NCP Drug
NCP Drug
Uploaded by
Mhar CamposanoCopyright:
Available Formats
NCP Drug
NCP Drug
Uploaded by
Mhar CamposanoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
NCP Drug
NCP Drug
Uploaded by
Mhar CamposanoCopyright:
Available Formats
DRUG NAME Generic Name:
CLASSIFICA -TION Antibiotic
DOSAGE/ ROUTE Maximum recommended dosage is 6g/day. Adults and pediatric patients weighing 40kg or more: 250-500 mg every 4-6 hr IM or IV. Up to 1g every 4-6 hr in severe infections.
ACTION
INDICATION CONTRAINDICATION Infectious due to penicillinase producing staphylococci; may be used to initiate treatment when a staphylococci infection is suspected Contraindicated with allergies to penicillins, cephalosporins or other allergens
ADVERSE EFFECT CNS: lethargy, hallucinations, seizures GI: glossitis, stomatitis, gastritis, sore mouth furry and black hairy tongue, nausea and vomiting, diarrhea HEMATOLOGIC: anemia, thrombocytopenia , neutropenia, prolonged bleeding time HYPERSENSITIVITY: rash, phlebitis, thrombosis at injection site OTHER:superinfe ction
NURSING INTERVENTION Obtain specimen for culture and sensitivity tests before first dose. To prevent vein irritation, avoid continuous infusions. Change site every 48 hours. Give 1-2 hours before or 2-3 hours after meals to prevent gastric irritation.
PenicillinaseOXACILLIN resistant SODIUM penicillin Brand Name: Bactocill
Bactericidal: inhibits cell wall cell wall of sensitive organisms, causing cell death
DRUG NAME Generic Name: AMINO ACIDS Brand Name: Aminosyn, Freamine - Travasol
CLASSIFICATION Caloric agent Protein Substrate
DOSAGE/ ROUTE Recommended protein dietary allowance are 0.9 g/kg/day for healthy adult, 1.4-2.2 g/kg/day in healthy infants and children Adults: 1-1.5 g/kg/day amino acid injection IV into the peripheral vein, 250-500 ml/day amino acid injection IV mixed with appropriate dextrose, vitamins, and electrolytes as part of a total parenteral nutrition (TPN) solution
ACTION Essential and nonessentials amino acids provides in various combinations to supply calories and proteins and provide a protein building and proteinsparing effect for the body ( a positive nitrogen balance)
INDICATIONS Provide nutrition to patients who are in a negative nitrogen balance when GI tract cannot absorb protein, when protein needs exceed the ability to absorb protein (with burns, trauma, infections); when bowel rest is needed; when tube feeding cannot supply adequate nutrition; when health can be improved or restore by replacing lost amino acids Treatment of hepatic
CONTRAINDICATION Contraindicated with hypersensitivity to any component of the solution; severe electrolyte acid-base imbalance; inborn errors in amino acid metabolism; decreased circulating blood volume; severe renal or hepatic disease; hyperammonenia; bleeding abnormalities.
ADVERSE EFFECT CNS: headache, dizziness, mental confusion, loss of conscious-ness
NURSING INTERVENTION
Assess nutritional status before and frequently during treatment; CV:hyperten-sion, weight the pulmona-ryedema, patient daily to generalized flushing monitor fluid load and Endocrine:hypoglycenia, nutritional status hyperglycemia, fatty acid deficiency, azotemia Monitor vital signs often GI: nausea, vomiting, during infusion abdominal pain, liver impairment, fatty liver Observe infusion site atleast daily Local: pain, infection for infection, phlebitis venous phlebitis; change thrombosis, tissue the dressing sloughing at injection using strict site aseptic technique atleast every 24 hr. Arrange to give D5W or D10W for injection by a peripheral line to avoid hypoglycemia
encephalopathy in patients with cirrhosis or hepatitis Nutritional support of uremic patients when oral nutrition is not feasible or is impractical or insufficient.
rebound if TPN infusion needs to be stopped. Monitor urine glucose, acetone, and specific gravity every 6 hrduring initial infusion period, atleast bid when the infusion stabilized; stop solution at any sign of renal failure Monitor patient for vascular overload or hepatic impairement.
DRUG NAME
CLASSIFICA -TION Aldosterone agonist Potassium sparing diuretic
DOSAGE/ ROUTE Adults: Edema: Initially, 100 mg/day (range 25100mg/day) when given as the sole agent; continue atleast 5 days, then adjust dosage or add another diuretic or both Hypokalemia: 25-100 mg/day PO
ACTION
INDICATION
CONTRAINDICATION Contraindicat ed with allergy to spironolacton e, hyperkalemia, renal disease, anuria, amiloride or triamterene use.
ADVERSE EFFECT CNS: dizziness, headache, drowsiness, fatigue, ataxia, confusion DERMATOLOGIC: Rash, urticarial GI: impotence, irregular menses, amenorrhea, postmenopausal bleeding HEMATOLOGIC:h yperalemia, hyponatremia, agranulocytosis OTHER:Carcinoge nc in animals, deepening of the voice, hisutism, gynecomastia
NURSING INTERVENTION Mark calendars of edema outpatients as reminders of alternate- day or 3- to 5-day/wk therapy Give daily doses early so that increased urination does not interfere with sleep Measure and record regular weight to monitor mobilization of edema fluid Avoid giving food rich in potassium
Generic Name: Spironolactone Brand name: - Aldctone - Novospiroton
Completitively blocks the effects of aldosterone in the renal tubule, causing loss of sodium and water and retention of potassium
Diagnosis and maintenance of primary hyperaldosternism Adjenctive therapy in edema associated with HF, nephrotic syndrome, hepatic cirrhosis when other therapies are inadequate or inappropriate Treatment of hypokalemia or prevention of hypokalemia in patients who would be at risk if hypokalemiaoccu red
Drug Name Generic name: Diazepam Brand name: Valium
Classificati on Antiepileptic Anxiolytic
Dosage/Rou te Individuals dosage; increase dosage cautiously to avoid adverse effects. Usual dose is 2-20mg IM or IV. Larger doses may be required for some indications (tetanus). Injections may be repeated in 1 hr. >muscle spasm: 510mg IM or IV initially,then 5-10 mg in 34 hr if necessary. >Anxiety: 210 mg IM or IV; repeat in 3-4 hr if
Actions Exact mechanisms of action not understood; acts mainly at the limbic system and reticular formation; may act in spinal cord and at supraspinal spines to produce skeletal muscle relaxation; potentiates the effects of GABA, an inhibitory neurotransmitter; anxiolytic effects occur at doses well below those necessary to cause sedation, ataxia; has little effect on cortical function.
Indications >Management of anxiety disorders or for short-term relief of symptoms of anxiety. >Acute alcohol withdrawal; may be useful in symptomatic relief of acute agitation, tremor, delirium tremens, hallucinosis. >Muscle relaxant >Parenteral: treatment of tetanus >Antiepileptic: adjunct in status epilepticus and severe recurrent convulsive seizures
Contraindicatio ns Contraindicated with hypersensitivity to benzodiazepines; psychoses; acute narrow-angle glaucoma, shock, coma, acute alcoholic intoxication; pregnancy (cleft lip or palate, inguinal hernia, cardiac defects, microcephaly, pyloric stenosis when used in first trimester, neonatal withdrawal syndrome reported in newborns); lactation
Adverse Effects >CNS: transient, mild drowsiness initially; sedation, depression, lethargy, apathy, fatigue, lightheadedness, disorientation, restlessness, confusion, crying >CV: Bradycardia, tachycardia, CV collapse, hypertension and hypotension, palpitations, edema >DEPENDENCE: Drug dependence with withdrawal syndrome when drug is discontinued >DERMATOLOGI C: Urticaria, pruritus, skin rash, dermatitis
Nursing Interventions >Do not administer intra-arterially; may produce arteriospasm, gangrene. >Change from IV to oral therapy as soon as possible >Do not use small veins for IV injection >reduce dose of opioid analgesics with IV diazepam; dose should be reduced by at least one-third or eliminated. >Carefully monitor BP, P, respiration during IV administration >Maintain patients receiving parenteral benxodiazepines in bed for 3 hr; do not permit ambulatory patients to operate a vehicle following an injection.
necessary
>GI: Constipation, diarrhea, dry mouth, salivation, nausea ,anorexia, vomiting, difficulty I swallowing >GU: Incontinence, urinary retention, changes in libido, menstrual irregularities >HEMATOLOGIC: Decreased Hct, blood dyscrasias
Drug Name Generic name: Ranitidine HCl
Classification Dosage/Route Histamine-2 antagonist >Acute duodenal ulcer: 150 mg bid PO for 4-8 wk. Alternatively 300 mg PO once a day at bedtime or 50 mg IM or IV every 6-8 hr or by intermittent IV infusion >Diluted to 100 ml and infused over 15-20 mis.Do not exceed 400 mg/day.
Actions Competitively inhibits the action of histamine at the H2 receptors of the parietal cells of the stomach, inhibiting basal gastric acid secretion and gastric acid secretion that is stimulated by food, insulin, histamine, cholinergic agonists, gastrin and pentagastrin.
Indications >Short-term treatment of active duodenal ulcer >Maintenance therapy for duodenal ulcer at reduced dosage >Short-term treatment and maintenance therapy of active, benign gastric ulcer >short-term treatment of GERD >treatment of erosive esophagitis
Contraindications >Contraindicated with allergy to ranitidine, lactation.
Adverse Effects >CNS: headache, malaise, dizziness, somnolence, insomnia, vertigo >CV: tachycardia, bradycardia, PVCs
Nursing Interventions >Administer oral drug with meal and at bedtme.
Brand name: Zantac
>Decrease doses in renal and liver >DERMATOLOGIC: failure. >Provide >GI: concurrent constipation,diarrhea, antacid hepatitis, abdominal therapy to pain relieve pain. >GU: gynecomastia
>HEMATOLOGIC: leucopenia, granulocytopenia, thrombocytopenia, pancytopenia >LOCAL: Pain at IM site, local burning or itching at IV site >OTHER: arthralgias
>Administer IM dose undiluted, deep into large muscle group. >Arrange for regular followup, including blood tests, to evacuate effects.
Drug Name
Classificatio n >Amebicide >Antibacteria l >Antibiotic >Antiprotozo al
Dosage/Route
Actions
Indications
Contraindicatio ns Contraindicated with hypersensitivity to metronidazole; pregnancy (do not use for trichomoniasis in 1st trimester).
Adverse Effects
Nursing Intervention s Avoid use unless needed. Metronidazole may be carcinogenic. >Administer oral doses with food. >Apply topically (MetroGel) after cleansing the area. Advise patient that cosmetics may be used over the area after application. >Reduce dosage in hepatic disease.
Generic name: Metronidazol e Brand name: Protostat, Vandazole
ORAL
Bactericidal: Inhibits DNA >amebiasis: 750 synthesis in mg PO tid for 5-10 specific days. anaerobes, causing cell >antibioticdeath; associated antiprotozoalpseudomembrano trichomonacida us colitis: 1-2 l, amebicidal: g/day PO in 3-4 Biochemical divided doses for mechanism of 7-10 days. actions is not known. >giardiasis:250 mg PO tid for 7 days. IV Anaerobic bacterial infection: 15 mg/kg IV infused over 1 hr; then 7.5 mg/kg infused over 1 hr every 6 hr for 710 days, not to exceed 4 g/day.
>Acute infection with susceptible anaerobic bacteria >Acute intestinal amebiasis >Amebic liver abscess >trichomonias is >bacterial vaginosis >Preoperative, intraoperative, postoperative prophylaxis for patients undergoing colorectal surgery >Topical application:
>CNS: headache, dizziness, ataxia, vertigo, incoordination, insomnia, seizures, peripheral neuropathy, fatigue >GI: unpleasant metallic taste, anorexia, nausea, vomiting, diarrhea, GI upset, cramps >GU: dysuria, incontinence,darkeni ng of the urine >LOCAL: thrombophlebitis (IV); redness, burning, dryness, amd skin irritation on topical medication >OTHER: severe, disulfiram-like interaction with alcochol, candidiasis (superinfection)
Treatment of inflammatory papules, pustules, and erythema of rosacea
Assessment Subjective: ------
Diagnosis Activity Intolerance related to involuntary muscle contractions as manifested by restlessness, neck rigidity, reflex spasm, and spasm of the jaw.
Planning After 8 hours of nursing intervention the patients relatives will verbalize understanding of situation and individual treatment regimen and safety measures. After 2 weeks of nursing intervention an improvement in patients condition will be seen as manifested by decreased involuntary movements, and increased ability to recognize his condition and be able to prevent secondary side effects such as falls or injury.
Intervention -Monitor vital signs every 2 hours.
Rationale -To note changes and possible signs of complication, improvement and serves as baseline data -To maintain position of function and reduce the risk of pressure ulcers
Evaluation After 8 hours of nursing intervention the patients relative was able to understand the situation and provide safety measures. After 2 weeks of rendering nursing intervention: *the patient's condition had improved *the patient had been able to demonstrate coping behaviors in preventing secondary side effects of the present condition.
Objectives: Vital Signs BP: 100/60mmHg BT: 36C PR: 74BPM RR: 24CPM >Inability to performed ADL > Limited range of motion >uncoordinated jerky movements >limited ability to perform gross motor skill
-Reposition the patient every 2 hours as needed to prevent contractures and pressure sores. -Provide therapeutic environment, placing the patient in a quiet room with a dim light and with a large proximity with other rooms. -Provide safety measures (raise side rails) as indicated in patient situation
-To avoid extrinsic stimulants that will trigger the involuntary muscle contractions of the patient.
-To avoid secondary injuries.
Nursing care plan1
Assessment SUBJECTIVE: Yung Amino Acids lang po na nireseta ni doctora yung pagakain nya and hindi po sya nakakalunok ng pagakain as verbalized by the wife of the patient. OBJECTIVE: (+) trismus or spasm of the jaw (+) TPN of Amino Acids (+) Dysphagia
Diagnosis Altered Nutrition less than body requirement related to Cranial Nerve V impairment as manifested by trismus or spasm of the jaw, difficulty in swallowing and muscle stiffness.
Planning SHORT TERM After 1 week the patient will be able to: -Increase/ Improve body weight. -have normal level of Fluids and Electrolytes. LONG TERM -After 1 month the patient will be able to perform ADL, independently. -After 3 months the patient will able to establish stable nutritional status such as normal body weight.
Intervention -Infuse and maintain TPN of Amino Acid that serves as the clients only source of nutrition. -After the recovery of the patient (2-5 weeks), administer oxygen as ordered by the physician.
Rationale -To support the failing nutritional status of the client and to provide reserve energy requirement. -For the patient to have increased and stable nutritional status by administering osteurized food via NGT insertion. -To serve as the baseline data and to know the nutritional improvement of the client.
Evaluation After 1 week of intervention the client manifests an increase level of body weight for at least 2lbs. Level of Fluid and Electrolytes normalized within a week. After 1 month of rendering care and supporting the client, he shown an improvement in terms of performing ADL independently. After 3 months, the patient established a stable nutritional status.
-Assess and monitor body weight before and after the interventions applied to the client.
Nursing Care Plan 2
Assessment Subjective: Nahihirapan siya huminga as verbalized by the patients wife Objective: Use of accessory muscles Altered RR Difficulty of Breathing Nasal Flaring Irritability Restlessness
Diagnosis Ineffective Breathing pattern related to spasm as evidenced by increase respiratory rate, DOB and nasal flaring
Planning
Intervention
Rationale
Evaluation STG: After an hour of Nursing Intervention Patients DOB was relieved LTG: After 2 weeks of Nursing intervention patient was able to: Demonstrate coping behaviors
STG: STG: STG: After an hour of 1. Administer 1. For management of Nursing Intervention oxygen at underlying Patients DOB lowest pulmonary will be concentration condition, relieved as indicated respiratory distress and prescribed or cyanosis. LTG: respiratory 2. That may restrict or After 2 weeks of medication. limit respiratory Nursing intervention 2. Assess for pain effort. patient will have a: and 3. To promote lung Demonstrate discomfort. expansion. coping 3. Elevate Head 4. To evaluate behaviors of bed as presence or appropriate. character of breathe 4. Auscultate sounds and chest. Secretions. LTG: LTG: 1. Encourage slower or deeper respiration 2. Encourage adequate rest periods between activities. 3. Refer for upper and lower 1. To assist client in taking control of the situation. 2. To limit fatigue. 3. To maximize clients level of functioning. 4. To maximize respiratory effort.
extremity endurance and strength training slowly. 4. Stress importance of good posture and effective use of accessory muscle.
You might also like
- Haiderpur Water Treatment PlantDocument23 pagesHaiderpur Water Treatment Plantakshay malik67% (6)
- Valdez Reflective-Questions PDFDocument3 pagesValdez Reflective-Questions PDFDexel Lorren ValdezNo ratings yet
- Subjective Data:: Assessme NT Diagnos IS Planning Intervention Rationale EvaluationDocument1 pageSubjective Data:: Assessme NT Diagnos IS Planning Intervention Rationale EvaluationCuttie Anne GalangNo ratings yet
- Drugs Study and Discharge Plan Arnold and SelwynDocument17 pagesDrugs Study and Discharge Plan Arnold and SelwynArnold ZamoroNo ratings yet
- Hypothyroidism (Drug Study)Document2 pagesHypothyroidism (Drug Study)Krisianne Mae Lorenzo FranciscoNo ratings yet
- Clinical Problem Solving in Periodontology and ImplantologyDocument195 pagesClinical Problem Solving in Periodontology and ImplantologyEshan Verma100% (21)
- MCN Case Presentation Group 2 1Document68 pagesMCN Case Presentation Group 2 1Mary-Ann JagonobNo ratings yet
- Tetralogy of FallotDocument4 pagesTetralogy of FallotLiezelle ArrozalNo ratings yet
- Intrapartum Assessment: Jonelle Baloloy, MD MCMC Ob GyneDocument39 pagesIntrapartum Assessment: Jonelle Baloloy, MD MCMC Ob GyneJonelle baloloyNo ratings yet
- VenoferinfDocument10 pagesVenoferinfzerin_atinNo ratings yet
- NCP IcuDocument2 pagesNCP IcuDiana MuañaNo ratings yet
- I Patient Assessment Data BaseDocument12 pagesI Patient Assessment Data BaseJanice_Fernand_1603No ratings yet
- Hemolytic Disease of The Newborn: (Erythroblastosis Fetalis)Document17 pagesHemolytic Disease of The Newborn: (Erythroblastosis Fetalis)sandeepv08No ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale Core CompetenciesDocument13 pagesAssessment Nursing Diagnosis Planning Intervention Rationale Core CompetenciesMina RacadioNo ratings yet
- Module4 Promabortion Week 8Document21 pagesModule4 Promabortion Week 8Emmy Flor ValmoriaNo ratings yet
- Drug Study SpironolactoneDocument2 pagesDrug Study SpironolactonePau-pau BasiNo ratings yet
- Chapter 1. Physical Activity and Exercise: Learning OutcomesDocument5 pagesChapter 1. Physical Activity and Exercise: Learning OutcomesKrish NalingNo ratings yet
- Acetaminophen (Tylenol)Document2 pagesAcetaminophen (Tylenol)amelia hearonNo ratings yet
- Name of Drug Mechanism of Action Indications Contra-Indications Side Effects Nursing ConsiderationsDocument10 pagesName of Drug Mechanism of Action Indications Contra-Indications Side Effects Nursing ConsiderationsmidskiescreamzNo ratings yet
- Lower Limb Trauma - 5Document12 pagesLower Limb Trauma - 5Renee RoSeNo ratings yet
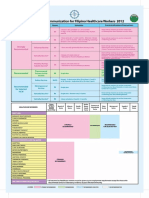
- Recommended Immunization For Filipino Healthcare Workers 2012Document1 pageRecommended Immunization For Filipino Healthcare Workers 2012SMRNo ratings yet
- Risk NCP Decreased Cardiac OutputDocument2 pagesRisk NCP Decreased Cardiac OutputMICHELLE FACTONo ratings yet
- Nursing Care Plan DMDocument8 pagesNursing Care Plan DMnikaaraaaNo ratings yet
- Learning Derived (Lysha)Document1 pageLearning Derived (Lysha)Choy DavidNo ratings yet
- Care Plan PedsDocument7 pagesCare Plan PedsdjbhetaNo ratings yet
- NCPDocument2 pagesNCPNichole Audrey SaavedraNo ratings yet
- Antepartum Haemorrhage MXDocument22 pagesAntepartum Haemorrhage MXAmir Hilmi Abd AzizNo ratings yet
- Case Pres Cerebrovascular DiseaseDocument34 pagesCase Pres Cerebrovascular DiseaseADRIATICO JAROSLUVNo ratings yet
- Phenobarbital Risk For Injury EAMCDocument4 pagesPhenobarbital Risk For Injury EAMCkeitacNo ratings yet
- RLE314 CU4 MedicationDocument7 pagesRLE314 CU4 MedicationVAL ASHLIE ACEBARNo ratings yet
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationDocument5 pagesAssessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationTedd CamilingNo ratings yet
- Warfarin - Drug InformationDocument23 pagesWarfarin - Drug InformationTestesteNo ratings yet
- NCP & Drug Study (Tondo Med)Document5 pagesNCP & Drug Study (Tondo Med)Kevin_Remollo_2431No ratings yet
- Abruptio PlacentaDocument10 pagesAbruptio PlacentaDoc DudayNo ratings yet
- Assessment Nursing Diagnosis Scientific Basis Planning Interventions RationaleDocument3 pagesAssessment Nursing Diagnosis Scientific Basis Planning Interventions RationaleJose Rey BuenavistaNo ratings yet
- Drug Study 12Document4 pagesDrug Study 12Nathalie kate petallarNo ratings yet
- Galantine HBRDocument5 pagesGalantine HBRArone SebastianNo ratings yet
- Febrile Seizures NCPDocument9 pagesFebrile Seizures NCPNurul IrhamnaNo ratings yet
- Pathophysiology (Normal Spontaneous Vaginal Delivery)Document2 pagesPathophysiology (Normal Spontaneous Vaginal Delivery)Jose Bryan NacillaNo ratings yet
- Measuring Blood Glucose LevelDocument7 pagesMeasuring Blood Glucose LevelHuda BehroozNo ratings yet
- Ineffective Tissue PerfussionDocument2 pagesIneffective Tissue Perfussionmonico39No ratings yet
- Drug Study Pyrantel & CefuroximeDocument2 pagesDrug Study Pyrantel & CefuroximeMikhael Briones ApasNo ratings yet
- BFS Uti 111Document65 pagesBFS Uti 111JemsMei Comparativo MensuradoNo ratings yet
- Discharge PlanDocument5 pagesDischarge PlanrraksNo ratings yet
- Drug StudyDocument4 pagesDrug StudyAli Longasa CortezNo ratings yet
- Javier, Jomar A. BSN121 Group 83 Nursing Care Plan (Pediatric Patient)Document7 pagesJavier, Jomar A. BSN121 Group 83 Nursing Care Plan (Pediatric Patient)Julie AnnNo ratings yet
- Pharmacology m7 Post Task CaparasDocument3 pagesPharmacology m7 Post Task CaparasGretta CaparasNo ratings yet
- Case Study, Chapter 42, Management of Patients With Musculoskeletal TraumaDocument2 pagesCase Study, Chapter 42, Management of Patients With Musculoskeletal TraumaAhmad BaolayyanNo ratings yet
- Drug PepcidDocument2 pagesDrug PepcidSrkocher0% (1)
- Young InfantDocument69 pagesYoung InfantAurora Doris BatagaNo ratings yet
- Post-Operative Nutrition: Things You Need To Know AboutDocument2 pagesPost-Operative Nutrition: Things You Need To Know AboutJannen Casas100% (1)
- Drugs Study For Surgery WardDocument4 pagesDrugs Study For Surgery WardMariquita BuenafeNo ratings yet
- Drug StudyDocument33 pagesDrug Studyjefwy8No ratings yet
- NCP Impaired Physical MobilityDocument1 pageNCP Impaired Physical MobilityLorraine Punla PanganNo ratings yet
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument3 pagesSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNo ratings yet
- Placino HIRSCHPRUNG DX PDFDocument15 pagesPlacino HIRSCHPRUNG DX PDFSiena PlacinoNo ratings yet
- Lack of Insulin Decreases Available Glucose For CellDocument1 pageLack of Insulin Decreases Available Glucose For CellvicenteturasNo ratings yet
- IbuprofenDocument2 pagesIbuprofenKate AbadNo ratings yet
- Drugs StudyDocument6 pagesDrugs StudyMark_Rebibis_8528No ratings yet
- Nursing Care Plan (NCP) For SchizophreniformDocument8 pagesNursing Care Plan (NCP) For SchizophreniformRisa Sol AriasNo ratings yet
- Preterm Labor Prevention of DeliveryDocument10 pagesPreterm Labor Prevention of Deliverynursereview100% (1)
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- Alberta Infant Motor Scale (AIMS) - A Clinical Refresher and Update On Evaluation of Normative DataDocument8 pagesAlberta Infant Motor Scale (AIMS) - A Clinical Refresher and Update On Evaluation of Normative DataCamila AlmeidaNo ratings yet
- Pertinent Papers For Fidelity Bond (SY 2020-2021) : Department of EducationDocument7 pagesPertinent Papers For Fidelity Bond (SY 2020-2021) : Department of EducationGregor Chio Jr.No ratings yet
- Position PaperDocument3 pagesPosition Paperapi-385384164No ratings yet
- 1349072656CV Dr. Shaheen N KhanDocument17 pages1349072656CV Dr. Shaheen N KhanTanveer Abbas JafriNo ratings yet
- Technical Rescue Program: Development ManualDocument252 pagesTechnical Rescue Program: Development Manualscoutscathox100% (2)
- Ethics Bush 2005 CasebookDocument27 pagesEthics Bush 2005 CasebookSFMultiservice -No ratings yet
- GSIS V PauigDocument4 pagesGSIS V PauigLovely CondeNo ratings yet
- Ethical Paper Senior SemDocument6 pagesEthical Paper Senior Semapi-643481686No ratings yet
- Omicron Webinar AHSDocument16 pagesOmicron Webinar AHSDian AkbariNo ratings yet
- Green Party Platform 2011Document12 pagesGreen Party Platform 2011chorgsNo ratings yet
- Sample Drug-And-Alcohol-Evaluations-ExampleDocument3 pagesSample Drug-And-Alcohol-Evaluations-ExampleasksundaydealsNo ratings yet
- Manajemen Surveilans Covid-19 Di Wilayah Kerja Bandar Udara Internasional Hang NadimDocument9 pagesManajemen Surveilans Covid-19 Di Wilayah Kerja Bandar Udara Internasional Hang NadimClaudia PataloNo ratings yet
- DLL - Mapeh 6 - Q1 - W1Document4 pagesDLL - Mapeh 6 - Q1 - W1Laine Agustin SalemNo ratings yet
- Construction Method StatementDocument35 pagesConstruction Method StatementHoang ThiNo ratings yet
- Sindrome de Pies UrentesDocument4 pagesSindrome de Pies UrentesIdelberto Torres BenitezNo ratings yet
- NG Sample v6.2Document18 pagesNG Sample v6.2pedro.medina.riosNo ratings yet
- Biopsychosocial ApproachDocument4 pagesBiopsychosocial ApproachUnknown WandererNo ratings yet
- Get The Expectant Father 5th Edition Jennifer Ash Rudick PDF ebook with Full Chapters NowDocument52 pagesGet The Expectant Father 5th Edition Jennifer Ash Rudick PDF ebook with Full Chapters Nowsuyaniewudzi100% (1)
- Maternal and Child Health Nursing (MCN 107) : Joel D. Federico, RN, MAN InstructorDocument28 pagesMaternal and Child Health Nursing (MCN 107) : Joel D. Federico, RN, MAN InstructorJesz E GarciaNo ratings yet
- Perdosri MukernasDocument26 pagesPerdosri MukernasMad MadNo ratings yet
- Shine Medical Technologies PitchBook Company ProfileDocument17 pagesShine Medical Technologies PitchBook Company ProfileJeff BuchananNo ratings yet
- 10.3job Hazard Analysis Worksheet-001Document9 pages10.3job Hazard Analysis Worksheet-001alsakhaa.serviceNo ratings yet
- 2.0 Drug Statistics and TrendsDocument108 pages2.0 Drug Statistics and TrendsAnkita Kaliraman100% (1)
- 5 Sciatica Exercises For Pain Relief (With Pictures) : Back IntelligenceDocument26 pages5 Sciatica Exercises For Pain Relief (With Pictures) : Back Intelligenceanand sahu100% (1)
- Inspeccion Tecnica Edificios.20121016.002759Document2 pagesInspeccion Tecnica Edificios.20121016.002759anon_803524693No ratings yet
- Running Head: Mental Illness As A Cause of Homelessness 1Document12 pagesRunning Head: Mental Illness As A Cause of Homelessness 1api-286680238No ratings yet
- Liberty Quarry DeniedDocument33 pagesLiberty Quarry DeniedThe Press-Enterprise / pressenterprise.comNo ratings yet
- Echinacea: Research ArticleDocument10 pagesEchinacea: Research Articlenadin nNo ratings yet