Jurnal 2
Jurnal 2
Uploaded by
Ade Yurga TonaraCopyright:
Available Formats
Jurnal 2
Jurnal 2
Uploaded by
Ade Yurga TonaraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Jurnal 2
Jurnal 2
Uploaded by
Ade Yurga TonaraCopyright:
Available Formats
Clinical Practice
HOR MONE Horm Res Paediatr Received: May 22, 2017
RESEARCH I N DOI: 10.1159/000479371 Accepted: July 10, 2017
Published online: November 13, 2017
PÆDIATRIC S
An International Consortium Update:
Pathophysiology, Diagnosis, and Treatment of
Polycystic Ovarian Syndrome in Adolescence
Lourdes Ibáñez a, b Sharon E. Oberfield c Selma F. Witchel d Richard J. Auchus e R. Jeffrey Chang f
Ethel Codner g Preeti Dabadghao h Feyza Darendeliler i Nancy Samir Elbarbary j
Alessandra Gambineri k Cecilia Garcia Rudaz l Kathleen M. Hoeger m Abel López-Bermejo n
Ken Ong o Alexia S. Peña p Thomas Reinehr q Nicola Santoro r Manuel Tena-Sempere s
Rachel Tao t Bulent O. Yildiz u Haya Alkhayyat v Asma Deeb w Dipesalema Joel x
Reiko Horikawa y Francis de Zegher z Peter A. Lee A
a Endocrinology,
Hospital Sant Joan de Deu, Esplugues, Barcelona, Spain; and bCIBERDEM, ISCIII, Madrid, Spain; c Division of
Pediatric Endocrinology, CUMC, New York-Presbyterian Morgan Stanley Children’s Hospital, New York, NY, USA;
d Division of Pediatric Endocrinology, Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA, USA; eUniversity of
Michigan, MSRBII, Ann Arbor, MI, USA; f Department of Reproductive Medicine, UCSD School of Medicine, La Jolla, CA,
USA; g Institute of Maternal and Child Research, University of Chile, School of Medicine, Santiago, Chile; h Department of
Endocrinology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India; i Istanbul Tıp Fakültesi, Çocuk
Kliniği, Istanbul, Turkey; j Ain Shams University, Cairo, Faculty of Medicine, Cairo, Egypt; k Department of Medical and
Surgical Sciences, University of Bologna, Bologna, Italy; l Division of Women, Youth and Children, Australian National
University, Canberra, ACT, Australia; m Department of OBGYN, University of Rochester Medical Center, Rochester, NY,
USA; n Pediatric Endocrinology, Hospital de Girona Dr. Josep Trueta, Girona, Spain; o MRC Epidemiology Unit, University
of Cambridge, Institute of Metabolic Science, Cambridge Biomedical Campus, Cambridge, UK; p Women’s and Children’s
Hospital, North Adelaide, SA, Australia; q University of Witten/Herdecke, Vestische Kinder- und Jugendklinik, Pediatric
Endocrinology, Diabetes, and Nutrition Medicine, Datteln, Germany; r Pediatrics, Yale School of Medicine, New Haven, CT,
USA; s University of Córdoba, Edificio IMIBIC, Córdoba, Spain; t Division of Pediatric Endocrinology, CUMC,
New York-Presbyterian Morgan Stanley Children’s Hospital, New York, NY, USA; u Department of Internal Medicine,
Division of Endocrinology and Metabolism, Hacettepe University School of Medicine, Ankara, Turkey; v Medical University
of Bahrain, BDF Hospital, Riffa, Kingdom of Bahrain; w Mafraq Hospital, Abu Dhabi, UAE; x Department of Paediatrics and
Adolescent Health, University of Botswana Teaching Hospital, Gaborone, Botswana; y Endocrinology and Metabolism,
National Center for Child Health and Development, Tokyo, Japan; z Department Pediatrics, University Hospital
Gasthuisberg, Leuven, Belgium; A Department of Pediatrics, Penn State College of Medicine, Hershey, PA, USA
Keywords Abstract
Polycystic ovary syndrome · Polycystic ovarian morphology · This paper represents an international collaboration of pae-
Hyperinsulinism · Hirsutism · Menstrual irregularities · diatric endocrine and other societies (listed in the Appendix)
Obesity · Insulin sensitizers · Anti-androgen under the International Consortium of Paediatric Endocrinol-
ogy (ICPE) aiming to improve worldwide care of adolescent
girls with polycystic ovary syndrome (PCOS)1. The manu-
L.I., S.E.O., and S.F.W. contributed equally and should be considered script examines pathophysiology and guidelines for the di-
to be first authors. agnosis and management of PCOS during adolescence. The
© 2017 S. Karger AG, Basel Peter A. Lee, MD, PhD
Department of Pediatrics, Penn State College of Medicine
500 University Drive
E-Mail karger@karger.com
Hershey, PA 17033 (USA)
www.karger.com/hrp E-Mail plee @ psu.edu
complex pathophysiology of PCOS involves the interaction
of genetic and epigenetic changes, primary ovarian abnor- 1,200
malities, neuroendocrine alterations, and endocrine and 1,100
metabolic modifiers such as anti-Müllerian hormone, hyper- 1,000
900
Number of citations
insulinemia, insulin resistance, adiposity, and adiponectin
levels. Appropriate diagnosis of adolescent PCOS should in- 800
clude adequate and careful evaluation of symptoms, such as 700
600
hirsutism, severe acne, and menstrual irregularities 2 years
500
beyond menarche, and elevated androgen levels. Polycystic
400
ovarian morphology on ultrasound without hyperandrogen-
300
ism or menstrual irregularities should not be used to diag- 200
nose adolescent PCOS. Hyperinsulinemia, insulin resistance, 100
and obesity may be present in adolescents with PCOS, but
1998
1999
2000
2001
2002
2003
2004
2005
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
2017
are not considered to be diagnostic criteria. Treatment of ad- a
olescent PCOS should include lifestyle intervention, local
therapies, and medications. Insulin sensitizers like metformin
60
and oral contraceptive pills provide short-term benefits on
55
PCOS symptoms. There are limited data on anti-androgens
50
and combined therapies showing additive/synergistic ac-
Number of publications
45
tions for adolescents. Reproductive aspects and transition
40
should be taken into account when managing adolescents.
35
© 2017 S. Karger AG, Basel
30
25
20
Introduction
15
10
Polycystic ovary syndrome (PCOS) is a long-term rec- 5
ognized, complex heterogeneous familial disorder [1, 2].
1997
1998
1999
2000
2001
2002
2003
2004
2005
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
Yet, despite decades of research, the etiology of PCOS re- b
mains elusive [3]. This collaborative effort, initiated by
Pediatric Endocrine Societies, was undertaken because of
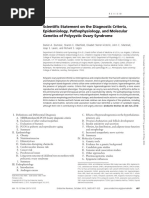
Fig. 1. a Annual number of citations for “adolescent PCOS” over
persistent questions in three areas: pathophysiology, di- the past 2 decades. b Annual number of publications for “adoles-
agnosis, and treatment1. This is attested to increased fo- cent PCOS” over the past 2 decades. Web of Science, Thomson
cus and number of publications related to PCOS, both in Reuters, 2017.
general and in the adolescent female (Fig. 1a, b).
The clinical symptoms, including hyperandrogenism
and chronic anovulation, typically develop during ado-
lescence. Further, the early onset of adrenarche may rep- Since this is a review of published manuscripts and ex-
resent the initial clinical feature of PCOS for some girls isting diagnostic and clinical practices and meets ethical
[4]. By the time patients present for medical attention, guidelines, it is exempt from Human Rights Review Com-
this multisystem disorder often has become a self-perpet- mittees and none have indicated any conflict of interest.
uating derangement in which identification of initiating
factors are difficult. Recent insights from genetic epide-
miology support long-standing clinical investigations in- A. Pathophysiology
dicating a broad etiopathology of PCOS.
Androgen excess, observed in approximately 60–80%
of patients with PCOS, is a key feature of the disorder.
1 Note that each of the societies designated one or more experts regarding
Hirsutism and hyperandrogenism are manifestations of
aspects of PCOS to participate in this endeavor. This is intended to be an up-
date of the current status of knowledge for the perspective that etiologic fac- the excessive androgen production. Indeed, hyperan-
tors, diagnostic criteria and treatment guidelines continue to be elucidated. drogenism, commonly demonstrated by elevated free
2 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
Fig. 2. Potential factors involved in pathophysiology of PCOS. Al- such as food choice, exercise, and endocrine disruptors influence
terations in steroidogenesis, ovarian folliculogenesis, neuroendo- the development of clinical features. Genome-wide association
crine function, metabolism, insulin secretion, insulin sensitivity, studies have identified loci of interest in close proximity to genes
adipose cell function, inflammatory factors, and sympathetic involved in gonadotropin secretion, gonadotropin action, ovarian
nerve function contribute to the pathogenesis of this disorder. Not follicular development, and insulin sensitivity.
all factors play roles in individual patients. Environment factors
(unbound) testosterone in circulation, is the most com- centrations contributing to higher free testosterone con-
mon abnormality observed in the syndrome and plays a centrations [5]. Herein, we deconstruct this complex
major role in perpetuating the aberrant hormone con- disorder into its major pathophysiologic components.
tributors to the pathophysiology of PCOS. Excessive Although we discuss specific elements, PCOS represents
ovarian androgen production is present in the majority of an example of systems biology with multiple intercon-
cases, but excessive adrenal androgen production can oc- nected signaling networks, which in individual instances
cur among some. The elevated androgen concentrations may not involve all networks (Fig. 2).
suppress sex hormone-binding globulin (SHBG) con-
Update: PCOS Pathophysiology, Horm Res Paediatr 3
Diagnosis, and Treatment DOI: 10.1159/000479371
1.1 Primary Ovarian Pathophysiology dehydroepiandrosterone (DHEA), DHEA sulfate, and
In humans, the factors influencing follicular growth androstenedione. It is becoming apparent that the ste-
are coordinated such that typically there is only a single roidogenic repertoire of the adrenal and, perhaps, the
follicle selected for terminal maturation and ovulation in theca cell include 11-hydroxyandrostenedione, which is
a sequential fashion. The maximum number of ovarian ultimately converted to the potent androgen 11-ketotes-
follicles, approximately 6–7 million, exist during mid- tosterone [14]. Women with PCOS showed higher serum
gestation and decrease to roughly 2–3 million primordial concentrations of the 11-oxygenated androgens 11β-hy-
follicles at birth. Subsequently, primordial follicles are droxyandrostenedione, 11-ketoandrostenedione, 11β-hy-
continuously recruited from this pool, with mechanisms droxytestosterone, and 11-ketotestosterone concentra-
to control the rate of entry of primordial follicles into the tions than control women [15].
growing pool being essential to maintain the ovarian re-
serve to preserve fertility [6]. These poorly understood 2. Insulin Resistance/Hyperinsulinemia
initial phases of follicular growth are gonadotropin-inde- Insulin resistance (IR) and hyperinsulinemia are com-
pendent and influenced by autocrine, paracrine, and local mon findings in women with PCOS independent of their
endocrine factors. degree of adiposity, body fat topography, and androgen
There is a dynamic balance between growing and dor- levels [16]. Women with PCOS have a high risk of devel-
mant follicles. In PCOS, the balance between androgens, oping impaired glucose tolerance and type 2 diabetes
anti-Müllerian hormone (AMH), and FSH is disrupted mellitus [17, 18] The pathogenesis of IR in PCOS reflects
leading to follicular arrest [7]. Abundant LH drives the the interaction of genetic influences, non-heritable intra-
theca cells to produce androgens, but FSH concentrations and extrauterine environmental factors, and alternative
and conversion of androgens to estradiol are insufficient, adaptations to energy excess. However in the context of
resulting in failure to select a dominant follicle, thus PCOS, puberty per se might play an important role in the
chronic anovulation [8]. AMH, secreted by granulosa molecular origins of IR and hyperinsulinemia. During
cells, plays a major role in governing this balance because puberty, adolescents experience a temporary decline in
it inhibits transition from primordial to primary follicles. insulin sensitivity with a nadir in mid-puberty [19–21].
Hence, PCOS is characterized by increased growth of This was first described in an effort to understand the de-
small follicles but subsequent growth arrest leading to the terioration of glycemic control in type 1 diabetes during
typical polycystic morphology. It has been suggested that adolescence [20]. This transient IR and hyperinsulinemia
the follicles in a PCOS ovary inherently differ from folli- have been attributed to the increases in growth hormone
cles in a normal ovary [9]. and IGF-1 concentrations in this period of growth to pro-
Theca cells obtained from women with PCOS retain vide more amino acids [20]. Pubertal IR appears to be
their phenotype with increased androgen secretion from selective for glucose metabolism, whereas protein metab-
increased CYP17A1 expression or P450c17 activity [10]. olism seems to respond normally to insulin action [22].
Immunohistochemical studies have indicated that pro- Importantly, IR in PCOS women is tissue-selective.
teins involved in the alternate “backdoor pathway” of ste- Resistance to the metabolic actions of insulin has been
roidogenesis are more highly expressed in PCOS theca reported primarily in skeletal muscle, adipose tissue, and
cells [11]. Genome-wide association studies (GWAS) di- liver; while sensitivity to insulin actions on steroidogen-
rected investigation to a specific locus, DENND1A, alter- esis persists in the adrenal gland and ovary. Hence the
native splicing of the DENND1A transcript generates sev- paradox: whereas some tissues manifest IR in women
eral variants. Expression of one variant, DENND1A.V2, with PCOS, steroid-producing tissues remain insulin
is greater in PCOS theca cells. Curiously, knockdown of sensitive [23].
this variant recapitulates a normal theca cell phenotype in While early studies attributed the IR in PCOS to obe-
PCOS ovaries, whereas overexpression in theca cells from sity, subsequent studies including euglycemic-hyperinsu-
normal women recapitulates PCOS phenotype [12]. The linemic clamp studies demonstrated the existence of IR
mechanism governing the regulation of the alternative in lean PCOS women [16, 24]. However, Stepto et al. [24]
splicing appears to reside outside of the DENND1A gene included patients diagnosed using the Rotterdam criteria
[13]. in their study (2 of the 3 criteria: oligo/anovulation, hy-
Many steroidogenic enzymes are expressed in both the perandrogenism, and polycystic ovaries on ultrasound
adrenal cortex, especially the zona reticularis, and the the- were used). Nevertheless, another large study found that
ca cell. Hormones secreted by the zona reticularis include only 53 out of 201 (26.3%) lean PCOS women (body mass
4 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
index [BMI] less than 25) had IR, suggesting that ethnic topic fat accumulation can also occur in the absence of
background and dietary composition might play a role in obesity, i.e., when there has been reduced prenatal growth
the metabolic factors among these women [25]. and thus a reduction in subcutaneous fat storage capacity
Both in vivo and in vitro studies suggest that insulin as that is followed by rapid postnatal catch-up and a relative
well as IGF-1 can synergize with LH to increase theca cell excess of fat, which is stored in the same ectopic depots
androgen production [26]. Insulin can also decrease the [45].
hepatic synthesis of SHBG increasing circulating free an- Molecular mechanisms responsible for IR in PCOS
drogens [27]. Additionally, insulin may directly stimulate include defective post-receptor insulin activity, in-
the activity of ovarian P450c17 and P450scc enzymes to creased free fatty acids, increased cytokine secretion,
promote ovarian androgen steroidogenesis [28]. In addi- and increased androgens [46–50]. Intra-abdominal adi-
tion, pancreatic beta cell secretory dysfunction has been pocytes show increased release of free fatty acids and
described in a subset of women with PCOS; this subset increased cytokine secretion, e.g., TNF-α, IL-6, leptin,
probably has the highest risk of developing carbohydrate and resistin [51, 52]. The increased free fatty acids drain
intolerance and type 2 diabetes [29]. via the portal vein to the liver and subsequently affect
Other potential mechanisms, including pubertal in- the secretion, metabolism, and peripheral actions of in-
crease in androgen production are hypothesized to con- sulin. Hence, the distribution of fat, rather than the mere
tribute to IR and hyperinsulinemia. The association be- presence of obesity or increased BMI, may be highly rel-
tween IR and androgen excess in women has long been evant in PCOS [53, 54]. Some studies have also suggest-
recognized because of the association of hyperandrogen- ed that IR in subjects with PCOS might be driven by
ic features with the rare syndromes of extreme IR due to alternative mechanisms differing from those occurring
mutations of the insulin receptor or autoantibodies tar- in obesity. In fact, women with PCOS are reported to
geting the insulin receptor [30–32]. Insulin may also po- have a higher degree of serine phosphorylation of the
tentiate the steroidogenic response to gonadotropins in- insulin receptor and insulin receptor substrate-1 result-
directly, by acting at the pituitary to increase gonadotrope ing in impaired insulin signal transduction and intrinsic
sensitivity to GnRH [33]. Furthermore, increased andro- IR independent of total or fat-free body mass [55]. In
gen levels have been associated with decreased adiponec- addition, a proinflammatory milieu amplified by PCOS
tin secretion by adipocytes in PCOS women, thereby fur- and obesity has been described in ovarian granulosa
ther reducing insulin sensitivity and consequently in- cells and stroma [56, 57].
creasing compensatory insulin levels [34]. In addition, Accumulation of lipids, i.e., diacylglycerol (DAG) and
insulin may also drive adipose androgen generation by ceramides, in muscle and liver interferes with insulin sig-
increasing aldo-keto reductase 1C3 (AKR1C3) activity in naling [58]. Intra-cellular ceramides can also impair in-
female subcutaneous adipose tissue [35]. sulin signaling by blocking the translocation of Akt, an
Obesity alone is associated with IR and compensatory important mediator of insulin sensitivity, to the plasma
hyperinsulinemia. Although the prevalence rates of obe- membrane [59, 60]. Interestingly, animal data have shown
sity vary widely across different geographic regions and that disrupted insulin signaling in the central nervous
ethnicities, a large proportion of PCOS patients are over- system is associated with the development of obesity and
weight or obese [36, 37]. Among obese adolescents, obe- impaired ovarian follicular maturation [61], suggesting
sity-associated IR may exacerbate the IR associated with another link between IR, hyperinsulinemia, obesity, and
puberty during this period of life, predisposing this group PCOS.
of individuals to develop prediabetes and type 2 diabetes
[38]. 3. Neuroendocrine Alterations
Several studies have reported associations for visceral 3.1. Changes in GnRH and Gonadotropin Secretion
obesity, proinflammatory markers, elevated fasting and in PCOS
glucose-stimulated insulin levels, and greater IR among Although not mandatory for diagnosis, a hallmark of
women with PCOS [39–42]. Endothelial dysfunction has PCOS is the presence of deregulated secretion of the go-
been described and may promote chronic inflammation nadotropins, LH and FSH, which control ovarian ste-
[43]. Although the mechanisms responsible for obesity- roidogenesis, follicular dynamics, and ovulation [3, 62–
related IR are not completely clear, ectopic accumulation 64]. Hence, it is reasonable to hypothesize that altered
of fatty acids in organs and tissue that are not meant to gonadotropin secretory profiles could impact the cardi-
store large amounts of fat appears to play a role [44]. Ec- nal features of PCOS, including hyperandrogenism and
Update: PCOS Pathophysiology, Horm Res Paediatr 5
Diagnosis, and Treatment DOI: 10.1159/000479371
ovulatory dysfunction [3, 4]. In fact, increased circulating estrogen receptor-β (ERβ), whose role in feedback con-
LH levels, increased LH:FSH ratios, elevated LH pulse trol of GnRH neurons remains unclear, is present. Ac-
frequency and/or amplitude, as well as relatively de- cordingly, it is tenable that the primary impact of andro-
creased FSH levels have been typically described in wom- gen excess on the feedback regulatory loops during differ-
en with PCOS [3, 65]. Yet, a fraction of PCOS patients ent developmental windows occurs at neuronal sites
with hyperandrogenism, especially when associated with other than (and likely upstream of) GnRH cells.
obesity, display non-elevated basal or stimulated LH lev-
els, which further attests the heterogeneity of presenta- 3.2. Altered Kisspeptin Signaling in PCOS
tions (and pathophysiology) of the syndrome. Although Among the various afferent neurons to GnRH neu-
LH is considered to be the biomarker of GnRH pulses, rons, Kiss1 neurons, which produce kisspeptins (encoded
dissociation between GnRH and LH has been reported in by the KISS1 gene), have emerged in the last decade as
several models which may contribute to the lower LH se- master regulators of GnRH neurosecretion and ovula-
cretion in some obese women with PCOS [66]. tion. Kisspeptins are among the most potent activators of
The alterations in gonadotropin secretory profiles are GnRH neurons identified to date [70]. Various KISS1/
compatible with changes in the profiles of GnRH pulsatil- Kiss1 neuronal populations have been identified in differ-
ity, presumably reflecting an increase in the activity of the ent mammalian species, including humans, rodents, and
GnRH pulse generator. Indeed, classical neuroendocrine non-human primates. A prominent and highly conserved
studies established that a pattern of GnRH secretion de- population of KISS1 neurons has been reported at the ar-
fined by increased number of pulses favors LH over FSH cuate nucleus (ARC) of the mediobasal hypothalamus, or
secretion by the pituitary [67]. While it is possible that its equivalent infundibular region in humans [71]. In ro-
primary (e.g., genetically determined) alterations at the dents, this ARC Kiss1 neuronal population has been pro-
GnRH pulse generator network might drive such changes posed to operate as a major hub for mediating the nega-
in some patients, data from different clinical and experi- tive feedback effects of sex steroids, as sex steroids consis-
mental studies have pointed out contributing roles of per- tently suppress Kiss1 expression at this site. In contrast, a
turbations of key modulators of GnRH neurosecretion, second more rostral hypothalamic population of Kiss1
including insulin and androgens, whose levels are report- neurons may participate in positive feedback, as estrogen
edly altered in PCOS [68]. enhances Kiss1 expression at this site [70].
Considering that hyperandrogenism is a hallmark of One interesting feature of the population of Kiss1 neu-
PCOS, considerable attention has been devoted to the in- rons in the ARC is that at least a fraction of them co-ex-
vestigation of potential mechanisms through which de- press other neurotransmitters that also play major roles
regulated androgen secretion contributes to the neuroen- in the control of GnRH/gonadotropin secretion [72].
docrine alterations of the syndrome [3]. Indeed, compel- These other neurotransmitters include neurokinin B
ling evidence suggests that elevated androgens disrupt the (NKB) and dynorphin. The NKB receptor NK3R is also
capacity of sex steroids to regulate GnRH/LH secretion expressed in Kiss1 neurons. This population of neurons
via classical feedback loops. This would result in dimin- which co-express kisspeptins, NKB, and dynorphin has
ished negative feedback actions of ovarian steroids (estro- been called KNDy neurons [73]. Based on the reported
gens and progesterone) that would contribute to and per- actions of NKB and dynorphin, which predominantly
petuate the LH hypersecretion characteristic of PCOS stimulate and inhibit LH secretion, respectively, and the
[67]. In fact, clinical data point out that diminished pro- dense interconnection of KNDy neurons within the ARC,
gesterone- and estrogen-negative feedback, linked to an- it has been proposed that NKB and dynorphin participate
drogen excess, has a role in the reported elevation of LH in a Ying-Yang fashion in the (auto)regulation of kiss-
pulsatility in patients with PCOS [69]. Furthermore, re- peptin output to GnRH neurons, and hence in the gen-
duced sensitivity to progesterone-negative feedback, due eration of GnRH pulses. As KNDy neurons are sensitive
to early-onset hyperandrogenism, has been mechanisti- to sex steroids and modulate GnRH pulse generation, it
cally linked to elevated LH secretion in women with is reasonable to speculate that deregulated function of this
PCOS, although only half of the patients seem to display neuronal population might contribute to the neuroendo-
overtly impaired negative feedback of progesterone [69]. crine alterations of PCOS.
From a mechanistic standpoint, it is notable that GnRH However, limited experimental evidence is available to
neurons appear to be devoid of the major sex steroid re- support or refute this possibility. Despite the meager data
ceptors responsible for negative feedback [70], while the for human and non-human primates, review of preclini-
6 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
cal rodent models can provide insights into the neuroen- al alteration of gamma-aminobutyric acid (GABA) sig-
docrinology of PCOS. To date, some studies have report- naling following early androgenization in a mouse model
ed alterations in Kiss1 expression and/or the number of of PCOS, which might explain part of the neuroendocrine
Kiss1 neurons in the hypothalamus of various preclinical alterations of the syndrome [81].
animal models of PCOS, generated by excessive androgen While GABA is generally regarded as inhibitory trans-
exposure at different developmental windows. Studies in mitter, different studies have documented that under cer-
rodent models of PCOS due to postnatal exposure to an- tain conditions, acting via GABA-A receptors, GABA can
drogens have reported persistent suppression of hypotha- evoke depolarization (activation) responses directly in
lamic Kiss1 expression [74]; a finding that is consistent GnRH neurons [82]. Moreover, a GABA neuronal path-
with the proven inhibitory action of sex steroids on Kiss1 way originating from the ARC is likely to play a role in
expression in the ARC and compatible with similar ob- transmitting the feedback actions of sex steroids. In this
servations in models of neonatal estrogenization of fe- context, studies in a mouse PCOS model of prenatal ex-
male rats [75]. However, different models of androgen- posure to dihydrotestosterone (DHT) has documented
ization have been reported to cause variable deregulation an increase in the GABAergic drive to GnRH neurons, as
of Kiss1/kisspeptin expression in the hypothalamus. evidenced by functional (increased postsynaptic cur-
Thus, it is likely that the actual change (up- or downregu- rents) and morphological (increased number of apposi-
lation) of the Kiss1 system depends on the developmental tions of GABA fibers) data. This state of enhanced GABA
window and regimen of exposure to androgens. input would derive from suppressed progesterone recep-
Although supportive evidence is sparse, the other tor expression in ARC GABA neurons projecting to
KNDy neuropeptides might also be involved in the patho- GnRH neurons, thus resulting in diminished restraint of
physiology of neuroendocrine alterations of PCOS [70, GABA signaling to GnRH neurons with consequent ele-
72]. NKB has been suggested to operate as stimulatory vated GnRH neurosecretion. In addition, androgenic me-
drive for kisspeptin neurosecretion onto GnRH neurons. tabolites generated following inappropriate exposures to
Hence, alterations of central NKB levels might impact DHT, such as 3α- and 3β-androstanediols, may also con-
GnRH and LH secretory profiles. This corresponds with tribute to activation of GABA-A receptors and suppres-
recent evidence showing that oral administration of the sion of the negative feedback machinery in GnRH neu-
antagonist of NKB receptor, ESN364, to intact female rons [81]. Admittedly, the experimental data supporting
monkeys lowered LH concentrations and blocked the LH such a pathogenic GABA pathway derive from a single
surge [76]. Another NK3R antagonist (AZD4901) was mouse PCOS model, which does not mimic the obese
administered to 67 women with PCOS for 28 days; treat- phenotype that is commonly seen in at least half of PCOS
ment with the highest dose was associated with decreased patients. Hence, it remains unclear whether GABAergic
LH pulse frequency and decreased testosterone concen- deregulation is commonplace in the wide spectrum of
trations [77]. Interestingly, pharmacological studies in clinical cases of PCOS.
humans have also shown that while administration of
NKB alone did not alter circulating gonadotropin levels, 3.4. Other Endocrine and Metabolic Modifiers
NKB partially suppressed gonadotropin responses to of GnRH Secretion in PCOS: AMH, Insulin, and
kisspeptin [78]. Thus, multidimensional interactions Adiponectin
likely modulate the actions of the KNDy peptides in the Recent data has revealed a previously unknown role of
control of gonadotropin secretion. This complexity has AMH in the stimulatory control of GnRH neurons [83].
also been documented in equivalent preclinical studies Central injection of AMH has been shown to increase the
[79, 80]. Whether such interactions are appreciably per- pulsatile secretion of LH in female mice in a dose-depen-
turbed in PCOS remains to be clarified. dent manner. This GnRH-dependent effect was associ-
ated to an increase in the firing of GnRH neurons, which
3.3. Altered GABA Signaling and PCOS express the AMH receptor AMHR2 [83]. In this context,
In addition to perturbed kisspeptin/KNDy signaling, it has been proposed that deregulated AMH levels in
evidence for deregulation of other key central neuroen- PCOS might contribute to the state of LH hypersecretion.
docrine pathways governing GnRH neuron function has However, it is important to note that the stimulatory ac-
been presented in preclinical models of PCOS. Among tions of AMH on GnRH neurosecretion have been ob-
those, elegant studies conducted by Campbell and co- served in control mice, not in PCOS models or patients;
workers have convincingly demonstrated a multi-factori- hence, although very appealing, the potential central role
Update: PCOS Pathophysiology, Horm Res Paediatr 7
Diagnosis, and Treatment DOI: 10.1159/000479371
of AMH in the neuroendocrine dysfunction associated ipose tissue (BAT) in this model, which caused an increase
with PCOS remains to be verified. in circulating adiponectin, equally corrected the metabol-
Although hyperandrogenism and possibly other ovar- ic and ovarian abnormalities of this preclinical model of
ian factors are major factors contributing to the increased PCOS [91]. It must be stressed, however, that the thera-
GnRH/LH secretion, the elevated insulin levels and IR are peutic benefits of adiponectin administration and/or
also putatively involved in such neuroendocrine altera- BAT transplantation in women with PCOS are yet to be
tions. In fact, central insulin actions are indispensable for demonstrated.
proper functioning of the gonadotropic axis in mice; lack
of brain insulin signaling decreases LH levels and disturbs 4. Genetics
follicular maturation [60]. In good agreement, insulin in- Studies of monozygotic and dizygotic twins have indi-
fusion in control women increased LH pulse frequency, cated a moderate heritability of PCOS. Other epidemio-
reminiscent of secretory profiles of women with PCOS logical studies have indicated the likely importance of
[84]. In fact, lean patients with PCOS have been shown to considering risk factors and biological processes acting
display increased basal LH levels and LH:FSH ratios. Yet, throughout the life-course: low birth weight and fetal ex-
another study involving women with PCOS reported that posure to androgens; postnatal rapid weight gain; preco-
insulin administration failed to alter LH pulsatility [85]. cious adrenarche and early age at pubertal development;
The mechanisms responsible for the effects of high in- adult weight status and lifestyle.
sulin levels on the GnRH pulse generator need further Until recently, candidate gene studies have been un-
elucidation. Insulin receptors in GnRH neurons appear derpowered leading to poorly reproducible results. The
dispensable for proper pubertal maturation and fertility, advent of large-scale GWAS with their stringent statisti-
therefore pointing to a primary action of insulin at other cal thresholds has brought robust new insights, although
brain targets, likely occurring upstream of the GnRH as yet these have been limited to adult PCOS cases and
neurons [86]. Studies in sheep and rodents suggest that their direct relevance to adolescent PCOS is yet to be es-
insulin signaling may modulate Kiss1 neuron function, tablished. The first GWAS for PCOS were performed in
thereby regulating GnRH neurosecretion [87, 88]. In fact, Han Chinese populations [92, 93]; while the identified
analyses in a sheep model of PCOS generated by gesta- genomic loci were replicable in that population, their ef-
tional androgenization revealed a decrease in IR expres- fects estimates are consistently smaller in Caucasian
sion in ARC KNDy neurons [87]. However, the function- PCOS cases, possibly due to population differences in
al relevance of such direct actions of insulin in Kiss1 neu- genetic architecture or even PCOS sub-phenotypes [94,
rons, in terms of control of gonadotropin secretion and 95].
fertility appear to be modest, if any, according to rodent Several of the individual genomic signals for PCOS
studies [89]. This would suggest that insulin operates at have provided new insights into its pathophysiology. As
other elements of the GnRH pulse generator to modulate noted above, the role of DENND1A splice transcripts in
GnRH secretion. Alternatively, related factors, such a ovarian theca cell steroidogenesis is being investigated.
IGF-I, known to act directly at GnRH neurons to control The PCOS susceptibility allele in the FSHB gene is also
the reproductive axis might contribute to deregulated go- associated robustly with lower circulating FSH levels [94,
nadotropin secretory profiles in women with PCOS. 95], and with other phenotypes indicative of diminished
Another metabolic regulator with putative pathophys- ovarian follicle stimulation: later onset of puberty, and
iological roles in PCOS is adiponectin, an adipokine neg- lower risk for dizygotic twinning [96]. Together, these
atively correlated with IR and adiposity. Although con- genetic findings indicate a co-primary neuroendocrine
flicting results have been reported on changes in circulat- pathogenesis of PCOS, alongside its likely ovarian etiol-
ing adiponectin in women with PCOS, systematic analyses ogy. These genetic studies and the pharmacologic studies
of published data suggest that women with PCOS display involving NK3R antagonists encourage further investiga-
lower adiponectin levels, which correlate with IR [90]. tion into the neuroendocrine features of PCOS. GWAS
While the pathogenic relevance of such alterations re- findings also suggest the importance of future studies of
mains to be established in humans, an experimental rat the possible role of epidermal growth factor receptors on
model of PCOS associated with DHEA administration re- ovarian follicle development/steroidogenesis [94].
vealed that adiponectin administration was largely suffi- Another powerful use of the genomic data is to test
cient to reverse the PCOS-like phenotypes of DHEA- combinations of signals that indicate the potential causal
treated rats [91]. Moreover, transplantation of brown ad- influences of biological pathways. Such Mendelian ran-
8 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
domization analyses have indicated causal roles in PCOS sion in pathways such as the type 1 diabetes mellitus path-
etiology for higher BMI, higher IR, and lower serum way, p53 signaling pathway and NOD-like receptor
SHBG concentrations, which could act by increasing the signaling pathway (involved in immune responses), as
bioactivity of androgens or other sex steroids [94]. Final- well as in metabolic pathways involved in ovarian func-
ly, a highly robust yet unexplained association between tion (IGFBP2, INSR, SLC2A8, NRIP1) and in ovarian ste-
genetic variants that confer a later age at menopause and roidogenesis (CYP19A1, AMH and its receptor AMHR2)
higher susceptibility to PCOS is intriguing [94]. It sug- [104, 105].
gests that perhaps the evolutionary incongruity of this In peripheral blood cells, differential methylation was
common heritable disorder impacting fertility might be observed in pathways related to the immune response
explained by its co-susceptibility to preserved fecundity and to cancer pathways (cellular survival, proliferation,
at older age. pluripotency, invasion, metastasis, and angiogenesis)
[106]. Interestingly, the association with immune path-
5. Epigenetics ways was also described in another report relating PCOS
A number of GWAS as well as replication studies in with epigenetic changes in pathways involved in autoim-
Chinese and Caucasian subjects have identified the LH/ mune and allergic diseases, such as type 1 diabetes mel-
choriogonadotropin receptor (LHCGR) (locus 2p16.3) as litus, thyroid disease, and asthma [107], and was consis-
a susceptibility gene for PCOS [97]. Increased LH activity tent with the abovementioned results in ovarian tissue
is a common feature in PCOS and may contribute to the [104].
defective folliculogenesis and hyperandrogenism com- In addition to the ovary and peripheral blood cells, ge-
monly seen in these patients. Hypomethylation of the nome-wide methylation studies have been performed in
LHCGR was first described in a mouse model of PCOS adipose tissue from women with PCOS and in a primate
and has been recently confirmed in human peripheral model of PCOS. In women, differential methylation
blood cells and granulosa cells from PCOS subjects [98, was observed in genes involved in steroid metabolism
99]. Decreased LHCGR methylation is known to increase (CYP1B1), liver function (GPT), in a candidate gene for
gene expression [100]. Hypomethylation of LHCGR, by PCOS (RAB5B, which participates in intracellular vesicle
causing hypersensitivity to LH pulses, may thus be a plau- transport), in two genes related to type 2 diabetes mellitus
sible mechanism underlying susceptibility to PCOS. (PPARG, SVEP1) and in one gene involved in DNA meth-
Aromatase, encoded by CYP19A1, is another candi- ylation (DMAP1) [108]. In prenatally androgenized fe-
date gene in PCOS. As estrogens are required for follicle male rhesus monkeys, differential methylation in adipose
selection and growth, decreased aromatase may contrib- tissue was observed for two anti-proliferative gene signal-
ute to the defective folliculogenesis observed in PCOS pa- ing pathways: TOB (involved in T-cell signaling) and
tients. In Chinese women with PCOS, CYP19A1 was hy- transforming growth factor-β (TGFB) [109]. The avail-
permethylated in ovarian tissue, which correlated with able genome-wide methylation studies in women with
decreased mRNA and protein levels [101]. In another PCOS are summarized in a recent review by Li et al. [110].
study, EPHX1, which encodes for epoxide hydrolase 1, an The authors highlight the significant association of PCOS
enzyme necessary for the degradation of aromatic com- phenotype with immune responses both in ovaries and in
pounds, was hypomethylated in peripheral blood cells peripheral blood cells.
from women with PCOS. In human granulosa-like tumor Regulation of gene expression by microRNAs (mi-
cells, it was also demonstrated that EPHX1 regulated es- RNAs) is considered to be an additional layer of epige-
tradiol concentrations, indicating a role for EPHX1 hypo- netic regulation. A genome-wide circulating miRNA ex-
methylation in ovarian steroidogenesis [102]. Alterations pression profile identified a number of miRNAs dysregu-
in the methylation pattern and expression of peroxisome lated in women with PCOS. These miRNA species are
proliferator-activated receptor gamma 1 (PPARG1), involved in glycometabolism and ovarian follicle devel-
which is involved in the regulation of ovarian function, opment pathways [111, 112]. Interestingly, miRNA-592
and of its co-repressors has also been described in granu- has been shown to be downregulated and to be inversely
losa cells from women with PCOS and in animal models related to LHCGR levels in PCOS patients [113].
of PCOS [103].
Besides gene-targeted studies, genome-wide methyla- 6. Altered Sympathetic Nerve Activity
tion studies in ovaries of women with PCOS have re- An alteration in sympathetic nerve activity has been
vealed alterations in DNA methylation and gene expres- proposed to contribute to the etiology of PCOS. Indeed,
Update: PCOS Pathophysiology, Horm Res Paediatr 9
Diagnosis, and Treatment DOI: 10.1159/000479371
Table 1. Suggested criteria for the diagnosis of PCOS in adolescence
Required Optionala Not recommendedb Comments
1. Irregular menses/ 1. PCOM 1. Obesity 1. Must generally be 2 years
oligomenorrhea 2. Severe cystic acne 2. Insulin resistance post-menarche
2. Evidence of hyperandrogenism: 3. Hyperinsulinemia 2. Must rule out other disorders
a. Biochemical 4. Biomarkers (e.g., AMH, of hyperandrogenism (e.g.,
b. Clinical (e.g., progressive T/DHT ratio) NC-CAH, Cushing syndrome)
hirsutism) 5. Acanthosis nigricans
PCOS; polycystic ovary syndrome; PCOM, polycystic ovarian morphology; AMH, anti-Müllerian hormone; T/DHT, testosterone to
dihydrotestosterone; NC-CAH, non-classical congenital adrenal hyperplasia. a These criteria are often used in concert with the required
criteria, but should not be used independently as diagnostic features. b These criteria have been associated with PCOS but are not
diagnostic.
many of the common clinical symptoms of PCOS, includ- deed, it is possible that adolescent hyperandrogenemia is
ing central obesity, hyperinsulinemia, and hyperandro- a consequence of the lack of full maturation of the hypo-
genemia, are associated with chronic increased activity of thalamic-pituitary-ovarian axis during this time of life.
the sympathetic nervous system [114, 115]. Direct assess- Similarly, prolonged anovulatory cycles are simply typi-
ment of sympathetic activity in PCOS women revealed an cal of pubertal development rather than an early manifes-
association between high muscle sympathetic nerve ac- tation of PCOS. Most importantly, it remains unclear
tivity and PCOS independently of BMI [116]. Additional when persistence of adolescent oligomenorrhea becomes
indirect markers of autonomic activity including heart a significant clinical finding (Table 1).
rate variability and heart rate recovery after exercise have As noted above, IR and hyperinsulinemia are often
demonstrated that young PCOS women exhibit increased noted in women with PCOS and may influence the devel-
sympathetic and decreased parasympathetic responses to opment of PCOS in some patients. However, current def-
these challenges [117–119]. initions of PCOS do not include obesity, IR, or hyperin-
Increased ovarian sympathetic tone in PCOS is sup- sulinemia as diagnostic criteria [127–135]. Nevertheless,
ported by the finding of a greater density of catechol- we will discuss as to whether adolescents with these find-
aminergic nerve fibers in polycystic ovaries [120] and ad- ings should be considered as being at risk for PCOS, since
ditional studies in a rat PCOS model that demonstrated they may carry an additional risk for manifestation of
increased sympathetic outflow previous to the appear- metabolic disease in adult life.
ance of ovarian cysts [121]. Additional studies in this rat
model showed an association between the development 1. Clinical Features
of follicular cysts and chronic increased production of As in adults, signs of hyperandrogenism in adolescents
nerve growth factor in the ovary [122], a hallmark of sym- can be clinical or biochemical. Hirsutism is defined as ex-
pathetic hyperactivity. The association between the neu- cessive, coarse, terminal hairs distributed in a male fash-
rotrophins and PCOS was strengthened by the finding ion, and PCOS is the most common cause of hirsutism in
that ovarian nerve growth factor production is increased adolescence [136]. The severity of hirsutism may not cor-
in PCOS women [123]. relate with serum androgen levels; moreover, there are
ethnic/genetic differences that may affect the degree of
hirsutism [137–139]. Hirsutism must be distinguished
B. Diagnosis from hypertrichosis defined as excessive vellus hair dis-
tributed in a non-sexual pattern. Mild hirsutism may not
As previously reviewed [124], diagnostic criteria for be a sign of hyperandrogenemia [140], but the likelihood
PCOS in adolescence remain controversial, primarily be- of androgen excess is increased when associated with oth-
cause the diagnostic pathological features used in adult er findings such as menstrual irregularities [141, 142].
women may be normal pubertal physiological events. Moderate or severe hirsutism may be a sign of androgen
These features include irregular menses, cystic acne, and excess in early postmenarcheal years. In adults, the eval-
polycystic ovarian morphology (PCOM) [125, 126]. In- uation and grading of hirsutism can be done using the
10 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
Ferriman-Gallwey scoring system, which may not be suit- than 3 months), or primary amenorrhea in girls with com-
able for adolescents (modified Ferriman-Gallwey) [132]. pleted puberty may suggest androgen excess [158, 159].
Adult terminal hair distribution is usually achieved by 2 Ovulatory dysfunction may also present as dysfunctional
years after menarche. The original report of Ferriman and uterine bleeding (cycles shorter than 21 days or lasting
Gallwey included females starting from the age of 15 years more than 7 days) [160–162]. These menstrual distur-
[143]. Ethnic and racial variation in the extent of hair bances may all be reflective of androgen excess [154]. One
growth influences this semi-subjective cutaneous sign of should keep in mind that age at menarche may differ in
androgen excess [131]. girls with PCOS due to variable presentation, including
Although acne is a common problem in adolescence, early puberty and primary amenorrhea. Age at menarche
it is usually transient and may not be indicative of hyper- may be inversely correlated to obesity [163, 164].
androgenism [144, 145]. Moderate or severe inflamma- Confirmation of biochemical hyperandrogenism is
tory acne, especially if unresponsive to topical therapy, important in symptomatic adolescents before a defini-
however, may require investigation of androgen excess tive diagnosis of PCOS can be considered. As described
[124, 146]. In a 5-year longitudinal analysis, development in prior publications on PCOS in adolescents, measure-
of moderate to severe inflammatory acne has been report- ments of total and/or free testosterone have been the
ed to be associated with androgen excess [147]. Alopecia most recommended hormone determinations to docu-
is rare and not well studied in adolescents [148]. Isolated ment hyperandrogenemia [165]. Methodological prob-
acne and alopecia should not be considered to be diag- lems regarding testosterone determinations include the
nostic criteria of PCOS in adolescence. following: (1) inadequate assay sensitivity to measure
Premature adrenarche (PA), defined in girls as the ap- low testosterone concentrations in girls and women; (2)
pearance of pubic hair before 8 years of age with Tanner assay interference due to simultaneous presence of other
II–III levels of adrenal androgens, may herald PCOS in steroid molecules with similar structure; (3) lack of well-
childhood [149]. However, PA does not precede PCOS in defined normative values; (4) binding of testosterone to
all girls [148] and not all girls with PA will develop PCOS SHBG and other proteins in the peripheral circulation,
[4, 150]. Persistent hyperandrogenemia in girls with PA and (5) technical aspects of testosterone assays [166–
may lead to PCOS, especially if accompanied by obesity 168].
[151]. Continued prospective monitoring of girls with PA Most recommendations advocate utilization of high-
should be performed. The diagnosis of non-classic con- quality liquid chromatography/tandem mass spectrom-
genital adrenal hyperplasia should be excluded based on etry (LC-MS/MS) to measure testosterone. However, un-
history, examination, and hormone levels including til this technology is universally available, high-quality
ACTH stimulation tests if warranted [152]. Similarly, pa- RIA with extraction and chromotography should be em-
tients should be screened for Cushing syndrome, if clini- ployed. Available guidelines have suggested total testos-
cal features are suggestive. terone concentrations >55 ng/dL (1.91 nmol/L) are likely
Irregular menses should also not be used as the only consistent with hyperandrogenism. Further, Gambineri
criterion for PCOS in adolescence because menstrual ir- et al. [169] defined hyperandrogenism during the follicu-
regularities are typical for at least 2 years after menarche lar phase as total testosterone concentrations >42 ng/dL
[124]. In adolescence, irregular menses that persist 2 years (1.45 nmol/L) using a LC-MS/MS assay. Because of the
after menarche may be a sign of PCOS, although irregular variability in the results of testosterone assays and the
menses may continue up to the 5th year after menarche limited data on the normal development fluctuations in
without development of PCOS [153, 154]. About 85% of testosterone levels during adolescence, no clear cutoff tes-
cycles are anovulatory during the 1st year after menarche, tosterone concentrations can be given.
59% during the 3rd year, and 25% in the 6th year [154].
Moreover, irregular cycles may not necessarily be associ- 2. Polycystic Ovary on Ultrasound: PCOM
ated with clinical or biochemical hyperandrogenism The presence of enlarged ovaries with increased stro-
[155]. The Endocrine Society Guidelines required persis- ma and multiple small peripheral cysts is known as
tent oligomenorrhea (menstrual cycles longer than 45 PCOM. PCOM is associated with hyperandrogenism but
days) for the diagnosis of PCOS in adolescents [134]. is not always included as a diagnostic element of PCOS.
Based on the expected variation of menstrual cycles in PCOM is an inconsistent finding in healthy girls [170]
normal girls [156, 157], the persistence of oligomenor- and adults [171], but a higher persistence of PCOM over
rhea, secondary amenorrhea (absence of cycles for more time is observed in hyperandrogenic adolescents [172].
Update: PCOS Pathophysiology, Horm Res Paediatr 11
Diagnosis, and Treatment DOI: 10.1159/000479371
Furthermore, the criteria to define the ultrasonographic ever, in adolescents, AMH should not be used as a crite-
pattern of PCOS continue to be modified [173]. rion of PCOS since there is a weaker association of AMH
The anatomic appearance of the ovary changes with levels with the disorder [188, 189]. This divergence may
age [174]. Ovarian volume increases during puberty and be due to the presence of higher AMH serum levels in
reaches the adult volume in the years following men- healthy adolescents compared to adult women, with a
arche. It remains stable in young adulthood and decreas- wide normal range [178, 180, 190, 191].
es after the middle of the fourth decade of life. [175]. Fol- Besides AMH, several biomarkers may be associated
licle size also changes with age, and the greatest number with PCOS. A high ratio of total testosterone to dihy-
of small follicles is observed during adolescence and drotestosterone (T/DHT) is associated with an adverse
young adulthood, with a significant decrease in follicle metabolic phenotype in PCOS patients [192]. Munzker et
count with age [176]. al. [192] found that T/DHT was significantly higher in
The ultrasonographic diagnosis of PCOM has been PCOS patients than in non-PCOS patients, and T/DHT
standardized for adults using the transvaginal route. In was even higher in obese PCOS patients than in non-
adolescents, however, most exams are performed by the obese PCOS patients. This phenomenon may be linked to
transabdominal route, where the high physiologic follicle conversion of testosterone to DHT by the 5α-reductase
number may render the follicle count an unreliable crite- enzymes, and may ultimately be useful to assess for the
rion for the diagnosis of PCOM. The importance of using diagnosis of PCOS.
appropriate diagnostic criteria of PCOM in adolescents is Proteomic profiling studies have indicated specific
emphasized because application of the adult criteria can proteins to be used as biomarkers for PCOS. Sarray and
lead to a falsely elevated prevalence of PCOM (30–40% Almawi [193] detected significantly elevated sCD40L in
range) [177, 178]. Therefore, ovarian volume is better women with PCOS. They posited that sCD40L, a trans-
suited than follicle count to determine the presence of membrane glycoprotein that regulates several cell types
PCOM in adolescence [179]. The Androgen Excess and in the inflammatory network, can be used as a predictor
PCOS Society suggested that an ovarian volume of 10 mL for PCOS in a Bahraini Arab population [193]. Though
be recommended for the diagnosis of PCOM in adoles- this result cannot be generalized across ethnic groups, it
cents [132]. Later, based on an ovarian volume larger than is an important finding for future replication and valida-
2 SD above the mean in the healthy adolescent population tion. HSP90B1, a stress-inducible chaperone protein as-
[180], an enlarged ovarian volume of 12 mL was recom- sociated with the growth of cancerous cells, has also been
mended by an international consensus [179]. identified as a potential biomarker for PCOS [194].
Available data suggest that among non-obese, non- HSP90B1 may have a role in promoting granulosa cellu-
hirsute girls with regular menstrual cycles, PCOM is not lar activity in the ovary, leading to PCOS. Further study
associated with hyperandrogenism or IR. Similar levels of is necessary to confirm this action [194].
androgens and indexes of insulin sensitivity were ob- Alongside proteomics and hormone discoveries,
served in healthy girls with and without PCOM [181]. promising preliminary work in the use of microRNA for
Nevertheless, persistence of enlarged ovaries and men- PCOS diagnosis is underway [195]. Circulating or ovari-
strual irregularities may foretell the future development an miRNAs could potentially modulate steroidogenesis
of PCOS [176, 182, 183]. and ovarian function in women with PCOS [195]. Bio-
markers are useful tools in general, and progress contin-
3. Biomarkers for PCOS ues in the discovery of newer biomarkers to assist in mak-
Limited data are available regarding newer biomark- ing the diagnosis of PCOS.
ers, except for AMH, nor has their utility to aid in the es-
tablishment of the diagnosis of PCOS in adolescence been 4. IR in the Context of PCOS
completely verified. AMH is a glycoprotein secreted by IR and compensatory hyperinsulinemia are not con-
the granulosa cells of small, growing follicles. As noted sidered to be diagnostic criteria for PCOS. Yet, IR and
above, animal studies have inferred a possible role for hyperinsulinemia have been documented in women with
AMH in the ontogeny of PCOS. AMH serum levels cor- PCOS since the late 1980s, when some studies showed
relate with the number of small antral follicles (2–5 mm) that obese women with PCOS had significantly increased
identified by transvaginal ultrasound in adult women glucose levels during an oral glucose tolerance test com-
[184, 185]. Elevated AMH levels have been a consistent pared to age- and weight-matched ovulatory women with
hormone finding in women with PCOS [186, 187]. How- elevated plasma androgen levels and control women.
12 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
Moreover, the presence of some degree of IR in subjects 2. Polycystic Ovarian Morphology
with PCOS is corroborated by the high prevalence of glu- • The presence of PCOM in an adolescent who does not
cose intolerance in obese PCOS adolescents. Estimated at have hyperandrogenism/oligo-anovulation does not
40% [37], glucose intolerance in obese PCOS adoles- indicate a diagnosis of PCOS (Level A).
cents is much higher than in the general US population • The measurement of ovarian volume, follicle number
of obese adolescents in which the prevalence of impaired and size, and uterine dimensions may be useful in the
glucose tolerance is about 15–20% [196]. evaluation of amenorrhea, but is not needed for PCOS
The diagnosis of IR in PCOS is unfortunately con- diagnosis in adolescents (Level A).
founded by the variety of definitions used in different
studies [16, 18, 37, 197]. IR may be measured directly us- 3. Biomarkers of PCOS
ing a euglycemic insulin clamp (requiring an intravenous • The use of AMH, T/DHT ratios, and specific proteins
line), but is usually measured indirectly, through the oral or microRNA as biomarkers of PCOS has not been
glucose tolerance test, or most commonly through fasting validated in adolescents (Level C.).
levels of glucose and insulin [197]. Though the derived
indices obtained from indirect measures may be some- 4. Insulin Resistance
what less accurate than direct, whole-body measurement, • IR, compensatory hyperinsulinemia, or obesity should
their utility as non-invasive measures of IR is vital. Indi- not be considered as diagnostic criteria for PCOS in
rect measurements of IR may be calculated in a variety adolescents (Level A).
of ways. These include fasting glucose to insulin ratio,
early insulin response, homeostatic model assessment
(HOMA), the Matsuda Index, and oral Sg index [197– C. Treatment of PCOS
201]. These methods are particularly useful in individual
or population studies. No pharmacological treatment has been approved so
far by FDA/EMA for use in adolescents with PCOS; how-
ever, some pharmacological interventions have been used
B. Diagnosis: Conclusions with Level of Evidence to manage PCOS symptoms. In the following sections,
the baseline and additive pharmacological treatments
1. Clinical Features of PCOS and their potential benefits, as well as reproductive as-
• Moderate to severe hirsutism constitutes clinical evi- pects in PCOS adolescents are discussed. Doses and se-
dence of androgen excess (Level B). quences of intervention combinations need to be indi-
• Mild hirsutism may be a sign of androgen excess when vidualized.
associated with menstrual irregularities (Level C).
• Moderate or severe inflammatory acne unresponsive 1. Baseline Treatment
to topical therapy may require investigation of andro- 1.1. Lifestyle Intervention
gen excess (Level C). Weight loss and increased physical exercise are gener-
• Isolated acne and/or alopecia should not be consid- ally recommended as the first-line therapy in overweight
ered diagnostic criteria for PCOS in adolescence (Lev- or obese girls [134]. Two small randomized controlled
el C). trials (RCTs) [202, 203] and one well-controlled clinical
• Persistent menstrual disturbances (oligomenorrhea study [204] in overweight PCOS girls have shown that the
and secondary amenorrhea) beyond 2 years after men- combination of weight loss and intensified exercise de-
arche or primary amenorrhea in girls with completed creases testosterone levels and the free androgen index,
puberty may suggest androgen excess (Level B). increases SHBG concentrations, and normalizes men-
• Biochemical hyperandrogenism should be defined strual regularity comparably to drug therapy, and is de-
based on the methodology used, as no clear cutoff for void of side effects. The combination of lifestyle interven-
testosterone concentrations exists for adolescents tion with medications normalized more androgen levels
(Level A). and menses in one of these studies [204]. However, long-
• Biochemical evidence of hyperandrogenism based on term data reporting sustained benefits on cycle regularity
elevations of total and/or free testosterone measured or on pregnancy outcomes after weight loss in adolescent
in a reliable reference laboratory documents hyperan- girls are lacking.
drogenemia in a symptomatic adolescent (Level B).
Update: PCOS Pathophysiology, Horm Res Paediatr 13
Diagnosis, and Treatment DOI: 10.1159/000479371
Cardiovascular risk factors such as hypertension, dys- Only 2 RCTs have evaluated the effect of photoepilation
lipidemia, and impaired glucose tolerance, as well as ear- in selected PCOS patients aged 16 years or older, showing
ly markers of atherosclerosis such as carotid intima-me- the benefits of laser therapy on facial hirsutism [214] and
dia thickness also improved after lifestyle intervention the superiority of alexandrite laser over IPL [215].
[134]. Weight loss, but not participation in lifestyle inter- Two RCTs performed in hirsute patients aged 16 years
vention itself, predicted the amelioration of components or older reported the benefits of topical eflornithine HCl
of PCOS [134]. Extremely obese adolescents often re- 13.9% cream applied twice daily in reducing facial hirsut-
spond poorly to lifestyle intervention [205]. A reduction ism [216]. The safety profile was good and percutaneous
of BMI SDS of 0.25 or greater [206] and/or 30 min per day absorption was minimal. Drawbacks included non-re-
of moderate to vigorous physical activity resulted in an sponse in 30% of users and regrowth to pretreatment lev-
improvement of cardiovascular risk factors in adoles- els within 8 weeks of discontinuation. Three other RCTs
cents with PCOS [207]. performed in hirsute women showed the ability of topical
Lifestyle intervention should be based on the combi- eflornithine when added to photoepilation to promote
nation of calorie-restricted diets (with no evidence that faster and more complete laser removal of facial hirsut-
one type of diet is superior for adolescents), behavioral ism and to reduce hair regrowth between laser sessions
treatment, and exercise [208]. Along these lines, a meta- and after cessation of IPL use [216, 217]. Laser epilation
analysis has demonstrated the benefits of dietary modifi- is most effective when used to treat areas of full, dark hair
cation in young women with PCOS [209]. Increasing on light-skinned people. The studies reporting the effects
physical activity from moderate to vigorous is effective in of topical finasteride on idiopathic hirsutism are limited
reducing the development of metabolic syndrome in nor- and contradictory.
mal-weight girls [209]. However, no large RCTs support We suggest photoepilation as first-line management of
the benefits of exclusive weight loss in normal-weight localized hirsutism in PCOS; diode and alexandrite lasers
PCOS adolescents. are preferred. Topical eflornithine is recommended as an
Decreasing sedentary behavior is at least as important adjuvant to photoepilation in cases with laser-resistant
as increasing physical activity [210]. Furthermore, family facial hirsutism or as monotherapy in patients with facial
treatment is an essential component in lifestyle interven- hirsutism where photoepilation is not indicated. The use
tion since parents’ readiness to change habits affects the of topical finasteride is not recommended based on the
outcome [208, 210]. existing data.
1.2 Local Therapies/Cosmetics 2. Additive Pharmaceuticals
Cosmetic hair-removal methods for hirsutism include Pharmacological interventions that have been used in
bleaching, chemical epilation, plucking, waxing, shaving, adolescent PCOS are included in Table 2.
electrolysis, and laser hair removal. Although only the lat-
ter result in permanent – albeit partial – hair removal, ef- 2.1. Metformin
ficacy and safety of electrolysis is not supported by any Metformin is the only insulin sensitizer that has been
RCT. evaluated in double-blind RCTs as single medication for
Evidence based on 11 RCTs [211] and 21 controlled adolescent PCOS; metformin use has increased over the
trials [212] supports the efficacy for up to 6 months of last 10 years despite not being licensed for PCOS [218].
partial hair removal with laser or intense pulsed light A meta-analysis of metformin use with and without
(IPL), despite a great variability following photoepilation lifestyle changes in PCOS up to August 2014 showed ben-
[212]. Partial long-term hair removal efficacy (beyond 6 eficial effects on BMI and menstrual cycles [219]. Of the
months) has been observed for all laser therapies after re- 12 RCTs included, 2 were performed in adolescents [202,
petitive treatments, although the data are limited [212]. 220]. The meta-analysis also highlighted the many limita-
The data comparing different laser methods are few and tions of the RCTs such as small sample size, short dura-
contradictory; however, the available studies show that tion (most trials had a duration of 6 months), and a mod-
diode and alexandrite offer the higher success rate, where- erate risk for bias.
as Nd:Yag provides the lowest [213]. The studies compar- Observational studies and 6 randomized trials [202,
ing laser and IPL devices are few and of low quality; all 220–224] (Table 2) have demonstrated short-term ben-
have been performed in adults with mixed forms of hir- eficial effects of metformin in PCOS adolescents who
sutism, hyperandrogenism, or unwanted hair growth. were mostly overweight or obese. There are only 2 small
14 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
Table 2. Medications used in the treatment of polycystic ovary syndrome in adolescent girls
Medication Mechanism(s) of action Dosage Side effects Contraindications
Estroprogestagen Inhibition of ovarian androgen secretion 21 out of 28 Breast tenderness, headache, Pregnancy, uncontrolled
OCP and increase in hepatic SHBG production, days/month increased risk of venous hypertension, liver dysfunction,
resulting in less circulating free androgens thromboembolism, tend to increase complicated valvular heart
insulin resistance disease, migraines with aura or
focal neurologic symptoms,
thromboembolism, diabetes
complications, organ
transplantation
Metformin Upregulation of the energy sensors 850 mg/day Gastrointestinal discomfort1, Renal and liver dysfunction,
STK11 and AMPK up to 1 g lactic acidosis2 surgery, use of contrast agents,
Improvement of insulin sensitivity in b.i.d. heart failure, alcoholism,
muscle and adipose tissue metabolic acidosis, dehydration,
Downregulation of hepatic gluconeogenesis hypoxemia
(improves fasting blood glucose)
Increase of GLP-1 secretion and GLP-1
receptor expression (improves postprandial
blood glucose)
Decrease of ovarian and adrenal androgen
production
Pioglitazone Peroxisome proliferator-activated 7.5 mg/day Weight gain (higher doses), Pregnancy, liver dysfunction,
receptor-γ activator up to 30 mg/ bladder cancer risk inconclusive bladder cancer
At low dose, inhibition of CDK5- day results; studies include only male
mediated phosphorylation of peroxisome diabetic patients >40 years, risk
proliferator-activated receptor-γ with cumulative doses >28,000 mg
Flutamide Androgen receptor blockade 62.5 mg/day Dose-dependent hepatotoxicity Pregnancy, renal and liver
up to 250 Absent at doses of 1 mg/kg/day dysfunction
mg/day Feminization of male fetuses
Spironolactone Aldosterone antagonism 50–200 mg/ Mostly dose-dependent: irregular Pregnancy, renal failure,
Androgen receptor blockade day menstrual bleeding, headache, hyperkalemia
hypotension, nausea, decreased
libido, feminization of male fetuses
Cyproterone Competition with dihydrotestosterone at 50–100 mg/ Liver toxicity, irregular menstrual Pregnancy, renal and liver
acetate receptor level day bleeding, nausea, decreased libido, dysfunction
Inhibition of 5α-reductase, prevents Combined feminization of male fetuses
conversion of testosterone to with OCP
dihydrotestosterone 2 mg/day
Finasteride Inhibition of 5α-reductase, prevents 1–5 mg/day Feminization of male fetuses, liver Pregnancy
conversion of testosterone to dysfunction (rare)
dihydrotestosterone
OCP, oral contraceptive pill; SHBG, sex hormone-binding globulin; STK11, serine/threonine protein kinase; AMPK, adenosine monophosphate-
activated protein kinase; b.i.d., bis in die. 1 Gradually increasing doses minimizes the appearance of gastrointestinal symptoms. 2 Older patients with type
2 diabetes and renal failure.
observational studies in non-obese PCOS adolescents A recent meta-analysis of metformin versus oral con-
with hyperinsulinemia showing improvement in ovula- traceptive pills (OCP) including 4 RCTs [202, 221, 224]
tion and testosterone levels with doses as low as 850 mg/ and a total of 170 adolescents showed that metformin and
day [225, 226]. Most studies failed to accurately report OCP had similar benefits on hirsutism, triglycerides, and
side effects and adherence to interventions. Overall, HDL cholesterol. Metformin was accompanied by a
metformin was associated with gastrointestinal dis- greater improvement of BMI, while the use of OCP was
comfort, but no serious adverse effects have been re- associated with improvement in menstrual regularity
ported. (modest) and acne (mild). The conclusion was that these
Update: PCOS Pathophysiology, Horm Res Paediatr 15
Diagnosis, and Treatment DOI: 10.1159/000479371
estimates were derived from low-quality evidence involv- provements in hirsutism, but total and LDL cholesterol
ing small studies and that further research is required were increased by both formulations [235]. Additionally,
[227]. there was evidence for worsening of HOMA-IR and fast-
ing glycemia with both preparations [236]. Metabolic
2.2 Anti-Androgens changes overall, however, did not result in significant
Two types of anti-androgens are used in the manage- concentrations outside the normal ranges. In young
ment of PCOS: androgen receptor blockers like spirono- women with PCOS (aged 20–25 years) treated with an
lactone, flutamide, and the third generation progestin, OCP containing drospirenone versus a combined contra-
cyproterone acetate, and inhibitors of 5-alpha reductase ceptive vaginal ring, an RCT suggested that both methods
such as finasteride, which prevents the conversion of tes- worsened the lipid profile, but OCP significantly wors-
tosterone to DHT. In adolescents with PCOS, direct com- ened triglycerides while remaining within the normal
parisons of the various anti-androgens or RCTs are not range [237]. In adult women, an RCT involving OCP with
available [228, 229]. Spironolactone is the most common- 3 different progestins (desogestrel, drospirenone, and cy-
ly used because of its availability and safety profile, with proterone acetate) showed identical metabolic impact
an initial dose of 25 mg/day gradually increasing up to [238]. Overall, high-quality RCTs of specific OCP formu-
200 mg/day. At initiation, spironolactone may be associ- lations for adolescents with PCOS are lacking to fully in-
ated with transient menstrual irregularity or spotting, form decision-making in this population; no specific for-
breast tenderness, and occasionally fatigue or orthostasis mulation can be recommended over another.
from volume depletion. Flutamide is not available in
some countries and is used sparingly because of concerns 2.4. Combination Treatments
regarding its potential hepatotoxicity at high doses (>250 Combination treatments under development for
mg/day). Evidence indicates that 1 mg/kg/day is effective PCOS in adolescent girls aim at improving the function
and not hepatotoxic, even with extended use [230]. Data of multiple pathways and at obtaining additive/synergis-
on efficacy of spironolactone compared to flutamide are tic actions that lead collectively to a profile with high ben-
limited, and the methodological quality of the studies is efit and low risk. Lifestyle improvement is the baseline
low [231]. Anti-androgens significantly reduce hirsutism treatment for most adolescent girls with PCOS, particu-
compared with placebo [232] and normalize menstrual larly if overweight or obese (see Lifestyle Intervention
cyclicity and endocrine-metabolic variables better than section C.1.1.). In most adolescents with PCOS, the addi-
monotherapy with metformin [231]. The efficacy is en- tion of an OCP will be followed by a reduction of PCOS
hanced when combined with OCP, metformin, or other symptoms via normalization of circulating free andro-
anti-androgens [231–234]. In sexually active adolescents, gens (primarily due to increased circulating SHBG con-
anti-androgens should only be used when adequate con- centrations) and via pseudo-normalization of the men-
traceptive measures are ensured, to avoid incomplete vir- strual pattern within a state of anovulatory infertility (see
ilization of male fetuses. Oral Contraceptive Pills section C.2.3.).
Slower reductions of PCOS symptoms can be obtained
2.3. Oral Contraceptive Pills with combinations of insulin-sensitizing and anti-andro-
Combination OCP containing an estrogen component genic generics, the most promising low-dose combina-
(typically ethinylestradiol) and a progestin component tion nowadays perhaps being that of metformin (850 mg/
address multiple concerns in adolescents with PCOS. An day), spironolactone (50 mg/day), and pioglitazone (7.5
increase in SHBG and decreased LH release due to the mg/day) [239]. This triple combination appears to nor-
estrogen component leads to a decreased free androgen malize cardiovascular risk and body composition more
index, and the progestin component allows for suppres- than combinations of only metformin and an anti-andro-
sion of endometrial proliferation and regular withdrawal gen [54, 234] and to result in a more favorable post-treat-
bleeding. As such, there is improvement in acne and hir- ment pattern of circulating androgens and ovulation rates
sutism and reduction in menstrual irregularity with OCP. than oral contraceptive intake [239].
Unfortunately, there are few RCTs comparing the relative
efficacy or metabolic impact of the different formulations 3. Reproductive Aspects
of hormonal contraceptives in adolescents. An RCT com- 3.1. Ovulation
paring the progestins desogestrel and cyproterone acetate Ovulation may occur in about 10% of adult women
in combination with ethinylestradiol found equal im- with PCOS. The frequency of ovulation in adolescent
16 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
PCOS is unknown. In normal puberty, menarche is fol- 4. Transition
lowed by an interval of anovulatory bleeding of variable Management of girls with PCOS should focus on ap-
length. During this interval, synchronization of hypotha- propriate diagnosis, reduction of symptoms in adoles-
lamic-pituitary-ovarian activity takes place that leads to cence, and improvement of post-treatment health in
ovulation and regular menstrual cycles. In adolescent adulthood. Specific therapeutic goals include attenua-
PCOS, there is persisting anovulation in most but not all tion of pregestational oligo-anovulation (thus the need
individuals. Notably, girls with premature pubarche (PP) for assisted reproduction) and reduction of gestational
that are at risk for PCOS may exhibit ovulatory frequency complications such as diabetes mellitus, preeclampsia,
(25%) during early postmenarche (1–3 years), which is and preterm delivery [245]. Given the apparent role of
indistinguishable from non-PP individuals [240]. Beyond hepato-visceral fat excess in the pathogenesis of anovula-
3 years after menarche, the ovulatory rate in PP was re- tory androgen excess [246, 247], PCOS therapy in ado-
duced. It was also noted that some early postmenarchal lescence should also aim at reducing hepato-visceral ad-
adolescents (<3 years) with irregular menstruation and iposity via lifestyle measures leading to weight loss in
elevated androgen levels followed for 3 years developed obese girls (see Lifestyle Intervention section C.1.1.) and
regular ovulatory cycles [182]. These findings suggest via pharmacological measures. These approaches would
that in some adolescents with or at risk for PCOS, normal enhance the preferential loss of central fat in non-obese
ovulatory function may exist or emerge with time and girls with a low subcutaneous fat storage capacity, such
present as ovulatory adolescent PCOS. as girls with a lipodystrophy, girls with ethnic back-
grounds associated with a high risk of developing diabe-
3.2 Contraception tes, and girls with a history of prenatal growth restraint
There is no evidence to suggest a decreased pregnancy [54]. The more low-risk and/or low-cost interventions
risk in adolescents with PCOS compared to that of adult for PCOS during adolescence, the fewer high-risk and/or
women with PCOS. Given that ovulation may occur high-cost treatments will be needed during adulthood,
spontaneously despite a pattern of chronic menstrual ir- and the better the outlook will be for the offspring of
regularity, contraceptive decision-making is important PCOS mothers.
in sexually active adolescents with this disorder. Men-
strual irregularity and menorrhagia in adolescents with
PCOS can be difficult to manage without hormonal in- C. Treatment: Conclusions with Level of Evidence
tervention. Accordingly, OCP are recommended as a
first-line therapy for adolescents with PCOS consistent 1. Baseline Treatments
with published guidelines [134]. The anti-androgenic 1.1. Lifestyle Intervention
properties of OCP and the benefit of menstrual control • Lifestyle intervention should be based on the combi-
make them an excellent contraceptive choice in young nation of calorie-restricted diets, behavioral treat-
women with PCOS. Medical contraindications for the ment, and exercise (Level A).
use of OCP are outlined in the 2010 Center for Disease • Combined weight loss and physical exercise are the
Control guidelines [241]. The potential metabolic impact first-line therapy in overweight and obese girls (Level
of OCP in PCOS is outlined in the above section (see Oral C). They decrease androgen levels, normalize men-
Contraceptives section C.2.3.). The use of progestin-only strual cycles (Level A), and improve markers of cardio-
contraception, such as depot medroxyprogesterone ace- metabolic health (Level B).
tate, is associated with weight gain in adolescents and • Extremely obese adolescents respond poorly to life-
possibly bone loss, although this is recoverable [242, style intervention (Level B).
243]. Progestin-only therapy does not raise SHBG as do • In normal-weight girls, increasing physical activity is
OCP containing ethinylestradiol. The progestin-only in- effective in reducing the development of metabolic
trauterine device may be an alternative first-line therapy syndrome (Level C). However, the benefits of exclu-
given the low systemic impact and overall high contra- sive weight loss in these adolescents are not supported
ceptive effectiveness [244]. Overall, there is a lack of by RCTs (Level C).
high-quality RCTs of contraceptive treatment options
for adolescents with PCOS to fully inform decision-mak- 1.2 Local Therapies/Cosmetic
ing in this population. • Photoepilation is the first-line management of localized
hirsutism in PCOS (Level B). Diode and alexandrite la-
Update: PCOS Pathophysiology, Horm Res Paediatr 17
Diagnosis, and Treatment DOI: 10.1159/000479371
sers are preferred (Level C). The alexandrite laser is su- and thus, attenuating pregestational oligo-anovula-
perior to IPL methods in facial hirsutism (Level B). tion, and reducing gestational complications such as
• Topical eflornithine is recommended as an adjuvant diabetes mellitus, preeclampsia, and preterm delivery
to photoepilation in girls with laser-resistant facial (Level B).
hirsutism aged 16 years or older, or as monotherapy
in those where photoepilation is not indicated (Level
A). Conclusion
• The use of topical finasteride is not recommended
based on existing data (Level C). This first global update on the pathophysiology, diag-
nosis, and treatment of adolescent PCOS is the outcome
2. Additive Pharmaceuticals of an international collaborative effort initiated by Pedi-
2.1 Metformin atric Endocrine Societies.
• Metformin has beneficial effects in overweight or One aim of this update was to offer a more develop-
obese adolescents with PCOS, but only short-term mental perspective than previous reports on adolescent
data are available (Level A). PCOS. The authors have attempted to merge many opin-
• In non-obese adolescents with PCOS and hyperinsu- ions on much evidence, and they realize that there may be
linemia, metformin improves ovulation and testoster- apparent inconsistencies between consecutive sections.
one levels (Level B). Hence, this report discloses the many uncertainties and
knowledge gaps persisting at the time of writing.
2.2. Anti-Androgens A second aim of this initiative was to document the
• Anti-androgens reduce androgen excess features more main directions of past, present, and future investigations
than metformin in monotherapy (Level B). Spirono- into adolescent PCOS. In the past, the keywords for
lactone is the most commonly used albeit data on ef- pathogenesis, diagnosis, and treatment may have been,
ficacy compared to flutamide are limited (Level C). respectively, ovarian and adrenal steroidogenesis, IR and
• Anti-androgens should only be used when contracep- LH hypersecretion; hirsutism and menstrual pattern; cos-
tive measures are guaranteed. metics and oral contraceptives. Current focuses have
shifted to include (epi)genetics and body adiposity; an-
2.3. Oral Contraceptive Pills drogens (by LC-MS/MS) and ovulatory function; lifestyle
• There are no high-quality RCTs of specific OCP for- measures, insulin sensitization and anti-androgens. In
mulations for adolescents with PCOS to help decision- the near future, the keywords are expected to include ec-
making in this population, and no specific formulation topic lipids and microbiome; miRNAs, metabolomics,
can be recommended over another (Level B). and adipo-, hepato-, myo-, and osteo-kines. Treatment
will aim at a slow but steady return to an overall healthy
2.4. Combination Treatments state with combination therapies that may vary over time
• Where available, triple low-dose combinations of in- and allow for spontaneous ovulations, uncomplicated
sulin-sensitizing and anti-androgenic generics nor- pregnancies, and healthy offspring.
malize cardiovascular risk and body composition Finally and most importantly, this global update
more than combinations of only metformin and an should contribute to improvement of the care worldwide
anti-androgen and result in a more favorable post- for adolescent girls with PCOS.
treatment pattern of circulating androgens and ovula-
tion rates than OCP intake (Level A).
Appendix
3. Reproductive Aspects S.E.O., S.F.W., and P.A.L. are members of the Pediatric Endo-
• In some adolescents with or at risk for PCOS, normal crine Society (PES); L.I., S.F.W., F.D., A.G., A.L.-B., K.O., T.R., N.S.,
ovulatory function may exist or emerge with time and F.Z., and P.A.L. are members of the European Society for Paediatric
present as ovulatory adolescent PCOS (Level A). Endocrinology (ESPE); C.G.R. and A.S.P. are members of the Aus-
tralasian Paediatric Endocrine Group (APEG); P.D. is a member of
the Asia Pacific Paediatric Endocrine Society (APPES); D.J. is a mem-
4. Transition ber of the African Society for Paediatric and Adolescent Endocrinol-
• PCOS therapy in adolescence should aim at decreasing ogy (ASPAE); Xiao-Ping Luo is a member of the Chinese Society of
hepato-visceral adiposity, enhancing central fat loss, Pediatric Endocrinology and Metabolism (CSPEM); R.H. is a mem-
18 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
ber of the Japanese Society for Pediatric Endocrinology (JSPE); E.C. Acknowledgement
is a member of the Sociedad Latinoamericana de Endocrinología
Pediátrica (SLEP); N.S.E., H.A., and A.D. are members of the Arab We would like to acknowledge Dr. Xiao-Ping Luo for represent-
Society of Paediatric Endocrinology and Diabetes (ASPED); P.D. is ing the Chinese Society of Pediatric Endocrinology and Metabolism
a member of the Indian Society for Pediatric and Adolescent Endo- (CSPEM).
crinology (ISPAE); S.F.W., S.E.O., R.J.C., and K.M.H. are members
of The Androgen Excess and PCOS Society (AE-PCOS); and R.J.A.,
and M.T.-S. are members of the Endocrine Society (ES).
References
1 Azziz R, Dumesic DA, Goodarzi MO: Poly- 13 Tee MK, Speek M, Legeza B, Modi B, Teves 24 Stepto NK, Cassar S, Joham AE, Hutchison
cystic ovary syndrome: an ancient disorder? ME, McAllister JM, Strauss JF 3rd, Miller WL: SK, Harrison CL, Goldstein RF, Teede HJ:
Fertil Steril 2011;95:1544–1548. Alternative splicing of DENND1A, a PCOS Women with polycystic ovary syndrome have
2 Unluturk U, Sezgin E, Yildiz BO: Evolution- candidate gene, generates variant 2. Mol Cell intrinsic insulin resistance on euglycaemic-
ary determinants of polycystic ovary syn- Endocrinol 2016;434:25–35. hyperinsulaemic clamp. Hum Reprod 2013;
drome: part 1. Fertil Steril 2016;106:33–41. 14 Turcu A, Smith JM, Auchus R, Rainey WE: Ad- 28:777–784.
3 Azziz R, Carmina E, Chen Z, Dunaif A, Laven renal androgens and androgen precursors-def- 25 Morciano, A. Romani F, Sagnella F, Scarinci
JS, Legro RS, Lizneva D, Natterson-Horowtiz inition, synthesis, regulation and physiologic E, Palla C, Moro F, Tropea A, Policola C, Del-
B, Teede HJ, Yildiz BO: Polycystic ovary syn- actions. Compr Physiol 2014;4:1369–1381. la Casa S, Guido M, Lanzone A, Apa R: As-
drome. Nat Rev Dis Primers 2016;2:16057. 15 O’Reilly MW, Kempegowda P, Jenkinson C, sessment of insulin resistance in lean women
4 Oberfield SE, Sopher AB, Gerken AT: Ap- Taylor AE, Quanson JL, Storbeck KH, Arlt W: with polycystic ovary syndrome. Fertil Steril
proach to the girl with early onset of pubic 11-oxygenated C19 steroids are the predomi- 2014;102:250–256.
hair. J Clin Endocrinol Metab 2011;96:1610– nant androgens in polycystic ovary syn- 26 Willis D, Franks S: Insulin action in human
1622. drome. J Clin Endocrinol Metab 2017; 102: granulosa cells from normal and polycystic ova-
5 Chang AY, Abdullah SM, Jain T, Stanek HG, 840–848. ries is mediated by the insulin receptor and not
Das SR, McGuire DK, Auchus RJ, de Lemos 16 Dunaif A, Segal KR, Shelley DR, Green G, Do- the type-I insulin-like growth factor receptor. J
JA: Associations among androgens, estro- brjansky A, Licholai T: Evidence for distinc- Clin Endocrinol Metab 1995;80:3788–3790.
gens, and natriuretic peptides in young wom- tive and intrinsic defects in insulin action in 27 Nestler JE, Powers LP, Matt DW, Steingold
en: observations from the Dallas Heart Study. polycystic ovary syndrome. Diabetes 1992;41: KA, Plymate SR, Rittmaster RS, Clore JN,
J Am Coll Cardiol 2007;49:109–116. 1257–1266. Blackard WG: A direct effect of hyperinsu-
6 Hsueh AJ, Kawamura K, Cheng Y, Fauser BC: 17 Dunaif A, Graf M, Mandeli J, Laumas V, Do- linemia on serum sex hormone-binding glob-
Intraovarian control of early folliculogenesis. brjansky A: Characterization of groups of hy- ulin levels in obese women with the polycystic
Endocr Rev 2015;36:1–24. perandrogenic women with acanthosis nigri- ovary syndrome. J Clin Endocrinol Metab
7 Franks S, Stark J, Hardy K: Follicle dynamics cans, impaired glucose tolerance, and/or hy- 1991;72:83–89.
and anovulation in polycystic ovary syn- perinsulinemia. J Clin Endocrinol Metab 28 Adashi EY, Hsueh AJW, Yen SSC: Insulin en-
drome. Hum Reprod Update 2008; 14: 367– 1987;65:499–507. hancement of luteinizing hormone and follicle-
378. 18 Diamanti-Kandarakis E, Dunaif A: Insulin re- stimulating hormone release by cultured pitu-
8 Lebbe M, Woodruff TK: Involvement of an- sistance and the polycystic ovary syndrome itary cells. Endocrinology 1981;108:1441–1449.
drogens in ovarian health and disease. Mol revisited: an update on mechanisms and im- 29 Torchen LC, Fogel NR, Brickman WJ, Papa-
Hum Reprod 2013:19:828–837. plications. Endocr Rev 2012;33:981–1030. rodis R, Dunaif A: Persistent apparent pan-
9 Webber LJ, Stubbs S, Stark J, Trew GH, Mar- 19 Moran A, Jacobs DR Jr, Steinberger J, Hong creatic β-cell defects in premenarchal PCOS
gara R, Hardy K, Franks S: Formation and CP, Prineas R, Luepker R, Sinaiko AR: Insulin relatives. J Clin Endocrinol Metab 2014; 99:
early development of follicles in the polycystic resistance during puberty: results from clamp 3855–3862.
ovary. Lancet 2003;362:1017–1021. studies in 357 children. Diabetes 1999; 48: 30 Taylor SI, Cama A, Accili D, Barbetti F, Quon
10 Nelson VL, Legro RS, Strauss JF 3rd, McAl- 2039–2044. MJ, de la Luz Sierra M, Suzuki Y, Koller E,
lister JM: Augmented androgen production is 20 Amiel SA, Sherwin RS, Simonson DC, Lauri- Levy-Toledano R, Wertheimer E, Moncadaj
a stable steroidogenic phenotype of propagat- tano AA, Tamborlane WV: Impaired insulin VY, Kadowaki H, Kadowaki T: Mutations in
ed theca cells from polycystic ovaries. Mol En- action in puberty. A contributing factor to the insulin receptor gene. Endocr Rev 1992;
docrinol 1999;13:946–957. poor glycemic control in adolescents with di- 13:566–595.
11 Marti N, Galván JA, Pandey AV, Trippel M, abetes. N Engl J Med 1986;315:215–219. 31 Moller DE, Flier JS: Insulin resistance – mech-
Tapia C, Müller M, Perren A, Flück CE: Genes 21 Ball GD, Huang TT, Gower BA, Cruz ML, anisms, syndromes, and implications. N Engl
and proteins of the alternative steroid back- Shaibi GQ, Weigensberg MJ, Goran MI: Lon- J Med 1991;325:938–948.
door pathway for dihydrotestosterone synthe- gitudinal changes in insulin sensitivity, insu- 32 Corbould A: Effects of androgens on insulin
sis are expressed in the human ovary and seem lin secretion, and beta-cell function during action in women: is androgen excess a com-
enhanced in the polycystic ovary syndrome. puberty. J Pediatr 2006;148:16–22. ponent of female metabolic syndrome? Dia-
Mol Cell Endocrinol 2017;441:116–123. 22 Saenger P: Metabolic consequences of growth betes Metab Res Rev 2008;24:520–532.
12 McAllister JM, Modi B, Miller BA, Biegler J, hormone treatment in paediatric practice. 33 Soldani, R, Cagnacci A, Yen SSC: Insulin in-
Bruggeman R, Legro RS, Strauss JF 3rd: Over- Horm Res 2000;53(suppl 1):60–69. sulin-like growth factor I (IGF-I) and IGF-II
expression of a DENND1A isoform produces 23 Geffner ME, Golde DW: Selective insulin ac- enhance basal and gonadotrophin-releasing
a polycystic ovary syndrome theca pheno- tion on skin, ovary, and heart in insulin-resis- hormone-stimulated luteinizing hormone re-
type. Proc Natl Acad Sci USA 2014; 111: tant states. Diabetes Care 1988;11:500–505. lease from rat anterior pituitary cells in vitro.
E1519–E1527. Eur J Endocrinol 1994;131:641–645.
Update: PCOS Pathophysiology, Horm Res Paediatr 19
Diagnosis, and Treatment DOI: 10.1159/000479371
34 O’Connor A, Phelan N, Tun TK, Boran G, Gib- 46 Escobar-Morreale HF, Luque-Ramírez M, 59 Badin PM, Langin D, Moro C: Dynamics of
ney J, Roche HM: High-molecular-weight adi- González F: Circulating inflammatory mark- skeletal muscle lipid pools. Trends Endocri-
ponectin is selectively reduced in women with ers in polycystic ovary syndrome: a system- nol Metab 2013;24:607–615.
polycystic ovary syndrome independent of body atic review and metaanalysis. Fertil Steril 60 Chavez JA, Summers SA: A ceramide-centric
mass index and severity of insulin resistance. J 2011;95:1048–1058. view of insulin resistance. Cell Metab 2012;15:
Clin Endocrinol Metab 2010;95:1378–1385. 47 Spranger J, Kroke A, Mohlig M, Hoffmann K, 585–594.
35 O’Reilly M, Gathercole L, Capper F, Arlt W, Bergmann MM, Ristow M, Boeing H, Pfeiffer 61 Bruning JC, Gautam D, Burks DJ, Gillette J,
Tomlinson J: Effect of insulin on AKR1C3 ex- AF: Inflammatory cytokines and the risk to de- Schubert M, Orban PC, Klein R, Krone W,
pression in female adipose tissue: in-vivo and velop type 2 diabetes: Results of the prospective Muller-Wieland D, Kahn CR: Role of brain
in-vitro study of adipose androgen generation population-based European Prospective Inves- insulin receptor in control of body weight and
in polycystic ovary syndrome. Lancet 2015; tigation into Cancer and Nutrition (EPIC)- reproduction. Science 2000;289:2122–2125.
385(suppl 1):S16. Potsdam Study. Diabetes 2003;52:812–817. 62 Fauser BC, Tarlatzis BC, Rebar RW, Legro RS,
36 Lim SS, Davies MJ, Norman RJ, Moran LJ: 48 Ciaraldi TP, Carter L, Nikoulina S, Mudaliar Balen AH, Lobo R, Carmina E, Chang J, Yildiz
Overweight, obesity and central obesity in S, McClain DA, Henry RR: Glucosamine reg- BO, Laven JS, Boivin J, Petraglia F, Wijeyeratne
women with polycystic ovary syndrome: a ulation of glucose metabolism in cultured hu- CN, Norman RJ, Dunaif A, Franks S, Wild RA,
systematic review and meta-analysis. Hum man skeletal muscle cells: divergent effects on Dumesic D, Barnhart K: Consensus on wom-
Reprod Update 2012;18:618–637. glucose transport/phosphorylation and gly- en’s health aspects of polycystic ovary syn-
37 Hoeger KM: Obesity and lifestyle manage- cogen synthase in non-diabetic and type 2 di- drome (PCOS): the Amsterdam ESHRE/AS-
ment in polycystic ovary syndrome. Clin Ob- abetic subjects. Endocrinology 1999; 140: RM-Sponsored 3rd PCOS Consensus Work-
stet Gynecol 2007;50:277–294. 3971–380. shop Group. Fertil Steril 2012;97:28–38.e25.
38 Sinha R, Fisch G, Teague B, Tamborlane WV, 49 Previs SF, Withers DJ, Ren JM, White MF, 63 Dumesic DA, Oberfield SE, Stener-Victorin
Banyas B, Allen K, Savoye M, Rieger V, Tak- Shulman GI: Contrasting effects of IRS-1 ver- E, Marshall JC, Laven JS, Legro RS: Scientific
sali S, Barbetta G, Sherwin RS, Caprio S: Prev- sus IRS-2 gene disruption on carbohydrate statement on the diagnostic criteria, epidemi-
alence of impaired glucose tolerance among and lipid metabolism. J Biol Chem 2000;275: ology, pathophysiology, and molecular genet-
children and adolescents with marked obesi- 38990–38994. ics of polycystic ovary syndrome. Endocr Rev
ty. N Engl J Med 2002;346:802–810. 50 Cho H, Mu J, Kim JK, Thorvaldsen JL, Chu Q, 2015;36:487–525.
39 Hughan KS, Tfayli H, Warren-Ulanch JG, Ba- Crenshaw EB 3rd, Kaestner KH, Bartolomei 64 Rosenfield RL, Ehrmann DA: The pathogen-
rinas-Mitchell E, Arslanian SA: Early bio- MS, Shulman GI, Birnbaum MJ: Insulin resis- esis of polycystic ovary syndrome (PCOS): the
markers of subclinical atherosclerosis in tance and a diabetes mellitus-like syndrome hypothesis of PCOS as functional ovarian hy-
obese adolescent girls with polycystic ovary in mice lacking the protein kinase Akt2 perandrogenism revisited. Endocr Rev 2016;
syndrome. J Pediatr 2016;168:104–111. (PKBb). Science 2001;292:1728–1731. 37:467–520.
40 Puder JJ: Central fat excess in polycystic ovary 51 Carpentier AC: Postprandial fatty acid me- 65 Taylor AE, McCourt B, Martin KA, Anderson
syndrome: relation to low-grade inflamma- tabolism in the development of lipotoxicity EJ, Adams JM, Schoenfeld D, Hall JE: Deter-
tion and insulin resistance. J Clin Endocrinol and type 2 diabetes. Diabetes Metab 2008;34: minants of abnormal gonadotropin secretion
Metab 2005;90:6014–6021. 97–107. in clinically defined women with polycystic
41 Pasquali R, Casimirri F, Venturoli S, Antonio 52 Gambineri A, Pelusi C, Vicennati V, Pagotto ovary syndrome. J Clin Endocrinol Metab
M, Morselli L, Reho S, Pezzoli A, Paradisi R: U, Pasquali R: Obesity and the polycystic ova- 1997;82 2248–56.
Body fat distribution has weight-independent ry syndrome. Int J Obes Relat Metab Disord 66 Moenter SM: Leap of faith: does serum lutein-
effects on clinical, hormonal, and metabolic 2002;26:883–96. izing hormone always accurately reflect cen-
features of women with polycystic ovary syn- 53 Lord J, Wilkin T: Polycystic ovary syndrome tral reproductive neuroendocrine activity?
drome. Metabolism 1994;43:706–713. and fat distribution: the central issue? Hum Neuroendocrinology 2015;102:256–266.
42 Ojeda-Ojeda M, Murri M, Insenser M, Esco- Fertil (Cambr) 2002;5:67–71. 67 Thompson IR, Kaiser UB: GnRH pulse fre-
bar-Morreale HF: Mediators of low-grade 54 Ibáñez L, Ong KK, López-Bermejo A, Dunger quency-dependent differential regulation of
chronic inflammation in polycystic ovary DB, de Zegher F: Hyperinsulinaemic andro- LH and FSH gene expression. Mol Cell Endo-
syndrome (PCOS). Curr Pharm Des 2013;19: gen excess in adolescent girls. Nat Rev Endo- crinol 2014;385:28–35.
5775–5791. crinol 2014;10:499–508. 68 Moore AM, Campbell RE: The neuroendo-
43 Lambert EA, Teede H, Sari CI, Jona E, Shor- 55 Dhindsa G, Bhatia R, Dhindsa M, Bhatia V: crine genesis of polycystic ovary syndrome: a
akae S, Woodington K, Hemmes R, Eikelis N, Insulin resistance, insulin sensitization and role for arcuate nucleus GABA neurons. J Ste-
Straznicky NE, De Courten B, Dixon JB, inflammation in polycystic ovarian syndrome roid Biochem Mol Biol 2016;160:106–117.
Schlaich MP, Lambert GW: Sympathetic acti- inflammation in polycystic ovarian syndrome 69 Eagleson CA, Gingrich MB, Pastor CL,
vation and endothelial dysfunction in poly- inflammation in polycystic ovarian syn- Arora TK, Burt CM, Evans WS, Marshall JC:
cystic ovary syndrome are not explained by drome. J Postgrad Med 2004;50:140–144. Polycystic ovarian syndrome: evidence that
either obesity or insulin resistance. Clin En- 56 Adams J, Liu Z, Ren YA, Wun WS, Zhou W, flutamide restores sensitivity of the gonadotro-
docrinol (Oxf) 2015;83:812–819. Kenigsberg S, Librach C, Valdes C, Gibbons pin-releasing hormone pulse generator to in-
44 de Zegher F, López-Bermejo A, Ibáñez L: Ad- W, Richards J: Enhanced inflammatory tran- hibition by estradiol and progesterone. J Clin
ipose tissue expandability and the early ori- scriptome in the granulosa cells of women Endocrinol Metab 2000;85:4047–52.
gins of PCOS. Trends Endocrinol Metab with polycystic ovarian syndrome. J Clin En- 70 Pinilla L, Aguilar E, Dieguez C, Millar RP, Te-
2009;20:418–423. docrinol Metab 2016;101:3459–3468. na-Sempere M: Kisspeptins and reproduc-
45 de Zegher F, Reinher T, Malpique R, Daren- 57 Schmidt J, Weijdegard B, Mikkelsen AL, Lin- tion: physiological roles and regulatory mech-
deliler F, López-Bermejo A, Ibáñez L: Re- denberg S, Nilsson L, Brannstrom M: Differ- anisms. Physiol Rev 2012;92:1235–316.
duced prenatal weight gain and/or augment- ential expression of inflammation-related 71 Oakley AE, Clifton DK, Steiner RA: Kiss-
ed postnatal weight gain precede polycystic genes in the ovarian stroma and granulosa peptin signaling in the brain. Endocr Rev
ovary syndrome in adolescent girls. Obesity cells of PCOS women. Mol Hum Reprod 2009;30:713–43.
(Silver Spring) 2017;25:1486–1489. DOI: 2014;20:49–58. 72 Navarro VM, Tena-Sempere M: Neuroendo-
10.1002/oby.21935. 58 Jornayvaz FR, Shulman GI: Diacylglycerol ac- crine control by kisspeptins: role in metabolic
tivation of protein kinase Cε and hepatic in- regulation of fertility. Nat Rev Endocrinol
sulin resistance. Cell Metab 2012;15:574–584. 2012;8:40–53.
20 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
73 Lehman MN, Coolen LM, Goodman RL: 83 Cimino I, Casoni F, Liu X, Messina A, Parkash 93 Shi Y, Zhao H, Shi Y, Cao Y, Yang D, Li Z,
Minireview: kisspeptin/neurokinin B/dynor- J, Jamin SP, Catteau-Jonard S, Collier F, Ba- Zhang B, Liang X, Li T, Chen J, Shen J, Zhao
phin (KNDy) cells of the arcuate nucleus: a roncini M, Dewailly D, Pigny P, Prescott M, J, You L, Gao X, Zhu D, Zhao X, Yan Y, Qin
central node in the control of gonadotropin- Campbell R, Herbison AE, Prevot V, Giaco- Y, Li W, Yan J, Wang Q, Zhao J, Geng L, Ma
releasing hormone secretion. Endocrinology bini P: Novel role for anti-Mullerian hormone J, Zhao Y, He G, Zhang A, Zou S, Yang A, Liu
2010;151:3479–3489. in the regulation of GnRH neuron excitability J, Li W, Li B, Wan C, Qin Y, Shi J, Yang J, Jiang
74 Brown RE, Wilkinson DA, Imran SA, Caraty and hormone secretion. Nat Commun 2016; H, Xu JE, Qi X, Sun Y, Zhang Y, Hao C, Ju X,
A, Wilkinson M: Hypothalamic kiss1 mRNA 7:10055. Zhao D, Ren CE, Li X, Zhang W, Zhang Y,
and kisspeptin immunoreactivity are reduced 84 Moret M, Stettler R, Rodieux F, Gaillard RC, Zhang J, Wu D, Zhang C, He L, Chen ZJ: Ge-
in a rat model of polycystic ovary syndrome Waeber G, Wirthner D, Giusti V, Tappy L, nome-wide association study identifies eight
(PCOS). Brain Res 2012;1467:1–9. Pralong FP: Insulin modulation of luteinizing new risk loci for polycystic ovary syndrome.
75 Navarro VM, Sánchez-Garrido MA, Caste- hormone secretion in normal female volun- Nat Genet 2012;44:1020–1025.
llano JM, Roa J, García-Galiano D, Pineda R, teers and lean polycystic ovary syndrome pa- 94 Hayes MG, Urbanek M, Ehrmann DA, Arm-
Aguilar E, Pinilla L, Tena-Sempere M: Persis- tients. Neuroendocrinology 2009;89:131–139. strong LL, Lee JY, Sisk R, Karaderi T, Barber
tent impairment of hypothalamic KiSS-1 sys- 85 Patel K, Coffler MS, Dahan MH, Yoo RY, TM, McCarthy MI, Franks S, Lindgren CM,
tem after exposures to estrogenic compounds Lawson MA, Malcom PJ, Chang RJ: Increased Welt CK, Diamanti-Kandarakis E, Panidis D,
at critical periods of brain sex differentiation. luteinizing hormone secretion in women with Goodarzi MO, Azziz R, Zhang Y, James RG,
Endocrinology 2009;150:2359–2367. polycystic ovary syndrome is unaltered by Olivier M, Kissebah AH; Reproductive Medi-
76 Fraser GL, Hoveyda HR, Clarke IJ, Ramaswa- prolonged insulin infusion. J Clin Endocrinol cine Network, Stener-Victorin E, Legro RS,
my S, Plant TM, Rose C, Millar RP: The NK3 Metab 2003;88:5456–5461. Dunaif A: Genome-wide association of poly-
receptor antagonist ESN364 interrupts pulsa- 86 Divall SA, Williams TR, Carver SE, Koch L, cystic ovary syndrome implicates alterations
tile LH secretion and moderates levels of Brüning JC, Kahn CR, Wondisford F, Ra- in gonadotropin secretion in European ances-
ovarian hormones throughout the menstrual dovick S, Wolfe A: Divergent roles of growth try populations. Nat Commun 2015;18:7502.
cycle. Endocrinology 2015;156:4214–4225. factors in the GnRH regulation of puberty in 95 Day FR, Hinds DA, Tung JY, Stolk L, Styrkars-
77 George JT, Kakkar R, Marshall J, Scott ML, mice. J Clin Invest 2010;120:2900–2909. dottir U, Saxena R, Bjonnes A, Broer L, Dung-
Finkelman RD, Ho TW, Veldhuis J, Skorup- 87 Cernea M, Phillips R, Padmanabhan V, Cool- er DB, Halldorsson BV, Lawlor DA, Laval G,
skaite K, Anderson RA, McIntosh S, Webber en LM, Lehman MN: Prenatal testosterone Mathieson I, McCardle WL, Louwers Y,
L: Neurokinin B receptor antagonism in exposure decreases colocalization of insulin Meun C, Ring S, Scott RA, Sulem P, Uitterlin-
women with polycystic ovary syndrome: a receptors in kisspeptin/neurokinin B/dynor- den AG, Wareham NJ, Thorsteinsdottir U,
randomized, placebo-controlled trial. J Clin phin and agouti-related peptide neurons of Welt C, Stefansson K, Laven JS, Ong KK, Per-
Endocrinol Metab 2016;101:4313–4321. the adult ewe. Eur J Neurosci 2016; 44: 2557– ry JR: Causal mechanisms and balancing se-
78 Narayanaswamy S, Prague JK, Jayasena CN, 2568. lection inferred from genetic associations
Papadopoulou DA, Mizamtsidi M, Shah AJ, 88 Qiu X, Dao H, Wang M, Heston A, Garcia with polycystic ovary syndrome. Nat Com-
Bassett P, Comninos AN, Abbara A, Bloom KM, Sangal A, Dowling AR, Faulkner LD, mun 2015;6:8464.
SR, Veldhuis JD, Dhillo WS: Investigating the Molitor SC, Elias CF, Hill JW: Insulin and 96 Mbarek H, Steinberg S, Nyholt DR, Gordon
KNDy hypothesis in humans by coadminis- leptin signaling interact in the mouse Kiss1 SD, Miller MB, McRae AF, Hottenga JJ, Day
tration of kisspeptin, neurokinin B, and nal- neuron during the peripubertal period. PLoS FR, Willemsen G, de Geus EJ, Davies GE,
trexone in men. J Clin Endocrinol Metab One 2015;10:e0121974. Martin HC, Penninx BW, Jansen R, McAlo-
2016;101:3429–3436. 89 Evans MC, Rizwan M, Mayer C, Boehm U, ney K, Vink JM, Kaprio J, Plomin R, Spector
79 Ruiz-Pino F, Garcia-Galiano D, Manfredi- Anderson GM: Evidence that insulin signal- TD, Magnusson PK, Reversade B, Harris RA,
Lozano M, Leon S, Sánchez-Garrido MA, Roa ling in gonadotrophin-releasing hormone Aagaard K, Kristjansson RP, Olafsson I, Ey-
J, Pinilla L, Navarro VM, Tena-Sempere M: and kisspeptin neurones does not play an es- jolfsson GI, Sigurdardottir O, Iacono WG,
Effects and interactions of tachykinins and sential role in metabolic regulation of fertil- Lambalk CB, Montgomery GW, McGue M,
dynorphin on FSH and LH secretion in devel- ity in mice. J Neuroendocrinol 2014; 26: 468– Ong KK, Perry JR, Martin NG, Stefánsson H,
oping and adult rats. Endocrinology 2015; 479. Stefánsson K, Boomsma DI: Identification of
156:576–588. 90 Toulis KA, Goulis DG, Farmakiotis D, Geor- common genetic variants influencing spon-
80 García-Galiano D, Pineda R, Roa J, Ruiz-Pino gopoulos NA, Katsikis I, Tarlatzis BC, Papa- taneous dizygotic twinning and female fertil-
F, Sánchez-Garrido MA, Castellano JM, dimas I, Panidis D: Adiponectin levels in ity. Am J Hum Genet 2016; 98: 898–908.
Aguilar E, Navarro VM, Pinilla L, Tena-Sem- women with polycystic ovary syndrome: a 97 Mutharasan P, Galdones E, Peñalver Bernabé
pere M: Differential modulation of gonado- systematic review and a meta-analysis. Hum B, Garcia OA, Jafari N, Shea LD, Woodruff
tropin responses to kisspeptin by aminoaci- Reprod Update 2009;15:297–307. TK, Legro RS, Dunaif A, Urbanek M: Evi-
dergic, peptidergic, and nitric oxide neuro- 91 Yuan X, Hu T, Zhao H, Huang Y, Ye R, Lin J, dence for chromosome 2p16.3 polycystic ova-
transmission. Am J Physiol Endocrinol Metab Zhang C, Zhang H, Wei G, Zhou H, Dong M, ry syndrome susceptibility locus in affected
2012;303:E1252–E1263. Zhao J, Wang H, Liu Q, Lee HJ, Jin W, Chen women of European ancestry. J Clin Endocri-
81 Moore AM, Prescott M, Marshall CJ, Yip SH, ZJ: Brown adipose tissue transplantation nol Metab 2013;98:E185–E190.
Campbell RE: Enhancement of a robust arcu- ameliorates polycystic ovary syndrome. Proc 98 Zhu JQ, Zhu L, Liang XW, Xing FQ, Schatten
ate GABAergic input to gonadotropin-releas- Natl Acad Sci USA 2016;113:2708–2713. H, Sun QY: Demethylation of LHR in dehy-
ing hormone neurons in a model of polycystic 92 Chen ZJ, Zhao H, He L, Shi Y, Qin Y, Shi Y, droepiandrosterone-induced mouse model of
ovarian syndrome. Proc Natl Acad Sci USA Li Z, You L, Zhao J, Liu J, Liang X, Zhao X, polycystic ovary syndrome. Mol Hum Reprod
2015;112:596–601. Zhao J, Sun Y, Zhang B, Jiang H, Zhao D, Bian 2010;16:260–266.
82 Herbison AE, Moenter SM: Depolarising and Y, Gao X, Geng L, Li Y, Zhu D, Sun X, Xu JE, 99 Wang P, Zhao H, Li T, Zhang W, Wu K, Li M,
hyperpolarising actions of GABA(A) receptor Hao C, Ren CE, Zhang Y, Chen S, Zhang W, Bian Y, Liu H, Ning Y, Li G, Chen ZJ: Hypo-
activation on gonadotrophin-releasing hor- Yang A, Yan J, Li Y, Ma J, Zhao Y: Genome- methylation of the LH/choriogonadotropin
mone neurones: towards an emerging con- wide association study identifies susceptibili- receptor promoter region is a potential mech-
sensus. J Neuroendocrinol 2011;23:557–569. ty loci for polycystic ovary syndrome on chro- anism underlying susceptibility to polycystic
mosome 2p16.3, 2p21 and 9q33.3. Nat Genet ovary syndrome. Endocrinology 2014; 155:
2011;43:55–59. 1445–1452.
Update: PCOS Pathophysiology, Horm Res Paediatr 21
Diagnosis, and Treatment DOI: 10.1159/000479371
100 Zhang Y, Fatima N, Dufau ML: Coordinated cose metabolism in polycystic ovarian syn- R, Gomez-Lobo V, Joel D, Tfayli H, Arsla-
changes in DNA methylation and histone drome. Endocrine 2016;53:280–90. nian S, Dabadghao P, Garcia Rudaz C, Lee
modifications regulate silencing/derepression 112 Wu HL, Heneidi S, Chuang TY, Diaond MP, PA: The diagnosis of polycystic ovary syn-
of luteinizing hormone receptor gene tran- Layman LC, Azziz R, Chen YH: The expres- drome during adolescence. Horm Res Pae-
scription. Mol Cell Biol 2005;25:7929–7939. sion of the miR-25/93/106b family of micro- diatr 2015;83:376–389.
101 Yu YY, Sun CX, Liu YK, Li Y, Wang L, RNAs in the adipose tissue of women with 125 Carmina E, Oberfield SE, Lobo R: The diag-
Zhang W: Promoter methylation of CY- polycystic ovary syndrome. J Clin Endocri- nosis of polycystic in adolescents. Am J Ob-
P19A1 gene in Chinese polycystic ovary syn- nol Metab 2014;99:E2754–E2761. stet Gynecol 2010;203:201.e1–e5.
drome patients. Gynecol Obstet Invest 2013; 113 Song J, Luo S, Li SW: miRNA-592 is down- 126 Di Fede G, Mansueto P, Pepe G, Rini B, Car-
76:209–213. regulated and may target LHCGR in poly- mina E: High prevalence of polycystic ovary
102 Sang Q, Li X, Wang H, Wang H, Zhang S, Xu cystic ovary syndrome patients. Reprod Biol syndrome in women with mild hirsutism
N, Kwon S, Abbott DH, Geller DH, Dumesic 2015;15:229–237. and no other significant clinical symptoms.
DA, Azziz R, Guo X, Goodarzi MO: Quanti- 114 Lansdown A, Rees DA: The sympathetic Fertil Steril 2010;94:194–197.
tative methylation level of the EPHX1 pro- nervous system in polycystic ovary syn- 127 Reinehr T, Bosse C, Lass N, Rothermel J,
moter in peripheral blood DNA Is associated drome: a novel therapeutic target? Clin En- Knop C, Roth CL: Effect of weight loss on
with polycystic ovary syndrome. PLoS One docrinol (Oxford) 2012;77:791–801. puberty onset in overweight children. J Pe-
2014;9:e88013. 115 Rahmouni K, Morgan DA, Morgan GM, Liu diatr 2017;184:143–50.
103 Qu F, Wang FF, Yin R, Ding GL, El-Prince X, Sigmund CD, Mark AL, Haynes WG: Hy- 128 Reinehr T, Kulle A, Rothermel J, Knop-
M, Gao Q, Shi BW, Pan HH, Huang YT, Jin pothalamic PI3K and MAPK differentially Schmenn C, Lass N, Bosse C, Holtherus PM:
M, Leung PC, Sheng JZ, Huang HF: A mo- mediate regional sympathetic activation to Longitudinal analyses of the steroid metabo-
lecular mechanism underlying ovarian dys- insulin. J Clin Invest 2004;114:652–658. lome in obese girls with weight loss. Endocr
function of polycystic ovary syndrome: hy- 116 Rahmouni K, Morgan DA, Morgan GM, Liu Connect 2017;6:213–224.
perandrogenism induces epigenetic altera- X, Sigmund CD, Mark AL, Haynes WG: Ab- 129 Zawadzki J, Dunaif A: Diagnostic criteria for
tions in the granulosa cells. J Mol Med 2012; normal heart rate recovery after maximal polycystic ovary syndrome: towards a ratio-
90:911–923. cardiopulmonary exercise stress testing in nal approach; in Dunaif A, Givens JR, Hasel-
104 Wang XX, Wei JZ, Jiao J, Jiang SY, Yu DH, young overweight women with polycystic tine FP, Merriam GR (eds): Polycystic Ovary
Li D: Genome-wide DNA methylation and ovary syndrome. Clin Endocrinol (Oxford) Syndrome. Boston, Blackwell Scientific Pub-
gene expression patterns provide insight 2008;68:88–93. lications, 1992, vol 4, pp 377–384.
into polycystic ovary syndrome develop- 117 Tekin G, Tekin A, Kiliçarslan EB, Hay- 130 Rotterdam ESHRE/ASRM-Sponsored PCOS
ment. Oncotarget 2014;5:6603–6610. dardedeoğlu B, Katircibaşi T, Koçum T, Erol Consensus Workshop Group: Revised 2003
105 Yu YY, Sun CX, Liu YK, Li Y, Wang L, Zhang T, Cölkesen Y, Sezgin AT, Müderrisoğlu H: consensus on diagnostic criteria and long-
W: Genome-wide screen of ovary-specific Altered autonomic neural control of the car- term health risks related to polycystic ovary
DNA methylation in polycystic ovary syn- diovascular system in patients with polycystic syndrome. Fertil Steril 2004;81:19–25.
drome. Fertil Steril 2015;104:145–153.e6. ovary syndrome. Int J Cardiol 2008;130:49–55. 131 Yildiz BO, Bolour S, Woods K, Moore A,
106 Shen HR, Qiu LH, Zhang ZQ, Qin YY, Cao 118 Yildirir A, Aybar F, Kabakci G, Yarali H, Oto Azziz R: Visually scoring hirsutism. Hum
C, Di W: Genome-wide methylated DNA A: Heart rate variability in young women Reprod Update 2010;16:51–64.
immunoprecipitation analysis of patients with polycystic ovary syndrome. Ann Non- 132 Azziz R, Carmina E, Dewailly D, Diamanti-
with polycystic ovary syndrome. PLoS One invasive Electrocardiol 2006;11:306–312. Kandarakis E, Escobar-Morreale HF, Fut-
2013;8:e64801. 119 Sverrisdottir YB, Mogren T, Kataoka J, Janson terweit W, Janssen OE, Legro RS, Norman
107 Li S, Zhu D, Duan H, Ren A, Glintborg D, PO, Stener-Victorin E: Is polycystic ovary RJ, Taylor AE, Witchel SF; Task Force on the
Andersen M, Skov V, Thomassen M, Kruse syndrome associated with high sympathetic Phenotype of the Polycystic Ovary Syn-
T, Tan: Differential DNA methylation pat- nerveactivity and size at birth? Am J Physiol drome of The Androgen Excess and PCOS
terns of polycystic ovarian syndrome in Endocrinol Metab 2008;294:E576–E581. Society: The Androgen Excess and PCOS
whole blood of Chinese women. Oncotarget 120 Heider U, Pedal I, Spanel-Borowski K: In- Society criteria for the polycystic ovary syn-
2017;8:20656–20666. crease in nerve fibers and loss of mast cells drome: the complete task force report. Fertil
108 Kokosar M, Benrick A, Perfilyev A, Fornes in polycystic and postmenopausal ovaries. Steril 2009;91:456–488.
R, Nilsson E, Maliqueo M, Behre CJ, Sazon- Fertil Steril 2001;75:1141–1147. 133 Johnson T, Kaplan L, Ouyang P, Rizza R:
ova, A, Ohlsson C, Ling C, Stener-Victorin 121 Lara HE, Ferruz JL, Luza S, Bustamante DA, National Institutes of Health evidence-based
E: Epigenetic and transcriptional alterations Borges Y, Ojeda SR: Activation of ovarian methodology workshop on polycystic ovary
in human adipose tissue of polycystic ovary sympathetic nerves in polycystic ovary syn- syndrome (PCOS). NIH EbMW Report.
syndrome. Sci Rep 2016;6:22883. drome. Endocrinology 1993;133:2690–2695. Bethesda, National Institutes of Health,
109 Xu N, Kwon S, Abbott DH, Geller DH, Du- 122 Lara HE, Dissen GA, Leyton V, Paredes A, 2012, vol 1, pp 1–14.
mesic DA, Azziz R, Guo X, Goodarzi MO: Fuenzalida H, Fiedler JL, Ojeda SR: An in- 134 Legro RS, Arslanian SA, Ehrmann DA,
Epigenetic mechanism underlying the de- creased intraovarian synthesis of nerve Hoeger KM, Murad MH, Pasquali R, Welt
velopment of polycystic ovary syndrome growth factor and its low affinity receptor is CK; Endocrine Society: Diagnosis and treat-
(PCOS)-like phenotypes in prenatally an- a principal component of steroid-induced ment of polycystic ovary syndrome: an En-
drogenized rhesus monkeys. PLoS One polycystic ovary in the rat. Endocrinology docrine Society clinical practice guideline. J
2011;6:e27286. 2000;141:1059–1072. Clin Endocrinol Metab 2013;98:4565–4592.
110 Li S, Zhu D, Duan H, Tan Q: The epigenom- 123 Dissen GA, Garcia-Rudaz C, Paredes A, 135 Azziz R, Carmina E, Dewailly D, Diamanti-
ics of polycystic ovarian syndrome: from Mayer C, Mayerhofer A, Ojeda SR: Excessive Kandarakis E, Escobar-Morreale HF, Fut-
pathogenesis to clinical manifestations. Gy- ovarian production of nerve growth factor terweit W, Janssen OE, Legro RS, Norman
necol Endocrinol 2016;32:942–946. facilitates development of cystic ovarian RJ, Taylor AE, Witchel SF; Androgen Excess
111 Jiang L, Huang J, Chen Y, Yang Y, Li R, Li Y, morphology in mice and is a feature of poly- Society: Position statement: criteria for de-
Chen X, Yang D: Identification of several cystic ovarian syndrome in humans. Endo- fining polycystic ovary syndrome as a pre-
circulating microRNAs from a genome- crinology 2009;150:2906–2914. dominantly hyperandrogenic syndrome: an
wide circulating microRNA expression pro- 124 Witchel SF, Oberfield S, Rosenfield RL, Cod- Androgen Excess Society guideline. J Clin
file as potential biomarkers for impaired glu- ner E, Bonny A, Ibáñez L, Pena A, Horikawa Endocrinol Metab 2006;91:4237–4245.
22 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
136 Plouffe L Jr: Disorders of excessive hair berty: evidence for marked hyperandrogen- cusing on natural history and circulating
growth in the adolescent. Obstet Gynecol emia in pre- and early pubertal obese girls. J hormones. Fertil Steril 1992;57:505–513.
Clin North Am 2000;27:79–99. Clin Endocrinol Metab 2007;92:430–436. 165 Escobar-Morreale HF, Carmina E, Dewailly
137 Engmann L, Jin S, Sun F, Legro RS, Polotsky 152 Carmina E, Dewailly D, Escobar-Morreale D, Gambineri A, Kelestimur F, Moghetti P,
AJ, Hansen KR, Coutifaris C, Diamond MP, HF, Kelestimur F, Moran C, Oberfield S, Pugeat M, Qiao J, Wijeyaratne CN, Witchel
Eisenberg E, Zhang H, Santoro N; Repro- Witchel SF, Azziz R: Non-classic congenital SF, Norman RJ: Epidemiology, diagnosis
ductive Medicine Network: Racial and eth- adrenal hyperplasia due to 21-hydroxylase and management of hirsutism: a consensus
nic differences in the polycystic ovary syn- deficiency revisited: an update with a special statement by the Androgen Excess and Poly-
drome (PCOS) metabolic phenotype. Am J focus on adolescent and adult women. Hum cystic Ovary Syndrome Society. Hum Re-
Obstet Gynecol 2017;216:493.e1–e13. Reprod Update 2017;5:1–20. prod Update 2012;18:146–170.
138 Yıldız BO, Bolour S, Woods K, Moore A, 153 Metcalf MG, Skidmore DS, Lowry GF, 166 Rosner W, Vesper H: Toward excellence in
Azziz R: Visually scoring hirsutism. Hum Mackenzie JA: Incidence of ovulation in the testosterone testing: a consensus statement. J
Reprod Update 2010;16:51–64. years after the menarche. J Endocrinol 1983; Clin Endocrinol Metab 2010;95:4542–4548.
139 Li R, Qiao J, Yang D, Li S, Lu S, Wu X, Wei 97:213–219. 167 Legro RS, Schlaff WD, Diamond MP, Couti-
Z: Epidemiology of hirsutism among wom- 154 Apter D: Endocrine and metabolic abnormal- faris C, Casson PR, Brzyski RG, Christman
en of reproductive age in the community: a ities in adolescents with a PCOS-like condi- GM, Trussell JC, Krawetz SA, Snyder PJ, Ohl
simplified scoring system. Eur J Obstet Gy- tion: consequences for adult reproduction. D, Carson SA, Steinkampf MP, Carr BR,
necol Reprod Biol 2012;163:165–169. Trends Endocrinol Metab 1998;9:58–61. McGovern PG, Cataldo NA, Gosman GG,
140 Martin KA, Chang RJ, Ehrmann DA, Ibanez 155 Hickey M, Doherty DA, Atkinson H, Slobo- Nestler JE, Myers ER, Santoro N, Eisenberg
L, Lobo RA, Rosenfield RL, Shapiro J, Mon- da DM, Franks S, Norman RJ, Hart R: Clini- E, Zhang M, Zhang H; Reproductive Medi-
tori VM, Swiglo BA: Evaluation and treatment cal, ultrasound and biochemical features of cine Network: Total testosterone assays in
of hirsutism in premenopausal women: an en- polycystic ovary syndrome in adolescents: women with polycystic ovary syndrome:
docrine society clinical practice guideline. J implications for diagnosis. Hum Reprod precision and correlation with hirsutism. J
Clin Endocrinol Metab 2008;98:1105–1120. 2011;26:1469–1477. Clin Endocrinol Metab 2010;95:5305–5313.
141 Souter I, Sanchez A, Perez M, Bartolucci A, 156 Diaz A, Laufer MR, Breech LL: Menstrua- 168 Auchus RJ: Steroid assays and endocrinolo-
Azziz R: The prevalence of androgen excess tion in girls and adolescents: using the men- gy. Best practices for basic scientists. Endo-
among patients with minimal unwanted strual cycle as a vital sign. Pediatrics 2006; crinology 2014;155:2049–2051.
hair growth. Am J Obstet Gynecol 2004;191: 118:2245–2250. 169 Gambineri A, Fanelli F, Prontera O, Repaci A,
1914–1920. 157 World Health Organization multicenter Di Dalmazi G, Zanotti L, Pagotto U, Flacco
142 Hawryluk EB, English JC 3rd: Female ado- study on menstrual and ovulatory patterns ME, Guidi J, Fava GA, Manzoli L, Pasquali R:
lescent hair disorders. J Pediatr Adolesc Gy- in adolescent girls. I. A multicenter cross- Prevalence of hyperandrogenic states in late
necol 2009;22:271–281. sectional study of menarche. World Health adolescent and young women: epidemiologi-
143 Ferriman D, Gallwey JD: Clinical assess- Organization Task Force on Adolescent Re- cal survey on Italian high-school students. J
ment of body hair growth in women. J Clin productive Health. J Adolesc Health Care Clin Endocrinol Metab 2013;98:1641–1650.
Endocrinol Metab. 1961;21:1440–1447. 1986;7:229–235. 170 Codner E, Villarroel C, Eyzaguirre FC,
144 Dilutunmbi Y, Paley K, English JC: Adoles- 158 Southam AL, Richart RM: The prognosis for López P, Merino PM, Pérez-Bravo F, Iñiguez
cent female acne: etiology and management. adolescents with menstrual abnormalities. G, Cassorla F: Polycystic ovarian morphol-
J Pediatr Adolesc Gynecol 2008;21:171–176. Am J Obstet Gynecol 1966;94:637–645. ogy in postmenarchal adolescents. Fertil
145 Chang RJ, Coffler MS: Polycystic ovary syn- 159 Franks S: Adult polycystic ovary syndrome Steril 2011;95:702–6.e1–e2.
drome: early detection in the adolescent. begins in childhood. Best Pract Res Clin En- 171 Murphy MK, Hall JE, Adams JM, Lee H,
Clin Obstet Gynecol 2007;50:178–187. docrinol Metab 2002;16:263–272. Welt CK: Polycystic ovarian morphology in
146 Chen WC, Zouboulis CC: Hormones and 160 van Hooff MH, Voorhorst FJ, Kaptein MB, normal women does not predict the devel-
the pilosebaceous unit. Dermatoendocrinol Hirasing RA, Koppenaal C, Schoemaker J: opment of polycystic ovary syndrome. J Clin
2009;1:81–86. Predictive value of menstrual cycle pattern, Endocrinol Metab 2006;91:3878–3884.
147 Lucky AW, Biro FM, Simbartl LA, Morrison body mass index, hormone levels and poly- 172 Venturoli S, Porcu E, Fabbri R, Pluchinotta
JA, Sorg NW: Predictors of severity of acne cystic ovaries at age 15 years for oligo-amen- V, Ruggeri S, Macrelli S, Paradisi R, Flami-
vulgaris in young adolescent girls: results of errohea at age 18 years. Hum Reprod 2004; gni C: Longitudinal change of sonographic
a five-year longitudinal study. J Pediatr 19:383–392. ovarian aspects and endocrine parameters in
1997;130:30–39. 161 Wiksten-Almströmer M, Hirschberg AL, irregular cycles of adolescence. Pediatr Res
148 Merino PM, Codner E, Cassorla F: A ratio- Hagenfeldt K: Prospective follow-up of 1995;38:974–980.
nal approach to the diagnosis of polycystic menstrual disorders in adolescence and 173 Dewailey D: Diagnostic criteria for PCOS: is
ovarian syndrome during adolescence. Arq prognostic factors. Acta Obstet Gynecol there a need for a rethink? Best Pract Res
Bras Endocrinol Metabol 2011;55:590–598. Scand 2008;87:1162–1168. Clin Obstet Gynaecol 2016:37:5–11.
149 Ibañez L, Potau N, Virdis R, Zampolli M, 162 Rosenfield RL, Ehrmann DA, Littlejohn EE: 174 Holm K, Laursen EM, Brocks V, Muller J:
Terzi C, Gussinyé M, Carrascosa A, Vicens- Adolescent polycystic ovary syndrome due Pubertal maturation of the internal genita-
Calvet E: Postpubertal outcome in girls diag- to functional ovarian hyperandrogenism lia: an ultrasound evaluation of 166. Ultra-
nosed of premature pubarche during child- persists into adulthood. J Clin Endocrinol sound Obstet Gynecol 1995;6:175–181.
hood: increased frequency of functional Metab 2015;100:1537–1543. 175 Kelsey TW, Dodwell SK, Wilkinson AG,
ovarian hyperandrogenism. J Clin Endocri- 163 Carroll J, Saxena R, Welt CK: Environmental Greve T, Andersen CY, Anderson RA, Wal-
nol Metab 1993;76:1599–1603. and genetic factors influence age at menarche lace WH: Ovarian volume throughout life: a
150 Witchel SF: Puberty and polycystic ovary in women with polycystic ovary syndrome. J validated normative model. PLoS One 2013;
syndrome. Mol Cell Endocrinol 2006; 254– Pediatr Endocrinol Metab 2012;25:459–466. 8:e71465.
255:146–153. 164 Dahlgren E, Johansson S, Lindstedt G, 176 Bentzen JG, Forman JL, Johannsen TH, Pin-
151 McCartney CR, Blank SK, Prendergast KA, Knutsson F, Odén A, Janson PO, Mattson borg A, Larsen EC, Andersen AN: Ovarian
Chhabra S, Eagleson CA, Helm KD, Yoo R, LA, Crona N, Lundberg PA: Women with antral follicle subclasses and anti-mullerian
Chang RJ, Foster CM, Caprio S, Marshall JC: polycystic ovary syndrome wedge resected hormone during normal reproductive aging.
Obesity and sex steroid changes across pu- in 1956 to 1965: a long-term follow-up fo- J Clin Endocrinol Metab 2013;98:1602–1611.
Update: PCOS Pathophysiology, Horm Res Paediatr 23
Diagnosis, and Treatment DOI: 10.1159/000479371
177 Mortensen M, Rosenfield RL, Littlejohn E: adolescents. Gynecol Endocrinol 2015; 31: rived from oral glucose tolerance test. Acta
Functional significance of polycystic-size 625–629. Diabetol 2012;49:S195–S204.
ovaries in healthy adolescents. J Clin Endo- 189 Lie Fong S, Visser JA, Welt CK, de Rijke YB, 201 Matsuda M, DeFronzo R: Insulin sensitivity
crinol Metab 2006;91:3786–3790. Eijkemans MJ, Broekmans FJ, Roes EM, Pe- indices obtained from oral glucose tolerance
178 Villarroel C, Merino PM, López P, Eyza- ters WH, Hokken-Koelega AC, Fauser BC, test: comparison with the euglycemic insulin
guirre FC, Van Velzen A, Iñiguez G, Codner Themmen AP, de Jong FH, Schipper I, clamp. Diabetes Care 1999;22:1462–1470.
E: Polycystic ovarian morphology in adoles- Laven JS: Serum anti-mullerian hormone 202 Hoeger K, Davidson K, Kochman L, Cherry
cents with regular menstrual cycles is associ- levels in healthy females: a nomogram rang- T, Kopin L, Guzick DS: The impact of met-
ated with elevated anti-Mullerian hormone. ing from infancy to adulthood. J Clin Endo- formin, oral contraceptives, and lifestyle
Hum Reprod 2011;26:2861–2868. crinol Metab 2012;97:4650–4655. modification on polycystic ovary syndrome
179 Dewailly D, Lujan ME, Carmina E, Cedars 190 Kelsey TW, Wright P, Nelson SM, Anderson in obese adolescent women in two random-
MI, Laven J, Norman RJ, Escobar-Morreale RA, Wallace WH: A validated model of se- ized, placebo-controlled clinical trials. J Clin
HF: Definition and significance of polycystic rum anti-mullerian hormone from concep- Endocrinol Metab 2008;93:4299–4306.
ovarian morphology: a task force report tion to menopause. PLoS One 2011;6:e22024. 203 Ornstein RM, Copperman NM, Jacobson MS:
from the Androgen Excess and Polycystic 191 Sopher AB, Grigoriev G, Laura D, Cameo T, Effect of weight loss on menstrual function in
Ovary Syndrome Society. Hum Reprod Up- Lerner JP, Chang RJ, McMahon DJ, Ober- adolescents with polycystic ovary syndrome. J
date 2014;20:334–352. field SE: Anti-Mullerian hormone may be a Pediatr Adolesc Gynecol 2011;24:161–165.
180 Rosenfield RL: The polycystic ovary mor- useful adjunct in the diagnosis of polycystic 204 Lass N, Kleber M, Winkel K, Wunsch R,
phology-polycystic ovary syndrome spec- ovary syndrome in nonobese adolescents. J Reinehr T: Effect of lifestyle intervention on
trum. J Pediatr Adolesc Gynecol 2014; 28: Pediatr Endocrinol Metab 2014; 27: 1175– features of polycystic ovarian syndrome,
412–419. 1179. metabolic syndrome, and intima-media
181 van Hooff MH, Voorhorst FJ, Kaptein MB, 192 Munzker J, Hofer D, Trummer C, Ulbing M, thickness in obese adolescent girls. J Clin
Hirasing RA, Koppenaal C, Schoemaker J: Harger A, Pieber T, Owen L, Keevil B, Bra- Endocrinol Metab 2011;96:3533–3540.
Polycystic ovaries in adolescents and the re- bant G, Lerchbaum E, Obermayer-Pietsch B: 205 Knop C, Singer V, Uysal Y, Schaefer A,
lationship with menstrual cycle patterns, lu- Testosterone to dihydrotestosterone ratio as Wolters B, Reinehr T: Extremely obese chil-
teinizing hormone, androgens, and insulin. a new biomarker for an adverse metabolic dren respond better than extremely obese
Fertil Steril 2000;74:49–58. phenotype in the polycystic ovary syn- adolescents to lifestyle interventions. Pediatr
182 Venturoli S, Porcu E, Fabbri R, Magrini O, drome. J Clin Endocrinol Metab 2015; 100: Obes 2015;10:7–14.
Gammi L, Paradisi R, Flamigni R: Longitu- 653–660. 206 Reinehr T, Lass N, Toschke C, Rothermel J,
dinal evaluation of the different gonadotro- 193 Sarray S, Almawi WY: Levels of CD40L and Lanzinger S, Holl RW: Which amount of
pin pulsatile patterns in anovulatory cycles other inflammatory biomarkers in obese BMI-SDS reduction Is necessary to improve
of young girls. J Clin Endocrinol Metab and non-obese women with polycystic ovary cardiovascular risk factors in overweight
1992;74:836–841. syndrome. Am J Reprod Immunol 2016; 76: children? J Clin Endocrinol Metab 2016;101:
183 Mortensen M, Ehrmann DA, Littlejohn E, 285–291. 3171–3179.
Rosenfield RL: Asymptomatic volunteers 194 Li Li, Zhang J, Deng Q, Li J, Li Z, Xiao Y, Hu 207 Harrison CL, Lombard CB, Moran LJ, Teede
with a polycystic ovary are a functionally dis- S, Li T, Tan Q, Li X, Luo B, Mo H: Proteomic HJ: Exercise therapy in polycystic ovary syn-
tinct but heterogeneous population. J Clin profiling for identification of novel bio- drome: a systematic review. Hum Reprod
Endocrinol Metab 2009;94:1579–1586. markers differentially expressed in human Update 2011;17:171–183.
184 Pigny P, Merlen E, Robert Y, Cortet-Rudelli ovaries from polycystic ovary syndrome pa- 208 Oude Luttikhuis H, Baur L, Jansen H,
C, Decanter C, Jonard S, Dewailly D: Elevat- tients. PLoS One 2016;11:e0164538. Shrewsbury VA, O'Malley C, Stolk RP, Sum-
ed serum level of anti-mullerian hormone in 195 Sorensen AE, Udesen PB, Wissing ML, En- merbell CD: Interventions for treating obe-
patients with polycystic ovary syndrome: re- glund AM, Dalgaard LT: MicroRNAs relat- sity in children. Cochrane Database Syst Rev
lationship to the ovarian follicle excess and ed to androgen metabolism and polycystic 2009;1:CD001872.
to the follicular arrest. J Clin Endocrinol ovary syndrome. Chem Biol Interact 2016; 209 Moran LJ, Ko H, Misso M, Marsh K, Noakes
Metab 2003;88:5957–5962. 259:8–16. M, Talbot M, Frearson M, Thondan M, Stepto
185 Pigny P, Jonard S, Robert Y, Dewailly D: Se- 196 Harris MI, Hadden WC, Knowler WC, Ben- N, Teede HJ: Dietary composition in the treat-
rum anti-Mullerian hormone as a surrogate nett PH: Prevalence of diabetes and im- ment of polycystic ovary syndrome: a system-
for antral follicle count for definition of the paired glucose tolerance and plasma glucose atic review to inform evidence-based guide-
polycystic ovary syndrome. J Clin Endocri- levels in U.S. population aged 20–74 yr. Dia- lines. J Acad Nutr Diet 2013;113:520–545.
nol Metab 2006;91:941–945. betes 1987;36:523–34. 210 Reinehr T: Lifestyle intervention in child-
186 Hart R, Doherty DA, Norman RJ, Franks S, 197 Matsuda M: Measuring and estimating insu- hood obesity: changes and challenges. Nat
Dickinson JE, Hickey M, Sloboda DM: Se- lin resistance in clinical and research set- Rev Endocrinol 2013;9:607–614.
rum antimullerian hormone (AMH) levels tings. Nutr Metab Cardiovasc Dis 2010; 20: 211 Haedersdal M, Gotzsche PC: Laser and pho-
are elevated in adolescent girls with polycys- 79–86. toepilation for unwanted hair growth. Co-
tic ovaries and the polycystic ovarian syn- 198 Burgert TS, Vuguin PM, DiMartino-Nardi J, chrane Database Syst Rev 2006;4:CD004684.
drome (PCOS). Fertil Steril 2010; 94: 1118– Attie KM, Saenger P: Assessing insulin resis- 212 Haedersdal M, Wulf HC: Evidence-based
1121. tance: application of a fasting glucose to in- review of hair removal using lasers and light
187 Rosenfield RL, Wroblewski K, Padmanab- sulin ratio in growth hormone-treated chil- sources. J Eur Acad Dermatol Venereol
han V, Littlejohn E, Mortensen M, Ehrmann dren. Horm Res 2002;57:37–42. 2006;20:9–20.
DA: Antimullerian hormone levels are in- 199 Jean AM, Hassoun A, Hughes J, Pomeranz 213 Sadighha A, Mohaghegh Zahed G: Meta-
dependently related to ovarian hyperan- C, Fennoy I, McMahon DJ, Oberfield SE: analysis of hair removal laser trials. Lasers
drogenism and polycystic ovaries. Fertil Utility of insulin response and proinsulin to Med Sci 2009;24:21–25.
Steril 2012;98:242–249. assess insulin resistance. J Pediatr 2009;155: 214 Clayton WJ, Lipton M, Elford J, Rustin M,
188 Villarroel C, Lopez P, Merino PM, Iniguez 893–899. Sherr L: A randomized controlled trial of la-
G, Sir-Petermann T, Codner E: Hirsutism 200 Nagasaka S, Kusaka I, Yamashita K, Funase ser treatment among hirsute women with
and oligomenorrhea are appropriate screen- Y, Yamauchi K, Katakura M, Ishibashi S, polycystic ovary syndrome. Br J Dermatol
ing criteria for polycystic ovary syndrome in Aizawa T: Index of glucose effectiveness de- 2005;152:986–992.
24 Horm Res Paediatr Ibáñez et al.
DOI: 10.1159/000479371
215 McGill DJ, Hutchison C, McKenzie E, Mc- ism. J Clin Endocrinol Metab 2001;86:3595– cystic ovary syndrome and cardiovascular
Sherry E, Mackay IR: A randomized, split- 3598. risk in young patients treated with drospire-
face comparison of facial hair removal with 227 Al Khalifah RA, Florez ID, Dennis B, Tha- none-ethinylestradiol or contraceptive vagi-
the alexandrite laser and intense pulsed light bane L, Bassilious E: Metformin or oral con- nal ring. A prospective, randomized, pilot
system. Lasers Surg Med 2007;39:767–772. traceptives for adolescents with polycystic study. Fertil Steril 2010;94:1417–1425.
216 Somani N, Turvy D: Hirsutism: an evidence- ovarian syndrome: a meta-analysis. Pediat- 238 Bhattacharya SM, Jha A: Comparative study
based treatment update. Am J Clin Dermatol rics 2016;137:e20154089. of the therapeutic effects of oral contracep-
2014;15:247–266. 228 Swiglo BA, Cosma M, Flynn DN, Kurtz DM, tive pills containing desogestrel, cyproter-
217 Vissing AC, Taudorf EH, Haak CS, Philip- Labella ML, Mullan RJ, Erwin PJ, Montori one acetate, and drospirenone in patients
sen PA, Hædersdal M: Adjuvant eflorni- VM: Clinical review: Antiandrogens for the with polycystic ovary syndrome. Fertil Steril
thine to maintain IPL-induced hair reduc- treatment of hirsutism: a systematic review 2012;98:1053–1059.
tion in women with facial hirsutism: a ran- and meta-analyses of randomized con- 239 Ibáñez L, del Río L, Díaz M, Sebastiani G,
domized controlled trial. J Eur Acad trolled trials. J Clin Endocrinol Metab 2008; Pozo OJ, López-Bermejo A, de Zegher F:
Dermatol Venereol 2016;30:314–319. 93:1153–1160. Normalizing ovulation rate by preferential
218 Wang T, McNeill AM, Chen Y, Senderak M, 229 Moghetti P, Tosi F, Tosti A, Negri C, Miscia- reduction of hepato-visceral fat in adoles-
Shankar RR: Metformin prescription pat- li C, Perrone F, Caputo M, Muggeo M, Cas- cent girls with polycystic ovary syndrome.
terns among US adolescents aged 10–19 tello R: Comparison of spironolactone, flu- J Adolesc Health 2017, DOI: 10.1016/j.
years: 2009–2013. J Clin Pharm Ther 2016; tamide, and finasteride efficacy in the treat- jadohealth.2017.04.010.
41:229–236. ment of hirsutism: a randomized, double 240 Ibáñez L, de Zegher F, Potau N: Anovulation
219 Naderpoor N, Shorakae S, de Courden B, blind, placebo-controlled trial. J Clin Endo- after precocious pubarche: early markers
Misso ML, Moran LJ, Teede HJ: Metformin crinol Metab 2000;85:89–94. and time course in adolescence. J Clin Endo-
and lifestyle modification in polycystic ovary 230 de Zegher F, Ibáñez L: Low-dose flutamide crinol Metab 1999;84:2691–2695.
syndrome: systematic review and meta-anal- for hirsutism: into the limelight, at last. Nat 241 US Medical Eligibility Criteria for Contra-
ysis. Hum Reprod Update 2015;21:560–574. Rev Endocrinol 2010;6:421–422. ceptive Use, 2010. MMWR Recomm Rep
220 Ladson G, Dodson WC, Sweet SD, Ar- 231 Ganie MA, Khurana ML, Eunice M, Gupta 2010;59:1–86.
chibong AE, Kunselman AR, Demers LM, N, Gulati M, Dwivedi SN, Ammini AC: 242 Bonny AE, Ziegler J, Harvey R, Debanne
Lee PA, Williams NI, Coney P, Legro RS: Ef- Comparison of efficacy of spironolactone SM, Secic M, Cromer BA: Weight gain in
fects of metformin in adolescents with poly- with metformin in the management of poly- obese and nonobese adolescent girls initiat-
cystic ovary syndrome undertaking lifestyle cystic ovary syndrome: an open-labeled ing depot medroxyprogesterone, oral con-
therapy: a pilot randomized double-blind study. J Clin Endocrinol Metab 2004; 89: traceptive pills, or no hormonal contracep-
study. Fertil Steril 2011;95:2595–2598.e1–e6. 2756–2762. tive method. Arch Pediatr Adolesc Med
221 Allen HF, Mazzoni C, Heptulla RA, Murray 232 Ganie MA, Khurana ML, Nisar S, Shah PA, 2006;160:40–45.
MA, Miller N, Koenigs L, Reiter EO: Ran- Shah ZA, Kulshrestha B, Gupta N, Zargar 243 Harel Z, Johnson CC, Gold MA, Cromer B,
domized controlled trial evaluating response MA, Wani TA, Mudasir S, Mir FA, Taing S: Peterson E, Burkman R, Stager M, Brown
to metformin versus standard therapy in the Improved efficacy of low-dose spironolac- R, Bruner A, Coupey S, Hertweck P, Bone
treatment of adolescents with polycystic tone and metformin combination than ei- H, Wolter K, Nelson A, Marshall S, Ba-
ovary syndrome. J Pediatr Endocrinol Metab ther drug alone in the management of wom- chrach LK: Recovery of bone mineral den-
2005;18:761–768. en with polycystic ovary syndrome (PCOS): sity in adolescents following the use of de-
222 Al-Zubeidi H, Klein KO: Randomized clini- a six-month, open-label randomized study. pot medroxyprogesterone acetate contra-
cal trial evaluating metformin versus oral J Clin Endocrinol Metab 2013; 98: 3599– ceptive injections. Contraception 2010; 81:
contraceptive pills in the treatment of ado- 3607. 281–291.
lescents with polycystic ovarian syndrome. J 233 Ibáñez L, Valls C, Ferrer A, Ong K, Dunger 244 Francis JKR, Gold MA: Long-acting revers-
Pediatr Endocrinol Metab 2015;28:853–858. DB, de Zegher F: Additive effects of insulin- ible contraception for adolescents. A review.
223 Bridger T, MacDonald S, Baltzer F, Rodd C: sensitizing and anti-androgen treatment in JAMA Pediatr 2017;171:694–701.
Randomized placebo-controlled trial of young, nonobese women with hyperinsulin- 245 Palomba S, de Wilde MA, Falbo A, Koster
metformin for adolescents with polycystic ism, hyperandrogenism, dyslipidemia, and MP, La Sala GB, Fauser BC: Pregnancy com-
ovary syndrome. Arch Pediatr Adolesc Med anovulation. J Clin Endocrinol Metab 2002; plications in women with polycystic ovary
2006;160:241–246. 87:2870–2874. syndrome. Hum Reprod Update 2015; 21:
224 El Maghraby H, Nafee T, Guiziry D, El- 234 Keleştimur F, Everest H, Unlühizarci K, 575–592.
nashar A: Randomized controlled trial of the Bayram F, Sahin Y: A comparison between 246 Kuchenbecker WK, Groen H, van Asselt SJ,
effects of metformin versus combined oral spironolactone and spironolactone plus fin- Bolster JH, Zwerver J, Slart RH, Vd Jagt EJ,
contraceptives in adolescent PCOS women asteride in the treatment of hirsutism. Eur J Muller Kobold AC, Wolffenbuttel BH, Land
through a 24 month follow up period. Mid- Endocrinol 2004;150:351–354. JA, Hoek A: In women with polycystic ova-
dle East Fertil Soc J 2015;20:131–137. 235 Mastorakos G, Koliopoulos C, Creatsas G: ry syndrome and obesity, loss of intra-ab-
225 Ibáñez L, Potau N, Ferrer A, Rodriguez-Hi- Androgen and lipid profiles in adolescents dominal fat is associated with resumption of
erro F, Marcos MV, de Zegher F: Anovula- with polycystic ovary syndrome who were ovulation. Hum Reprod 2011; 26: 2505–
tion in eumenorrheic, nonobese adolescent treated with two forms of combined oral 2512.
girls born small for gestational age: insulin contraceptives. Fertil Steril 2002; 77: 919– 247 Jones H, Sprung VS, Pugh CJ, Daousi C, Ir-
sensitization induces ovulation, increases 927. win A, Aziz N, Adams VL, Thomas EL, Bell
lean body mass, and reduces abdominal fat 236 Mastorakos G, Koliopoulos C, Deligeoro- JD, Kemp GJ, Cuthbertson DJ: Polycystic
excess, dyslipidemia, and subclinical hyper- glou E, Diamanti-Kandarakis E, Creatsas G: ovary syndrome with hyperandrogenism is
androgenism. J Clin Endocrinol Metab Effects of two forms of combined oral con- characterized by an increased risk of hepatic
2002;87:5702–5705. traceptives on carbohydrate metabolism in steatosis compared to nonhyperandrogenic
226 Ibáñez L, Valls C, Ferrer A, Marcos MV, Ro- adolescents with polycystic ovary syndrome. PCOS phenotypes and healthy controls, in-
driguez-Hierro F, de Zegher F: Sensitization Fertil Steril 2006;85:420–427. dependent of obesity and insulin resistance.
to insulin induces ovulation in nonobese ad- 237 Battaglia C, Mancini F, Fabbri R, Persico N, J Clin Endocrinol Metab 2012; 97: 3709–
olescents with anovulatory hyperandrogen- Busacchi P, Facchinetti F, Venturoli S: Poly- 3716.
Update: PCOS Pathophysiology, Horm Res Paediatr 25
Diagnosis, and Treatment DOI: 10.1159/000479371
You might also like
- Lecture Outline: See Separate Powerpoint Slides For All Figures and Tables Pre-Inserted Into Powerpoint Without NotesDocument43 pagesLecture Outline: See Separate Powerpoint Slides For All Figures and Tables Pre-Inserted Into Powerpoint Without NotessyafiqahNo ratings yet
- Developmental Endocrinology From Research To Clinical Practice Contemporary Endocrinology 1st Edition Erica A. Eugster All Chapter Instant DownloadDocument84 pagesDevelopmental Endocrinology From Research To Clinical Practice Contemporary Endocrinology 1st Edition Erica A. Eugster All Chapter Instant Downloadkanduukhaire100% (4)
- The Diagnosis of Polycystic Ovary Syndrome During AdolescenceDocument14 pagesThe Diagnosis of Polycystic Ovary Syndrome During AdolescenceFelipe Correa AraNo ratings yet
- Polycystic Ovary SyndromeDocument13 pagesPolycystic Ovary SyndromeLIZARDO CRUZADO DIAZNo ratings yet
- Jurnal 1Document8 pagesJurnal 1lomba Panah Dies UnsriNo ratings yet
- Polycystic Ovarian Syndrome: Effect of Hormones, Associated Comorbidities and Recent Advances in TherapyDocument12 pagesPolycystic Ovarian Syndrome: Effect of Hormones, Associated Comorbidities and Recent Advances in TherapyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Impact of Polycystic Ovary, Metabolic Syndrome and Obesity on Women Health: Volume 8: Frontiers in Gynecological EndocrinologyFrom EverandImpact of Polycystic Ovary, Metabolic Syndrome and Obesity on Women Health: Volume 8: Frontiers in Gynecological EndocrinologyNo ratings yet
- (FREE PDF Sample) Type 1 Diabetes Etiology and Treatment Contemporary Endocrinology 1st Edition Mark A. Sperling EbooksDocument84 pages(FREE PDF Sample) Type 1 Diabetes Etiology and Treatment Contemporary Endocrinology 1st Edition Mark A. Sperling Ebooksviktarukani100% (2)
- PCOSDocument9 pagesPCOSHardikNo ratings yet
- Taieb Et Al 2024 Rethinking the Terminology a Perspective on Renaming Polycystic Ovary Syndrome for an Enhanced (1)Document11 pagesTaieb Et Al 2024 Rethinking the Terminology a Perspective on Renaming Polycystic Ovary Syndrome for an Enhanced (1)IbrahimNo ratings yet
- 3 - Pcos Tog 2017Document11 pages3 - Pcos Tog 2017Siti NurfathiniNo ratings yet
- Insulin Resistance and PCOS-dr. Hilma Final 11 Juli 2021 FIXDocument48 pagesInsulin Resistance and PCOS-dr. Hilma Final 11 Juli 2021 FIXputrihealthirezaNo ratings yet
- Buy ebook Selective Estrogen Receptor Modulators Research and Clinical Applications 1st Edition Stefan Nilsson Phd cheap priceDocument60 pagesBuy ebook Selective Estrogen Receptor Modulators Research and Clinical Applications 1st Edition Stefan Nilsson Phd cheap priceerisalinglhc100% (4)
- Jurnal Pcos InternationalDocument5 pagesJurnal Pcos InternationalPuput Anistiya Hariani100% (1)
- Anupama Sharma, Et AlDocument10 pagesAnupama Sharma, Et AlAGERI PUSHPALATHANo ratings yet
- Polycystic Ovary Syndrome Throughout A Woman's LifeDocument15 pagesPolycystic Ovary Syndrome Throughout A Woman's LifeMDLuchoNo ratings yet
- Original Research PaperDocument4 pagesOriginal Research PaperOviya ChitharthanNo ratings yet
- Pcos ApprovedDocument30 pagesPcos ApprovedEsha BhatiaNo ratings yet
- Cureus 0016 00000053951Document9 pagesCureus 0016 00000053951hassan hamayalNo ratings yet
- Polycysticovarysyndrome Inadolescents: Selma Feldman Witchel,, Hailey Roumimper,, Sharon OberfieldDocument16 pagesPolycysticovarysyndrome Inadolescents: Selma Feldman Witchel,, Hailey Roumimper,, Sharon OberfieldAgustina S. SelaNo ratings yet
- Final-5 Ayurvedic - Treatment - of - Polycystic - Ovary - Syndrome - PCOS-2022-02-16-08-23Document4 pagesFinal-5 Ayurvedic - Treatment - of - Polycystic - Ovary - Syndrome - PCOS-2022-02-16-08-23Deepak KumarNo ratings yet
- Polycystic Ovary SyndromeDocument13 pagesPolycystic Ovary SyndromeNAYSHA YANET CHAVEZ RONDINELNo ratings yet
- Midyr Case Study NewDocument18 pagesMidyr Case Study NewAndres Ham Samson BernabeNo ratings yet
- Awareness of Lifestyle Modification in Females Diagnosed With Polycystic Ovarian Syndrome in India: Explorative StudyDocument7 pagesAwareness of Lifestyle Modification in Females Diagnosed With Polycystic Ovarian Syndrome in India: Explorative StudyMirza FinandarNo ratings yet
- Adolescent Varicocele Who Is at RiskDocument8 pagesAdolescent Varicocele Who Is at Riskmayicem665No ratings yet
- AContemporaryViewofMenopausalHormoneTherapy-1718207786634Document12 pagesAContemporaryViewofMenopausalHormoneTherapy-1718207786634Grilla fivepointzeroNo ratings yet
- Current Management of PCOSDocument46 pagesCurrent Management of PCOSFauzan MasriNo ratings yet
- 沙特3分河南PCOS PDFDocument7 pages沙特3分河南PCOS PDFmeltwithsnow163.comNo ratings yet
- Saudi Journal of Biological Sciences: Mingsan Miao, Mengfan Peng, Zhengwang Zhu, Xiaoli Yan, Zhenzhen Wei, Mengyan LiDocument7 pagesSaudi Journal of Biological Sciences: Mingsan Miao, Mengfan Peng, Zhengwang Zhu, Xiaoli Yan, Zhenzhen Wei, Mengyan Limeltwithsnow163.comNo ratings yet
- A Review: Brief Insight Into Polycystic Ovarian SyndromeDocument7 pagesA Review: Brief Insight Into Polycystic Ovarian SyndromeAnh Vũ Hồ NgọcNo ratings yet
- Pcos Fto 8Document11 pagesPcos Fto 8Rafli RizaldyNo ratings yet
- Diet and Lifestyle Modifications For Effective Management of PCOSDocument13 pagesDiet and Lifestyle Modifications For Effective Management of PCOSZoe PeregrinaNo ratings yet
- Male Hypogonadism - Basic, Clinical, and Therapeutic Principles PDFDocument407 pagesMale Hypogonadism - Basic, Clinical, and Therapeutic Principles PDFMansoor Abbas100% (1)
- Pediatrics Goatsmilk2010 Basnet E973 7Document8 pagesPediatrics Goatsmilk2010 Basnet E973 7Leli Khairani AdnanNo ratings yet
- Aub 15Document28 pagesAub 15Nadiah Baharum ShahNo ratings yet
- Diamanti Kandarakis2012 PDFDocument50 pagesDiamanti Kandarakis2012 PDFLoly GuerreroNo ratings yet
- Armijo Sanchez Et Al 2024 Treatment With A Patented 3 6 1 Myo Inositol To D Chiro Inositol Ratio Antioxidants VitaminsDocument10 pagesArmijo Sanchez Et Al 2024 Treatment With A Patented 3 6 1 Myo Inositol To D Chiro Inositol Ratio Antioxidants Vitaminshassan hamayalNo ratings yet
- Dok PCOSDocument56 pagesDok PCOSasriNo ratings yet
- Rehabilitation Care of Women With PCOS ADocument3 pagesRehabilitation Care of Women With PCOS AsanyengereNo ratings yet
- CP Rates Among LBW Infants Fell in The 1990sDocument7 pagesCP Rates Among LBW Infants Fell in The 1990sЯковлев АлександрNo ratings yet
- Polycystic Ovary SyndromeDocument6 pagesPolycystic Ovary SyndromealemNo ratings yet
- Jeanes 2017Document9 pagesJeanes 2017ThormmmNo ratings yet
- PCOS-Journal Article 2Document8 pagesPCOS-Journal Article 2dinarosman02No ratings yet
- Prenatal Androgen Excess Induces Multigenerational Effects On Female and Male DescendantsDocument15 pagesPrenatal Androgen Excess Induces Multigenerational Effects On Female and Male Descendantstajeyi2393No ratings yet
- Leptin and PCOSDocument8 pagesLeptin and PCOSNasheen NaidooNo ratings yet
- Article: Hormonal Profile and Reproductive Potential of Polycystic Ovary Syndrome (Pcos) Women in IndonesiaDocument9 pagesArticle: Hormonal Profile and Reproductive Potential of Polycystic Ovary Syndrome (Pcos) Women in IndonesiafirmianisaNo ratings yet
- Dietary Patterns and Polycystic Ovary Syndrome - A Systematic ReviewDocument6 pagesDietary Patterns and Polycystic Ovary Syndrome - A Systematic ReviewKatia Sosa VeraNo ratings yet
- Pediatrics Goatsmilk2010 Basnet E973 7Document8 pagesPediatrics Goatsmilk2010 Basnet E973 7Supri AdiNo ratings yet
- Introduction PCOSDocument14 pagesIntroduction PCOSalex.avenko1030No ratings yet
- Adgent Et Al - 2018 - A Longitudinal Study of Estrogen-Responsive Tissues and Hormone ConcentrationsDocument11 pagesAdgent Et Al - 2018 - A Longitudinal Study of Estrogen-Responsive Tissues and Hormone ConcentrationsBerry BancinNo ratings yet
- PIIS0022347617301828Document4 pagesPIIS0022347617301828adkhiatul muslihatinNo ratings yet
- Prevalence and Risk Factors of Persistent Stress Urinary Incontinence at Three MonthsDocument5 pagesPrevalence and Risk Factors of Persistent Stress Urinary Incontinence at Three MonthsDwickyNo ratings yet
- IJRAR23D2391Document6 pagesIJRAR23D2391Itti MishraNo ratings yet
- ACOG Contemporary View of Menopausal Hormone TherapyDocument12 pagesACOG Contemporary View of Menopausal Hormone Therapyluks26No ratings yet
- PCODDocument14 pagesPCODHardikNo ratings yet
- A New Approach To Polycystic Ovary Syndrome: The Gut MicrobiotaDocument13 pagesA New Approach To Polycystic Ovary Syndrome: The Gut MicrobiotaSagung Ayuska GandhariNo ratings yet
- Final Presentation - Fouzia Hassan Ananna 0Document24 pagesFinal Presentation - Fouzia Hassan Ananna 0princessporipromaNo ratings yet
- Insulin Resistance in Polycystic Ovary Syndrome Across Various Tissues - An Updated Review of Pathogenesis, Evaluation, and TreatmentDocument18 pagesInsulin Resistance in Polycystic Ovary Syndrome Across Various Tissues - An Updated Review of Pathogenesis, Evaluation, and TreatmenthamoodNo ratings yet
- Chapitre 3Document39 pagesChapitre 3Rania BouabdallahNo ratings yet
- MP Whyte 2019Document13 pagesMP Whyte 2019Esteban Mercol EcheverríaNo ratings yet
- 2020 Fifteen-minute Consultation- The Overweight Teenage Girl With AcneDocument6 pages2020 Fifteen-minute Consultation- The Overweight Teenage Girl With AcneMaria Thereza MoraisNo ratings yet
- Jurnal 8Document9 pagesJurnal 8Ade Yurga TonaraNo ratings yet
- Jurnal 7Document10 pagesJurnal 7Ade Yurga TonaraNo ratings yet
- Microbiology of Chronic Suppurative Otitis Media: A Prospective Study in A Tertiary Care HospitalDocument4 pagesMicrobiology of Chronic Suppurative Otitis Media: A Prospective Study in A Tertiary Care HospitalAde Yurga TonaraNo ratings yet
- Fix 3Document8 pagesFix 3Ade Yurga TonaraNo ratings yet
- Acne VulgarisDocument21 pagesAcne VulgarisAde Yurga TonaraNo ratings yet
- Derek G. Waller, Andrew W. Hitchings, Anthony P. Sampson - Medical Pharmacology and Therapeutics-Elsevier (2022) (перетянутый)Document18 pagesDerek G. Waller, Andrew W. Hitchings, Anthony P. Sampson - Medical Pharmacology and Therapeutics-Elsevier (2022) (перетянутый)kabulkabulovich5No ratings yet
- Opioid-Induced Androgen DeficiencyDocument12 pagesOpioid-Induced Androgen DeficiencyMikaelNo ratings yet
- Medroxyprogesterone AcetateDocument3 pagesMedroxyprogesterone Acetateapi-3797941No ratings yet
- Bio Essay On HormonesDocument3 pagesBio Essay On HormonesDarshana PatelNo ratings yet
- Unidajump2019,+6 +djunaediDocument10 pagesUnidajump2019,+6 +djunaeditri septianiNo ratings yet
- Synthesis of Steroid HormonesDocument54 pagesSynthesis of Steroid HormonesMing ZhaoNo ratings yet
- HormonesDocument13 pagesHormonesethankhoo2007No ratings yet
- Adrenal CrisisDocument13 pagesAdrenal CrisisNisa UcilNo ratings yet
- DLL Mod.1 Part 1 3RD QRTR G10Document4 pagesDLL Mod.1 Part 1 3RD QRTR G10Jr CapanangNo ratings yet
- Pemakaian Kontrasepsi Suntik Dmpa Dan Kejadian Amenorea Sekunder Di Wilayah Kerja Puskesmas Lepo-Lepo Kota KendariDocument7 pagesPemakaian Kontrasepsi Suntik Dmpa Dan Kejadian Amenorea Sekunder Di Wilayah Kerja Puskesmas Lepo-Lepo Kota KendarievizaNo ratings yet
- Lecture Discussion With QUIZDocument11 pagesLecture Discussion With QUIZAJ BayNo ratings yet
- Chapter 15 - Hypercalcemia and Primary HyperparathyroidismDocument46 pagesChapter 15 - Hypercalcemia and Primary HyperparathyroidismSteffi AraujoNo ratings yet
- Biochem QuizDocument2 pagesBiochem QuizAiramel Shekina AlborNo ratings yet
- TP Thyroid Nodules 1Document59 pagesTP Thyroid Nodules 1Meaw Thitirat SupasilNo ratings yet
- The Female Reproductive System Is Designed To Carry Out Several FunctionsDocument2 pagesThe Female Reproductive System Is Designed To Carry Out Several FunctionsArdie MingayNo ratings yet
- A Semi Detailed Lesson Plan in ScienceDocument3 pagesA Semi Detailed Lesson Plan in ScienceI AM ANONYMOUSNo ratings yet
- Conceptual and Ayurvedic Management Approach in Yuvanpidika W.S.R. To Acne VulgarisDocument6 pagesConceptual and Ayurvedic Management Approach in Yuvanpidika W.S.R. To Acne VulgarisIJAR JOURNALNo ratings yet
- DiabetesMellitusMasterclass MedmasteryHandbookDocument88 pagesDiabetesMellitusMasterclass MedmasteryHandbookDeenissa Van GawaranNo ratings yet
- About Duphaston and Why Is It Used ForDocument2 pagesAbout Duphaston and Why Is It Used ForbrenskieNo ratings yet
- Physiology and PubertyDocument8 pagesPhysiology and PubertynofiajahNo ratings yet
- Case StudyDocument9 pagesCase Studyapi-740607793No ratings yet
- Hypothalamus-Pituitary-Thyroid Axis: PRESENTERS: DR: Nyangaresi Justine DR: Mitchelle Facilitator: DRDocument31 pagesHypothalamus-Pituitary-Thyroid Axis: PRESENTERS: DR: Nyangaresi Justine DR: Mitchelle Facilitator: DRJustine NyangaresiNo ratings yet
- Materi To Interna 02 FebruariDocument75 pagesMateri To Interna 02 FebruariMario AlexanderNo ratings yet
- Etiopathogenesis of Diabetes MellitusDocument35 pagesEtiopathogenesis of Diabetes MellitusironNo ratings yet
- ThyroidDocument102 pagesThyroidfadoNo ratings yet
- Tugas Individu LKMMDocument4 pagesTugas Individu LKMMMuhammad Rizki QomarNo ratings yet
- Thyroid DissertationDocument7 pagesThyroid DissertationCustomPaperWritingServiceNorthLasVegas100% (2)
- Endocrine Gland....Document62 pagesEndocrine Gland....Sabita TripathiNo ratings yet
- 2017 Steroid Tapering Guideline Cancer NHS Foundation TrustDocument1 page2017 Steroid Tapering Guideline Cancer NHS Foundation TrustArdan MirazNo ratings yet