod TM,
Pharmaceutical and Biomedical Kumar Shiva HG. Gastric Floating Drug
Sciences.2011. 2(4): 1427-1433. delivery System: A Review. Indian J.
26. Surana AS, Kotecha RK. An overview on Pharm. Educ. 2007. 41(4) : 295-304
various approaches to oral controlled drug 29. Vanshiv DS, Joshi PH, Sherje A, Phale
delivery system via gastroretention. Int J AAS, Dhat PS. Gastroretentive Drug
Pharm Sci Review and Res. 2010; 2(2): Delivery System: Review. Journal of
68-72. Pharmacy Research. 2009. 2(12): 1879-
27. Mathur P, Saroha S, Syan N, Verma S, 1885.
Nanda S, Valecha V. An overview on 30. Jain NK. Pharmaceutical product
recent advancements and developments in development. 2nd Ed. Bangalore & New
gastroretentive buoyant drug delivery Delhi: CBS publisher, 2004. P.40-45.
system. Pelagia Research Library. 2011. 2
(1) : 161-169
Correspondence Address:
PawanJalwal
Department of Pharmaceutical Sciences,
Baba Mastnath University,
Asthal Bohar, Rohtak-124001
E-mail- pawan_jalwal@rediffmail.com
Mobile No. 09812875605
PawanJalwal et al Page 692
You might also like
- Nclex DiseasesDocument6 pagesNclex Diseasesshangguanlongkui95% (21)
- GI Long Notes PDFDocument88 pagesGI Long Notes PDFQueenie WongNo ratings yet
- Grupo+6+Formulation and Evaluation of Famotidine+%285%29Document5 pagesGrupo+6+Formulation and Evaluation of Famotidine+%285%29Denisse ÁngelNo ratings yet
- Formulation and Evaluation of Mefenamic Acid Ointment Using Penetration EnhancersDocument5 pagesFormulation and Evaluation of Mefenamic Acid Ointment Using Penetration EnhancersIndradewiNo ratings yet
- Formulation and Evaluation of Mefenamic Acid Ointment Using Penetration EnhancersDocument5 pagesFormulation and Evaluation of Mefenamic Acid Ointment Using Penetration EnhancersIndradewiNo ratings yet
- Development and in Vitro-In Vivo Evaluation of Gastro Retentive Drug Delivery of Nizatidine Using Natural and Semi - Synthetic PolymersDocument17 pagesDevelopment and in Vitro-In Vivo Evaluation of Gastro Retentive Drug Delivery of Nizatidine Using Natural and Semi - Synthetic PolymersShyamlaNo ratings yet
- Attachment PDFDocument10 pagesAttachment PDFHEPHZIBAH CHILAKANo ratings yet
- Floating Tablets of FamotidineDocument8 pagesFloating Tablets of FamotidineRomah Cliquers LelledNo ratings yet
- Bulk Density Dan Tapped Density of MetforminDocument7 pagesBulk Density Dan Tapped Density of MetforminAtikah Ip Ananda MulyonoNo ratings yet
- Formulation and Evaluation of Cimetidine Floating Matrix TabletsDocument15 pagesFormulation and Evaluation of Cimetidine Floating Matrix TabletsIndahsariNo ratings yet
- 20.Md Musharraf Ali and V.saikishoreDocument9 pages20.Md Musharraf Ali and V.saikishoreBaru Chandrasekhar RaoNo ratings yet
- Formulation and Evaluation of Thermosensitive Intranasal in Situ Gel of Sumatriptan Succinate by Using A Blend of PolymersDocument9 pagesFormulation and Evaluation of Thermosensitive Intranasal in Situ Gel of Sumatriptan Succinate by Using A Blend of PolymersabikeshNo ratings yet
- 70-Article Text-132-1-10-20190708Document12 pages70-Article Text-132-1-10-20190708Daisy Arora KhuranaNo ratings yet
- Formulation & Evaluation of SMEDDS of Low Solubility Drug For Enhanced Solubility & DissolutionDocument18 pagesFormulation & Evaluation of SMEDDS of Low Solubility Drug For Enhanced Solubility & DissolutionJohn PaulNo ratings yet
- Formulation Development and Evaluation of Immediate Release Tablets Containing Antihypertensive Agent Amlodipine Besylate and ValsartanDocument8 pagesFormulation Development and Evaluation of Immediate Release Tablets Containing Antihypertensive Agent Amlodipine Besylate and ValsartanDược K45 Trần Dũng TâmNo ratings yet
- JDDR 139Document11 pagesJDDR 139Earthjournal PublisherNo ratings yet
- Metformin Drug ProfileDocument9 pagesMetformin Drug ProfileSalman ShaikhNo ratings yet
- Ijcpa 2013002Document3 pagesIjcpa 2013002AHMED MOHAMMED MAHMOUD MUSTAFANo ratings yet
- Formulation of Solid Dispersions For EnhDocument7 pagesFormulation of Solid Dispersions For Enhpratikdhotre211No ratings yet
- Nanoemulsion CapsanthinDocument11 pagesNanoemulsion CapsanthinRuang BazaarNo ratings yet
- Editorajpcr,+32 AJPCR 35690 RADocument9 pagesEditorajpcr,+32 AJPCR 35690 RAtaikhoan217No ratings yet
- Formulation and In-Vitro Evaluation of Controlled Release Transdermal Drug Delivery System of Simvastatin A Model Hypocholesterolemia DrugDocument6 pagesFormulation and In-Vitro Evaluation of Controlled Release Transdermal Drug Delivery System of Simvastatin A Model Hypocholesterolemia DrugPRASANTA KUMAR MOHAPATRANo ratings yet
- Fulcincap PDFDocument8 pagesFulcincap PDFAnonymous jhUUAkErONo ratings yet
- Carrageenan, A Review PDFDocument19 pagesCarrageenan, A Review PDFgonzaloNo ratings yet
- CR TabletDocument13 pagesCR TabletKhánh ToànNo ratings yet
- Admin, Journal Manager, IJCPR-990 (Repaired)Document9 pagesAdmin, Journal Manager, IJCPR-990 (Repaired)sadafNo ratings yet
- 2459 FullDocument18 pages2459 FullEnggerianiNo ratings yet
- Iota Carragenan Struktur KimiaDocument8 pagesIota Carragenan Struktur KimiasejatiirpanNo ratings yet
- Scientific Discussion: 1/16 ©EMEA 2007Document16 pagesScientific Discussion: 1/16 ©EMEA 2007Marisa OktavianaNo ratings yet
- A Comparison of i So and a Acc MethodsDocument8 pagesA Comparison of i So and a Acc MethodsJacqueline Capataz TafurNo ratings yet
- Improvement Dissolution Rate and Bioavailability of Simvastatin TabletDocument10 pagesImprovement Dissolution Rate and Bioavailability of Simvastatin TabletTaufik Rizki RamdamiNo ratings yet
- Solid Dispersion ........Document31 pagesSolid Dispersion ........Rishikesh ChakorNo ratings yet
- Design and Characterization of MucoadhesDocument6 pagesDesign and Characterization of Mucoadheskamleshkpatel114No ratings yet
- Formulation Development and In-Vitro Evaluation of Bucoadhesive Tablet of Chlorpheniramine Maleate and Phenylephrine Hydrochloride in Combined Dosage FormDocument11 pagesFormulation Development and In-Vitro Evaluation of Bucoadhesive Tablet of Chlorpheniramine Maleate and Phenylephrine Hydrochloride in Combined Dosage FormNeerajNo ratings yet
- Alhamdany, A. T.10 (6), 119. Doi10.22159ijap.2018v10i6.28687Document9 pagesAlhamdany, A. T.10 (6), 119. Doi10.22159ijap.2018v10i6.28687Maria CamiloNo ratings yet
- Pratik - Dhotre - Project GMC111Document18 pagesPratik - Dhotre - Project GMC111pratikdhotre211No ratings yet
- Mechanism of Gentamicin Sulphate Release in Nanocomposite Hydrogel Drug Delivery SystemsDocument4 pagesMechanism of Gentamicin Sulphate Release in Nanocomposite Hydrogel Drug Delivery SystemsAnonymous l5jiLwO15No ratings yet
- Production of Amino Acids (Glutamate)Document48 pagesProduction of Amino Acids (Glutamate)Shiv SiddhNo ratings yet
- Studies On Formulation and Evaluation of Bilayered Tablets of CurcuminDocument7 pagesStudies On Formulation and Evaluation of Bilayered Tablets of CurcuminMasayu Dinahya DiswantiNo ratings yet
- Ijpir 16 403 - 98 110Document13 pagesIjpir 16 403 - 98 110JeffNo ratings yet
- Jurnal KesehatanDocument6 pagesJurnal KesehatanFikaPermatasaryNo ratings yet
- Formulation and in Vitro Evaluation of Readyuse Suspension of Ampiillin TrihydrateDocument4 pagesFormulation and in Vitro Evaluation of Readyuse Suspension of Ampiillin TrihydrateREfli Eko FebriantoNo ratings yet
- Formulation and in Vitro Evaluation of Mucoadhesive Tablets of Ofloxacin Using Natural GumsDocument6 pagesFormulation and in Vitro Evaluation of Mucoadhesive Tablets of Ofloxacin Using Natural Gumsabdi100% (1)
- Development and Evaluation of An In-Situ Gelling Liquid Dosage Form of An Anti - Hypertensive DrugDocument9 pagesDevelopment and Evaluation of An In-Situ Gelling Liquid Dosage Form of An Anti - Hypertensive DrugInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- PectinasasDocument9 pagesPectinasascarolasbdNo ratings yet
- 2019 - Encapsulation of Flaxseed Oil Extract in Alginate - Salep System by Ionic GelationDocument10 pages2019 - Encapsulation of Flaxseed Oil Extract in Alginate - Salep System by Ionic GelationAyu Nila RatnaNo ratings yet
- Amino AcidDocument47 pagesAmino AcidYuppie RajNo ratings yet
- Medical Research and Clinical Case ReportsDocument5 pagesMedical Research and Clinical Case ReportsDrkrishnasarma pathyNo ratings yet
- Formulation & Evaluation of Sustained Release Microsphere of PropanololDocument11 pagesFormulation & Evaluation of Sustained Release Microsphere of PropanololAlfitaRahmawatiNo ratings yet
- Formulation and Evaluation of Floating Matrix Tablet of Losartan For Gastro-Retentive Drug DeliveryDocument6 pagesFormulation and Evaluation of Floating Matrix Tablet of Losartan For Gastro-Retentive Drug DeliveryRaja AbhilashNo ratings yet
- 1214 Full PDFDocument6 pages1214 Full PDFFeslyAnugerahAriestaPayungNo ratings yet
- Acetazolamide PPT@Document39 pagesAcetazolamide PPT@SREEDHAR ATTLANo ratings yet
- Formulation, In-Vitro and In-Vivo Evaluation of Enteric Coated Pellets of Substituted Benzimidazole Proton Pump InhibitorDocument11 pagesFormulation, In-Vitro and In-Vivo Evaluation of Enteric Coated Pellets of Substituted Benzimidazole Proton Pump InhibitorkavitaNo ratings yet
- 18.rajiv Kumar Parminder Nain Jaspreet Kaur Vipin Saini and Varinder SoniDocument11 pages18.rajiv Kumar Parminder Nain Jaspreet Kaur Vipin Saini and Varinder Sonidesi imastutiNo ratings yet
- 3420 PDFDocument11 pages3420 PDFreskyNo ratings yet
- Merck Rebrand - 100908 - 1907Document5 pagesMerck Rebrand - 100908 - 1907Paula BautistaNo ratings yet
- 1989 4 Final Report On The Safety Assessment of CaptanDocument38 pages1989 4 Final Report On The Safety Assessment of CaptanDavid SilverNo ratings yet
- Obat Git 2009Document32 pagesObat Git 2009Vian AprilyaNo ratings yet
- Phytic Acid in Peanut (Spectro)Document4 pagesPhytic Acid in Peanut (Spectro)Yap Poh SiewNo ratings yet
- Antiglycemic and Antioxidant Activity of Terminalia Chebula Fruits ProteinDocument5 pagesAntiglycemic and Antioxidant Activity of Terminalia Chebula Fruits ProteinInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Food Carotenoids: Chemistry, Biology and TechnologyFrom EverandFood Carotenoids: Chemistry, Biology and TechnologyNo ratings yet
- PerhitunganDocument1 pagePerhitunganRomah Cliquers LelledNo ratings yet
- Design, Evaluation and Study of Effect of Hydrophilic Polymers On Release Rate of Antiulcer Floating TabletsDocument7 pagesDesign, Evaluation and Study of Effect of Hydrophilic Polymers On Release Rate of Antiulcer Floating TabletsRomah Cliquers LelledNo ratings yet
- Floating Tablets of FamotidineDocument8 pagesFloating Tablets of FamotidineRomah Cliquers LelledNo ratings yet
- Msds PDFDocument5 pagesMsds PDFRomah Cliquers LelledNo ratings yet
- Gastric Juice RegulationDocument22 pagesGastric Juice Regulationjanuian75% (4)
- 05 05 NOTES-HormonalDocument3 pages05 05 NOTES-HormonalSidney TyNo ratings yet
- 1409-Article Text-3354-1-10-20231111Document6 pages1409-Article Text-3354-1-10-20231111Guna SoundariNo ratings yet
- Test Bank For Advanced Nutrition and Human Metabolism 7th Edition Gropper Smith Carr 1305627857 9781305627857Document22 pagesTest Bank For Advanced Nutrition and Human Metabolism 7th Edition Gropper Smith Carr 1305627857 9781305627857francisNo ratings yet
- Git Physiology Compiled by Umah, Umah VictorDocument43 pagesGit Physiology Compiled by Umah, Umah VictorNwaoha Chibuzor AnthonyNo ratings yet
- Nutritional TherapyDocument34 pagesNutritional TherapyArshi BatoolNo ratings yet
- Gastrointestinal PhysiologyDocument6 pagesGastrointestinal PhysiologyPedro RodriguezNo ratings yet
- Chapter 81, GI SecretionDocument88 pagesChapter 81, GI SecretionSangita MNo ratings yet
- Fisiologi Sekresi Asam LambungDocument6 pagesFisiologi Sekresi Asam Lambungaminullahginanjar_87No ratings yet
- 0.7 Surgery Trans PDFDocument29 pages0.7 Surgery Trans PDFJoy ManzanoNo ratings yet
- 1-Peptic UlcerDocument12 pages1-Peptic UlcerDAVID ULRICH DALLENo ratings yet
- GastritisDocument17 pagesGastritisSri Wahyuni HarliNo ratings yet
- Gastrointestinal Tract HormonesDocument10 pagesGastrointestinal Tract HormonesKevin SangNo ratings yet
- Gastrointestinal PhysiologyDocument134 pagesGastrointestinal Physiologyapi-19916399100% (1)
- Regulation of Gastric SecretionDocument18 pagesRegulation of Gastric SecretionSanchit Rao50% (2)
- Peptic UlcerDocument2 pagesPeptic Ulcermehnoor kaurNo ratings yet
- 1 IntroductionDocument22 pages1 IntroductionirfanNo ratings yet
- Git Lec 3,4Document14 pagesGit Lec 3,4Kim Sa-buNo ratings yet
- Physiology, Lecture 8, GIT 2 (Stomach) (Slides)Document24 pagesPhysiology, Lecture 8, GIT 2 (Stomach) (Slides)Ali Al-Qudsi100% (2)
- Gastro-Intestinal Hormones & TransmittersDocument23 pagesGastro-Intestinal Hormones & TransmittersAlbert ChuwaNo ratings yet
- Gastric SecretionDocument36 pagesGastric SecretionammuNo ratings yet
- The Gastric Phase of The Integrated Response To A MealDocument12 pagesThe Gastric Phase of The Integrated Response To A MealpuchioNo ratings yet
- In A Nutshell... : Biology 12 - The Digestive System - Chapter NotesDocument10 pagesIn A Nutshell... : Biology 12 - The Digestive System - Chapter NotesE ZeeNo ratings yet
- Gastric Secretions MineDocument27 pagesGastric Secretions MinesasamaterasuNo ratings yet
- Defining Physiology: Principles, Themes, Concepts.: Hwee Ming Cheng Kin Kheong Mah Kumar SeluakumaranDocument104 pagesDefining Physiology: Principles, Themes, Concepts.: Hwee Ming Cheng Kin Kheong Mah Kumar SeluakumaranGiovanni HenryNo ratings yet
- 303 - Gastrointestinal Physiology) Gastric Secretion - The Cephalic - Gastric PhaseDocument5 pages303 - Gastrointestinal Physiology) Gastric Secretion - The Cephalic - Gastric Phasekedas70No ratings yet
- Gastric Juice - 1Document31 pagesGastric Juice - 1wanderer_1010100% (1)
- Review Question - GI PDFDocument10 pagesReview Question - GI PDFTee BeeNo ratings yet