REVIEW ARTICLE
Sensory Neurons, Ion Channels,
Inflammation and the Onset of
Neuropathic Pain
Patrick L. Stemkowski, Peter A. Smith
ABSTRACT: Neuropathic pain often fails to respond to conventional pain management procedures.
here we review the aetiology of neuropathic pain as would result from peripheral neuropathy or injury.
We show that inflammatory mediators released from damaged nerves and tissue are responsible for
triggering ectopic activity in primary afferents and that this, in turn, provokes increased spinal cord
activity and the development of ‘central sensitization’. Although evidence is mounting to support the role
of interleukin-1β, prostaglandins and other cytokines in the onset of neuropathic pain, the clinical
efficacy of drugs which antagonize or prevent the actions of these mediators is yet to be determined.
basic science findings do, however, support the use of pre-emptive analgesia during procedures which
involve nerve manipulation and the use of anti-inflammatory steroids as soon as possible following
traumatic nerve injury.
RÉSUMÉ: Neurones sensitifs, canaux ioniques, inflammation et début de la douleur neuropathique. il arrive
fréquemment que la douleur neuropathique ne réponde pas au traitement conventionnel de la douleur. Nous revoyons
l'étiologie de la douleur neuropathique résultant d'une neuropathie périphérique ou d'une blessure. Nous démontrons
que les médiateurs de l'inflammation libérés au niveau des nerfs et des tissus lésés sont responsables du
déclenchement d'une activité ectopique dans les afférents primaires et que ceci provoque une augmentation de
l'activité au niveau de la moelle épinière et entraîne une « sensibilisation centrale ». bien qu'il existe de plus en plus
de données en faveur du rôle de l'interleukine-1 β, des prostaglandines et d'autres cytokines lors du début de la
douleur neuropathique, l'efficacité clinique des médicaments qui sont des antagonistes ou qui préviennent l'action de
ces médiateurs demeure à déterminer. les observations faites en sciences fondamentales sont en faveur de
l'utilisation de l'analgésie prophylactique pendant les interventions où il y a manipulation de nerfs et de l'utilisation
de stéroïdes anti-inflammatoires le plus tôt possible après une lésion nerveuse traumatique.
Can J Neurol Sci. 2012; 39: 416-435
The biology of pain
Pain can be defined as ‘an unpleasant sensory and emotional
experience associated with actual or potential tissue damage, or
described in terms of such damage’1. Pain minimizes contact
with the injurious stimulus; thus, promoting a protective
response2. This evokes both a reflex withdrawal from the
stimulus and complex behavioural strategies to avoid further
contact with such stimuli3. despite the unpleasant nature of pain,
it would be difficult to imagine any organism surviving without
it. For instance, what would motivate an organism to limit use of
an injured limb and allow healing? how would an organism
learn from its surrounding environment? Cox and colleagues
studied several families from Northern Pakistan that contained
members with a congenital inability to experience pain and
illustrated the following: “The index case was a ten-year-old
child, well known to the medical service after regularly
performing ‘street theatre’. he placed knives through his arms
and walked on burning coals, but experienced no pain. he died
416
before being seen on his fourteenth birthday, after jumping off a
house roof”4. Clearly, without the protection afforded by the pain
response, survival is compromised. So long as pain reflects an
injury, in space and time, then the benefits of pain outweigh
costs.
An important consideration, from the above definition, is that
pain has sensory and emotional (affective) dimensions. The
sensory dimension corresponds to nociception which is defined
as the neural process of encoding and processing noxious or
harmful stimuli5. Through this process, the nature (chemical,
mechanical or thermal), location, intensity and temporal aspects
From the Centre for Neuroscience, University of Alberta, Edmonton Alberta, Canada.
RECEivEd OCTObER 14, 2011. FiNAl REviSiONS SUbmiTTEd mARCh 1, 2012.
Correspondence to: Peter A Smith, Centre for Neuroscience and department of
Pharmacology, 9-75 medical Sciences building, University of Alberta, Edmonton,
Alberta, T6G 2h7, Canada. Email: peter.a.smith@ualberta.ca
�lE JOURNAl CANAdiEN dES SCiENCES NEUROlOGiqUES
of the stimulus are communicated to the higher centres6.
Although this specialized detection system usually initiates pain,
it is not synonymous with pain, as this is a conscious experience
that can occur in the absence of nociception5. For example, poststroke pain can be independent of peripheral nociceptor
activation7. The affective dimension is the moment-by-moment
unpleasantness of pain, made up of emotional feelings associated
with future implications, including distress, fear and suffering8.
These concerns are the result of pain-related activity in limbic
structures, such as the amygdala which elicits complex
behaviours leading to escape and avoidance8.
The affective dimension suggests psychosocial aspects can
influence the perception of pain such that ‘pain is whatever the
person says it is’9. Therefore, what is painful, yet tolerable to one
individual or in one circumstance, can be unbearable to or in
another. For instance, Rainville and colleagues demonstrated
that hypnosis can manipulate the unpleasantness of a given
noxious stimulus to individual human subjects10. Further, while
somatosensory regions of the brain always became active in
response to the noxious stimulus, activity in affective regions
varied with the degree of unpleasantness10,11.
Relative to the physiological contribution of nociception to
the pain experience, psychosocial aspects have been poorly
addressed in pain research. This disparity is, in part, a
consequence of animal models and measures of pain
behaviour12. While reflexive measures, such as paw withdrawal,
provide quantitative meaning to nociception, they suggest little
about the psychological state of the animal and, thus, underrepresent the pain experience8. Until recently, measures which
include the monitoring of pain affect, such as conditioned place
aversion (CPA), have been uncommon13. The focus on
nociception in pain research has been associated with the clinical
failure of several potential pain medicines12. Thus, an
understanding of both sensory and affective dimensions of pain
may improve translational research.
Pain in the clinic
Pain can result in hyperalgesia, allodynia and spontaneous
pain. These symptoms are the consequence of a heightened state
of sensitivity in response to tissue damage. The iASP
(international Association for the Study of Pain) defines
hyperalgesia as ‘an increased response to a stimulus which is
normally painful’. it is thought that hyperalgesia is the
consequence of sensitized nociceptive nerve endings and,
therefore, stimulus modality is harmful and response is painful14.
in contrast, allodynia is defined as ‘pain due to a stimulus which
does not normally provoke pain’ (iASP). Allodynia is generated
by a different mechanism than hyperalgesia, where the original
stimulus modality is non-harmful but the response has become
painful. Therefore, the ‘quality’ of the sensation has changed.
For example, allodynia is observed in patients with lesions of the
nervous system where touch, light pressure, or moderate cold or
warmth evokes pain when applied to apparently normal skin.
The term allodynia is, thus, reserved for situations where it is
known that the stimulus is incapable of activating nociceptors14.
Chronic pain resulting from tissue injury is often associated with
paroxysmal spontaneous pain12. Unlike allodynia and
hyperalgesia, spontaneous pain is non-evoked and is the most
universal clinical symptom in chronic pain states, such as
Volume 39, No. 4 – July 2012
neuropathic pain15. in addition, spontaneous pain appears to be a
much better predictor of ‘average’ and ‘worst’ pain ratings than
evoked pain hypersensitivities15. Paradoxically, research has
focussed on behavioural measures of hyperalgesia and allodynia
in chronic pain animal models. For instance, in a ten year period,
90% of the papers published in Pain reported evoked
hypersensitivity data, whereas the remaining 10% reported
spontaneous behaviour measurements16. This reluctance has
been attributed to the uncertainty of animal behaviours
corresponding to spontaneous pain and, therefore, represents
another important challenge in translational pain research12.
Nociceptive pain is limited in duration, lasting long enough to
signal the presence of a noxious stimulus. in response to tissue
damage, the protective function of pain is further enhanced by
allodynia and hyperalgesia3. inflammation is critical to this
process, whereby, a complex cascade of events (discussed
below) leads to the activation and sensitization of sensory nerve
fibres17. This heightened state of sensitivity subsides in the
absence of further tissue damage and once the wound has
healed3.
Pain symptoms persisting long after an initial insult suggest
that the pain response has become maladaptive and, thus, can be
considered a disease14. These chronic pain states can be
neuropathic or inflammatory in aetiology12,14. The iASP defines
neuropathic pain as ‘pain caused by a lesion or disease of the
somatosensory nervous system’. This definition encompasses
the observation that neuropathic pain can be triggered by a wide
variety of insults. These include direct nerve and spinal cord
trauma; viral infections including Herpes zoster and hiv; or
metabolic diseases including diabetes18. Chronic inflammatory
pain is thought to be the consequence of an underlying
inflammatory disorder related to tissue pathology such as
arthritis, gastritis, colitis or dermatitis19. Chronic inflammatory
pain is also associated with post traumatic and repetitive strain
injuries. Although distinct differences between neuropathic and
chronic inflammatory pain states have been reported, including
neurochemical changes and responses to analgesics20, both pain
states are thought to involve nervous system plasticity3. Further
understanding of these pain states at a molecular and cellular
level, as well as how they relate to one another is, therefore,
required. The present review focuses on cutaneous sensory
neurons, our understanding of the pathophysiological changes
that occur in them following injury and how these changes may
lead to the onset of chronic pain.
Primary afferent fibres and Dorsal Root Ganglion neurons
Primary afferent fibres are classified according to size, extent
of myelination, conduction velocity and neurochemical
phenotype. Conduction velocity is positively correlated with
fibre cross-sectional diameter21. large diameter A-fibres are the
most rapidly conducting, whereas, small diameter C-fibres are
the slowest conducting. The A-fibres are myelinated and have
readily definable subgroups. From fastest to slowest, the A-fibre
subgroups have been designated the Greek letters: α, β and δ.
There is considerable variability in conduction velocity between
species and even between nerves of the same species21.
however, it is known that mammalian A-fibres can conduct up
to 100 m/s while C-fibres conduct at <1m/s22. The majority of
afferents that transmit painful information are Aδ or C, while the
417
�ThE CANAdiAN JOURNAl OF NEUROlOGiCAl SCiENCES
majority of afferents that convey innocuous thermal or
mechanical information are Aβ−fibres. however, thinly
myelinated and, possibly, some unmyelinated small afferents are
associated with the transmission of innocuous sensations23,24. For
instance, a woman with selective loss of large diameter,
myelinated sensory fibres provided an opportunity to study C-
fibres in isolation24. in this particular case, light touch to the back
of the hand was felt as very diffuse and faint, yet pleasant. Thus,
some C-fibres may be associated with sensations resulting from
innocuous stimuli.
Figure: Diagram illustrating cutaneous sensory neuron subpopulations identified according to AP waveform, morphology, neurochemistry and targetderived neurotrophic support. A. Large Aβ-neurons have short AP durations with no shoulder on the repolarization phase, large cell body diameters (>
40 μm) with thickly myelinated axons and are dependent on target-derived NT-3. B. Medium Aδ-neurons have intermediate AP durations with the
presence of a shoulder on the repolarization phase, intermediate cell body diameters (30-40 μm) with thinly myelinated axons and express TRPV1
channels. C. Small C-neurons have long AP durations with the presence of a shoulder on the repolarization phase and small cell body diameters (< 30
μm) with unmyelinated axons. Small neurons can be further subdivided into i) IB4-positive which express the P2X3 receptor and are dependent targetderived GDNF; and ii) IB4-negative which express neuropeptides, such as SP and CGRP and are dependent on target-derived NGF. Both IB4-positive
and –negative small neurons express TRPV1 channels. All AP waveforms were elicited in response to 2 ms depolarizing current pulses of appropriate
suprathreshold magnitude26. Calibration in A. (40 mV, 5 ms) refers to all AP waveforms. AP = Action potential; SP = Substance P; GDNF = Glial;
Derived Neurotrophic Factor; NGF = Nerve Growth Factor; TRPV1 = Vanilloid Receptor Type 1
418
�lE JOURNAl CANAdiEN dES SCiENCES NEUROlOGiqUES
Morphology and Neurochemistry
Fibre diameter is also positively correlated to cell body
diameter and, therefore, Aβ-fibres are associated with the largest
cell body diameters, typically greater than 40 μm, whereas, Aδ−
and C-fibres are associated with medium (30-40 μm) and small
(< 30 μm) sized cell bodies, respectively25 [Figure].
Small, cutaneous dorsal root ganglion (dRG) neurons can be
divided into peptidergic and non-peptidergic subpopulations27.
The peptidergic neurons express substance P (SP) and calcitonin
gene-related peptide (CGRP), while the non-peptidergic Cneurons express a binding site for the α-d-galactose-specific
Griffonia (or Bandeiraea) simplicifolia ib4 (GSA-ib4) plant
lectin28. These ib4-positive rat dRG neurons frequently express
adenosine triphosphate-activated purinergic P2X3 receptors29
[Figure]. This serves as another defining neurochemical and,
perhaps, functional feature of non-peptidergic small dRG
neurons. On the other hand, immunoreactivity for CGRP is
commonly used to define peptidergic, small sensory neurons
since CGRP reactivity (40% of all sensory neurons) includes SP
populations (20% of all sensory neurons), as well as other, SP
exclusive, sensory neurons populations, such as somatostatin
(SOm) expressing dRG neurons30-32. in dRG, vanilloid receptor
1 (TRPv1) immunoreactivity is restricted to small- and mediumsized neurons with reactivity in both peptidergic and nonpeptidergic sensory neurons33,34 [Figure]. Since TRPv1 is a
transducer of noxious thermal stimuli, its presence is commonly
used to distinguish nociceptive sensory neurons from, presumed,
non-nociceptive neurons.
it is also important to consider that, while many of these cell
surface and cytoplasmic molecules are useful as markers of
phenotypes associated with distinct sensory neuron subpopulations, their presence varies between species, between
innervated tissues, with animal age and after tissue injury35-37.
Neurotrophic support
Neurotrophic factors of the nerve growth factor (NGF) family
exert biological responses by binding to their respective high
affinity receptors: tropomyosin receptor kinase A (TrkA), Trkb
and TrkC38. Additionally, all neurotrophins are capable of
binding the p75 receptor which belongs to the tumor necrosis
factor receptor (TNFR) family. in the adult nervous system,
sensory neurons remain responsive to neurotrophic factors and
the presence of several target-derived neurotrophins has been
associated with the maintenance of differentiated sensory neuron
phenotypes39. For instance, peptidergic and non-peptidergic
adult dRG neurons differ in neurotrophic support: the nerve
growth factor (NGF) dependent and the glial cell line-derived
neurotrophic factor (GdNF) dependent neurons, respectively
36,40,41
[Figure]. Consistent with neurotrophin dependence,
peptidergic neurons express TrkA, whereas the non-peptidergic
express receptor components for GdNF signalling, including the
GdNF family receptor alpha-1 (GFRα-1) and the
transmembrane tyrosine kinase receptor, rearranged during
tranfection (RET) receptor36,41,42. Upon removal of NGF or
GdNF, respective cultured sensory neuron subpopulations are
diminished or phenotypically switched43. The NGF-dependent
population (CGRP-positive) represents roughly 40% of dRG
neurons, whereas the GdNF-dependent population (ib4positive) represents roughly 30%28,40 with minimal overlap
Volume 39, No. 4 – July 2012
between the two populations. Further, the lack of behavioural
responses to nociceptive stimuli in NGF and trkA null mutant
mice is in agreement with the hypothesis that most TrkA neurons
convey nociceptive information44. more recently, the role of Ret
signalling in the postnatal development of sensory neurons has
been analyzed in mice carrying a specific deletion of the Ret
gene in dRG neurons45,46. The phenotype of this conditional
knockout has indicated that Ret signalling is not required for
dRG neuron survival, but is necessary for the proper
differentiation of the non-peptidergic nociceptive subtype, as it
appears to promote the expression of several markers that are
characteristic of these sensory neurons and to support the normal
extent of their peripheral projections in the skin45.
Another member of the neurotrophin family, neurotrophin-3
(NT-3), also interacts with mature sensory neurons. in cutaneous
afferents, mRNA for the NT-3 receptor, TrkC, is detected in
larger sized adult sensory neurons which show little size overlap
with neurons expressing TrkA47. Further, in situ hybridization
reveals that TrkC has minimal co-localization with TrkA
expressing adult rat dRG48. Thus, NT-3 responsive neurons may
be functionally distinct from NGF responsive neurons. in
support, single unit recordings from mice with null mutations of
the NT-3 gene indicated that two mechanoreceptive subsets of
cutaneous afferents require this factor: d-hair receptors and
slowly adapting mechanoreceptors, while other cutaneous
receptors were unaffected49. in adult NT-3 heterozygous
animals, slowly adapting afferents had the greatest reduction in
incidence with corresponding morphological losses of Aβ-fibre
axons. merkel cells, which are the end organs of slowly adapting
mechanoreceptors, were severely reduced. This loss of merkel
cells, together with their innervating Aβ-fibres, happens in the
first postnatal weeks of life, in contrast to muscle spindles and
afferents which are never formed in the absence of NT-3. Thus,
NT-3 is essential for the maintenance, but not the establishment,
of specific cutaneous afferents known to sub serve fine tactile
discrimination in humans.
in summary, the dependence of sensory neurons on
neurotrophic factors is dynamic, altering with nervous system
development and after tissue injury. in addition, sensory neuron
responsiveness may be dependent on target tissue, sensory
ganglia (dRG or trigeminal ganglia), species and the presence of
one or multiple neurotrophic factor receptors, including p75 coexpression. despite these complexities, it can be suggested that
mechanoreceptive populations tend to depend on NT-3, whereas,
nociceptive populations tend to depend on NGF and GdNF. in
addition, the Trkb ligand, brain derived neurotrophic factor, is
likely involved in the maintenance of several sensory neuron
populations.
Mechanisms of sensory transduction
Cutaneous sensory neurons can be further classified
according to sensory modality. For example, thermoreceptors
respond to warming or cooling, whereas mechanoreceptors
respond to stretch, pressure and hair movement. in addition,
many nociceptors are polymodal and respond to a variety of
harmful stimuli. The transduction of stimulus modality into
action potentials involves a variety of complex cellular and
molecular processes50.
Over the past decade, the molecular correlates of sensory
transduction, whose activities depend on specific stimuli in the
419
�ThE CANAdiAN JOURNAl OF NEUROlOGiCAl SCiENCES
surrounding environment, have been identified51. Cation
channels, known as transient receptor potential (TRP) channels,
represent the first illustration that sensory ion channels can be
gated by a physical stimulus33,52. These channels are divided into
seven subfamilies, have six transmembrane domains, a pore
region, cytoplasmic amino and carboxy termini and arrange as
functional tetramers53. members of three families, the vanilloid
TRP channels (TRPv), the melastatin or long TRP channels
(TRPm), and the ankyrin transmembrane protein channels
(TRPA) are of particular interest as thermoreceptors54. in
mammals, temperature sensitive TRPs are each tuned to distinct
temperature ranges and, collectively, permit discrimination of
temperature ranging from noxious cold to noxious heat50. Four
TRP channels belonging to the TRPv subfamily are activated by
heating, with characteristic activation temperatures ranging from
warm temperatures (> 25°C for TRPv4; >31°C for TRPv3), to
heat (> 43°C for TRPv1) and noxious heat (> 52°C for
TRPv2)51. in contrast, TRPm8 and TRPA1 are activated by
cooling, (< 28°C for TRPm8; <18°C for TRPA1).
many thermal TRPs are also chemo-, mechano- and /or osmosensitive. For instance, TRPv1 responds to protons and
capsaicin, the pungent component of spicy peppers33,55. in
contrast, TRPm8 is activated by menthol, while TRPA1
responds to a variety of pungent compounds, including
cinnamaldehyde (cinnamon), allicin (garlic) and isothiocyanates
(wasabi)56,57. TRPA1 and TRPv4 have been associated with
mechanosensitivity58,59. in addition, TRPv4 mediates animal
behaviours in response to hypotonic stimuli and maybe of
particular interest in hypersensitive states60.
There are many other possible molecular correlates for
sensory neuron transduction. For example, two pore potassium
channels, such as TREK-1, close upon cooling and may allow
depolarization of cold-sensitive neurons61,62. Additionally,
TREK-1 channels are stretch-sensitive and TREK-1 knockout
mice have increased sensitivity to low-threshold mechanical
stimuli61,63. Acid sensing ion channels (ASiCs) respond to
protons and membrane stretch, however, a role in
mechanoception has been unsubstantiated with animal models64.
Several other molecules may be involved in sensory neuron
transduction, including canonical-1 TRP channels (TRPC1),
P2X3 ATP-gated cation channels, protease activated receptors
(PAR 1, 2 and 4) and voltage-gated channels (vGCs), including
voltage-gated sodium channels (vGSCs)50,52,65,66.
Taken together, the diverse sensory modalities of primary
afferents may be associated with the expression pattern of
transduction molecules, such as TRP channels, in cutaneous
tissues. For instance, noxious heat sensations could be explained
by the high expression of TRPv1 and TRPv2 in nociceptive
Aδ− and C-fibres50,55. Though TRPm8 and TRPA1 are both
expressed in small diameter sensory neurons, only TRPA1
expression co-localizes with putative nociceptive neuron
markers, such as SP and CGRP, thereby, rationalizing noxious
cold as distinct from cool thermo-sensations52. Consistent with
polymodal nociceptors, TRPA1 is expressed in a subset of
TRPv1 expressing nociceptive neurons responding to noxious
mechanical and thermal stimuli52. The close apposition between
free nerve endings (FNEs) and keratinocytes, as well as the
synaptic junctions between merkel cells and Aβ−fibres suggest
skin cells can act as first-line transducers of physical stimuli50. in
support, merkel cells express TRPv4 and keratinocytes express
420
TRPv3 and TRPv450,52. in a manner analogous to auditory and
taste transduction, skin cells could respond to innocuous heat
and mechanical stimuli and, then, chemically transmit the signal
to sensory neurons, such as Aβ−fibres50.
Peripheral connections
Sensory neuron connectivity, both peripherally and centrally,
is vital to the discriminative task of the somatosensory system.
Within the skin, there are several morphologically distinct nerve
endings which can be classified according to afferent threshold,
adaptation and, ultimately, sensory modality. For instance,
physiological and cytological examination of the hairy skin in
cats showed that free nerve endings (FNEs) are the nerve
terminals of Aδ- and C-fibres, sub serving the modalities of pain
and temperature67. The Aδ−fibres pass through the papillary
dermis and penetrate the basement epidermal layer where they
lose their myelin sheath, while peptidergic and non-peptidergic
C-fibres terminate in different epidermal layers of glabrous and
hairy skin50,67. many FNEs are considered nociceptors. Certain
nociceptors, whose afferent conduction velocities correspond to
Aδ− and C-fibres, are high threshold mechanoreceptors and
respond vigorously to only intense (tissue damaging) mechanical
stimuli68,69. Other nociceptors are polymodal, whose afferent
conduction velocities are reflective of C-fibres, and respond
vigorously to noxious mechanical and thermal stimuli and to
chemical substances relevant to tissue damage68,69. Still, some
nociceptors, in deep subcutaneous tissue, have such high
thresholds that they are unresponsive or “silent” in acute events,
but become active after chronic tissue damage69-71. FNEs of Aδand C-fibres have also been associated with innocuous stimuli
where some are considered thermoreceptors or low threshold
mechanoreceptors69,72-74. As noted above, evidence is
accumulating that many of the FNEs form en passant synapses
with epidermal cells, such as keratinocytes, which express
molecular correlates for stimulus transduction50,75. Thus, FNEs
may not always be the first-line transducers of pain and
temperature.
Sensory corpuscles are capsulated low threshold
mechanoreceptors formed by a central axon surrounded by
variably arranged differentiated Schwann cell-related and
perineurial-derived cells72,76. Two main subtypes of sensory
corpuscles can be considered: the extensively capsulated,
Pacinian corpuscles and the poorly capsulated, meissner
corpuscles. meissner corpuscles lie just beneath the epidermis,
while Pacinian corpuscles reside in the dermis and deeper tissues
and, in both cases, the capsulated arrangements appears to act as
a filter that protects the sensory endings from irrelevant
stimuli77. Corpuscles can have Aα-, Aβ- or Aδ-sensory nerve
fibres and upon static, mechanical skin displacement, only a few
action potentials are recorded from sensory units and, therefore,
corpuscle are defined as rapidly adapting77. however, adaptation
terminology is misleading since static displacement does not
account for derivatives of displacement, such as velocity and
direction21. Thus, many rapidly adapting mechanoreceptors do
not adapt rapidly when presented their most effective stimulus,
such as dynamic mechanical displacements. Therefore, Pacinian
and meissner corpuscles are vibration detectors which are
ideally tuned to detect high (> 100 hz) and low (< 100 hz)
dynamic displacements, respectively77.
�lE JOURNAl CANAdiEN dES SCiENCES NEUROlOGiqUES
The Ruffini endings and merkel cell–neurite complexes are
slow adapting, low threshold mechanoreceptors of glabrous- and
hairy skin21,77. Ruffini endings are located in the connective
tissue of the dermis and are relatively large spindle shaped
structure tied into the local collagen matrix77. Ruffini ending
structure is considered analogous to that of the Golgi tendon
organ in muscle and, therefore, suggests that Ruffini endings
function as stretch receptors72. Αα/β sensory axons branch
between the fibrils and stretching of the skin tightens the fibrils
which, in turn, leads to deformation and depolarization of the
axonal ramifications21,78. The merkel cell is a special cell type
in the basal layer of the epidermis that enfolds the unmyelinated
ending of the Αα/β afferent fibre21,77. The merkel cell–neurite
complex is selectively sensitive to a particular component of
local displacement which makes it sensitive to edges, corners
and curvature. however, it is not known whether this selectivity
is due to the merkel cell or to the transducer mechanism within
the afferent terminal79.
hairs are additional low threshold mechanoreceptors of hairy
skin and have two main types of follicles72: 1) Guard hairs have
thick diameter shafts, such as that found on the human scalp or
outer coat of furred mammals. 2) vellus hairs have thin diameter
shafts, such as that found on the human eyelid or the down hairs
of furred animals. Aα−, Αβ− or Aδ−nerve fibre endings wrap
around the hair follicle, collectively termed the piloneural
complex and become activated upon the slightest bending of the
hair50,72,74. Ultrastructural analysis has revealed that axons
innervate from the base of guard- and vellus-hair follicles and
split into fork-like projections known as lanceolate terminals.
Further, lanceolate terminals have been associated with rapidly
adapting afferents and, thereby, enable hairs with movement
detecting capabilities21,72.
Electrophysiology
The electrical properties of dRG neurons correlate to
receptor- and afferent-type and, ultimately, to sensory function.
intracellular recordings from somata in intact, but isolated, adult
mouse dRG led to discovery of three distinct cell types on the
basis of action potential (AP) shape, sensitivity to tetrodotoxin
(TTX) and ionic dependence: 1) ‘fast’ (F) -neurons, exhibiting
brief APs which were mediated by TTX-sensitive (TTX-S) Na+
channels; 2) ‘afterhyperpolarization’ (A) -neurons, exhibiting
large and prolonged afterhyperpolarzations (AhPs) which were
dependent on TTX-resistant (TTX-R) Na+ channels; and 3)
‘hump’ (h) -neurons, exhibiting broader spikes that were
mediated by TTX-R Na+ and Ca2+ channels with the latter
producing a characteristic ‘hump’or shoulder on the descending
limb of the AP80-82. Similar AP shapes were reported in other
studies where broad somatic APs tend to have slow C–, as well
as some fast Aβ−conducting fibres, while narrow APs tend to
have faster conducting fibres, including Aα−, Aβ− and
Aδ−fibres [Figure]26,83,84. in addition, broad somatic APs from
C– and some Aδ-neurons are often associated with a shoulder on
the repolarization phase [Figure]. Studies in intact preparations,
where the peripheral receptor could also be characterized, have
associated sensory function with the heterogeneous electrical
properties of dRG somatic membranes82,85-87. The major trend is
that somatic spikes in nociceptors are characterized by broad
APs with shoulders on the descending limb, while receptors
Volume 39, No. 4 – July 2012
responding to innocuous stimuli are characterized by narrower
spikes. it was also discovered that Aδ−fibres innervating high
threshold mechanoreceptors (hTmRs) exhibit broader APs than
Aδ−fibres innervating d-hairs82,86. Aβ hTmRs differ from Aβ
low threshold mechanoreceptors (lTmRs) in the same general
way, however, Aβ lTmRs supplying different receptor types
(e.g., slowly adapting type i, Pacinian corpuscles, etc.) exhibit
no correlation between receptor type and electrophysiology of
the soma. The relationship between AP shape and receptor
threshold in C-fibres appears to be species dependent. For
instance, C-fibre AP duration is longer for high threshold
(nociceptive) afferents than for low threshold afferents in rat and
guinea pig88,89, however, no such relationship was found in
cats90. Taken together, the variability of AP shapes in A-fibres
and, possibly, C-fibres suggests AP duration is more related to
receptor threshold than to conduction velocity.
The differential ionic dependencies and TTX sensitivities of
APs reflect non-uniform ion channel expression among dRG
cell types. Through several electrophysiological, pharmacological and molecular studies, it is now known that dRG
neurons are host to a variety of voltage-gated ion channels91.
Voltage gated sodium channels (VGSC)s are heteromultimeric proteins consisting of a large pore-forming α-subunit
and small extracellular accessory β-subunits which modulate
channel membrane insertion and channel gating92. Nine
mammalian sodium channel isoforms have been identified and
functionally expressed93. TTX-S isoforms include Nav1.1,
Nav1.2, Nav1.3, Nav1.4, Nav1.6 and Nav1.7, whereas, TTX-R
isoforms include Nav1.5, Nav1.8 (formerly peripheral nerve
sodium channel type 3 (PN3) and sensory neuron specific
(SNS)) and Nav1.9 (formerly novel voltage-gated Na+ channel
(NaN))92,94,95.
variations in sodium current properties in dRG neurons are
associated with a heterogeneous sodium channel population.
For instance, electrophysiological studies in dRG somata have
demonstrated the presence of kinetically slow TTX-R sodium
current in small, but not large-sized neurons96,97. Cloning studies
identified sodium channel α-subunits Nav1.8 and Nav1.9 which
produce TTX-R currents when heterologously expressed98-100.
Further, in situ hybridization has revealed that transcripts for the
two TTX-R sodium channels are preferentially expressed in
small diameter sensory neurons which include nociceptive (Ctype) neurons. Waxman’s group demonstrated differential
maintenance of the two dRG TTX-R isoforms, where Nav1.9 is
preferentially expressed in small ib4-positive dRG neurons
while both small ib4-positive and -negative neurons express
Nav1.843. The differential expression was also associated with
alterations in sodium channel properties expected to influence
excitability, such as a hyperpolarized voltage-dependence of
activation and inactivation in ib4-positive neurons. The
persistent nature of currents mediated via Nav1.9 was further
predicted to underscore the longer AP durations observed in
small ib4-positive neurons89. in a similar manner, many other
isoforms have been characterized each with unique biophysical
properties that influence AP generation, such as the ‘rapidly
repriming’, resurgent Nav1.6 sodium current. This current, by
virtue of its rapid recovery from inactivation, can maintain high
frequency firing101. heterogeneous expression of vGSC
isoforms thus tunes electrical behaviour in the various sensory
421
�ThE CANAdiAN JOURNAl OF NEUROlOGiCAl SCiENCES
neuron subpopulations and their altered expression or
modulation by mediators may be of consequence after tissue
damage101-103.
immunocytochemical methods have also been used to
determine the distribution of vGSC isoforms in sensory neurons
and it is now known that large dRG neurons predominantly
express TTX-S channels, such as Nav1.1, Nav1.6 and Nav1.7,
with some TTX-R Nav1.8 expression, while small neurons
express TTX-S channels, in conjunction with TTX-R Nav1.8 and
Nav1.9 channels101. These findings have been further
substantiated using intracellular recording, together with
immunohistochemistry, to show the distribution of channels in
dRG neurons that give rise to particular fibre types, such as the
association of nociceptive C-fibres and broad APs with ib4positive cell bodies immunoreactive for the Nav1.9 isoform89,101.
last, it is known that expression of multiple sodium channels,
including TTX-R vGSCs, is not limited to the cell body and
extends along the fibres, thereby, demonstrating the likely
importance of these channels in conduction and fibre
characteristics101.
voltage-gated calcium channels (vGCCs) are the critical link
between membrane depolarization and calcium entry and
represent of one of several ways calcium can influence
membrane excitability and physiological processes, including
neurotransmitter release104,105. biochemical characterization of
vGCCs has revealed a complex protein structure composed of
α1 pore forming subunit, encoded by gene subfamilies: Cav1 to
3104, as well as several auxillary subunits105,106.
Sensory neurons express several biophysically and
pharmacologically distinct vGCCs104. These include: 1) low
voltage activated (lvA) channels encoded by the gene subfamily
Cav3 which have ‘low’ gating thresholds from -60 to -50 mv
evoking rapidly inactivating ‘transient’ (T-type) currents, which
are sensitive to changes in holding potential and which are nonselectively inhibited by amiloride and Ni2+104,105,107. 2) high
voltage activated (hvA) channels encoded by gene subfamilies
Cav1 and 2 which have ‘high’ gating thresholds from -30 to -20
mv. Further, hvA Ca2+ currents include ‘long-lasting’ (l-type,
Cav1) currents, ‘Purkinje cell’ (P/q-type, Cav2.1) currents and
‘neuronal’ (N-type, Cav2.2) currents which are sensitive to
blockade by dihydropyridines, omega-agatoxin ivA and by
omega-conotoxin GviA, respectively104,105,107-109. 3) last, there
are the intermediate voltage activated calcium channels which
have ‘intermediate’ gating thresholds, evoking currents that are
‘resistant’ (R-type, Cav2.3) to most toxins.
While N-type currents are equally proportionate in small,
medium and large neurons, T-type currents have their greatest
proportion in medium neurons and l-type currents have their
greatest contribution in small neurons107,110-112. The lvA and
hvA channels are associated with different physiological roles.
N-type vGCCs are highly expressed at presynaptic nerve
terminals where they are involved in fast synaptic
transmission113. in contrast, T-type vGCCs are expressed in cell
bodies and nerve endings of afferent fibres where they partake in
regulating neuronal excitability by contributing to the initiation
of repetitive discharge113,114. Further, the unique biophysical
properties attributed to T-type vGCCs lower AP threshold,
promote bursting activity and generate subthreshold membrane
oscillations.
422
As well as their pore forming α subunits, vGCCs contain
various accessory subunits. The α2-δ subunit, which has
particular relevance to neuropathic pain mechanisms, is thought
to be involved in the trafficking of channels to the plasma
membrane115. it is upregulated by nerve injury116-119 and appears
to be the primary site of action for the antiallodynic agents
pregabalin120 and gabapentin121-123.
Potassium channels are the most diverse class of ion channels
owing to numerous encoding genes, alternative mRNA splicing,
α-subunit assemblies into dimeric or tetrameric channels, as well
as associations with β-subunits124. The variation in AhP
duration, observed by matsuda and colleagues, suggests that
potassium conductances are another defining feature among
sensory neurons80. it is now known that dRG neurons contain a
wide variety of potassium channels of all four families: voltagegated (Kv), calcium-activated (KCa), inwardly-rectifying (KiR)
and two-pore (K2P) channels. Although all four families have
been associated with pain hypersensitivity 125, Kv and KCa
channels and their relation to sensory neuron physiology will be
the topic of further discussion. For more information on KiR and
K2P, see reference numbers125-128.
Kv and KCa channels exist as tetramers composed of four pore
forming α-subunits either alone or in association with regulatory
β-subunits129,130. The voltage-dependent delayed rectifier and
fast transient potassium currents were first described in dRG
neurons by Kostyuk’s group131. The delayed rectifier current was
characterized by its slow activation kinetics and lack of
inactivation during maintained membrane depolarization. in
contrast, the fast transient current or A-current (IA) had,
relatively, ‘fast’ activation kinetics and was almost completely
inactivated at -50 mv. in addition, the fast transient current
required a relatively small depolarization for activation when
compared to the delayed rectifier current. Though both can be
blocked by tetraethylammonium (TEA), fast transient potassium
currents are also susceptible to block by 4-aminopyridine (4AP)132,133. The existence of delayed rectifier and fast transient
potassium currents in dRG neurons was confirmed in
subsequent studies. however, a third component was identified
based on sensitivity to the Eastern green mamba venom,
dendrotoxin, and greater susceptibility (<100 micromolar),
relative to IA (>100 micromolar), to 4-AP block134,135. When
isolated, the dendrotoxin-sensitive current (Id) was calcium
insensitive and displayed, relative to IA, slow, incomplete
inactivation135,136. biophysically, potassium currents could be
divided into non-inactivating and transient A-currents with the
later subdivided divided into fast (IAf) and slow (IAs) components
where IAf had, relatively, faster kinetics and more negative
voltage dependencies than IAs137. Thus, pharmacological and
biophysical studies agree that at least three voltage-gated
potassium currents can be readily identified in sensory neurons:
sustained or non-inactivating, IA or IAf and Id or IAs (but see also
reference number138).
There is a complex distribution of the voltage-gated
potassium currents among sensory neurons. While most sensory
cell types have a non-inactivating or sustained potassium
current, the distribution of transient components is less
understood. For instance, A-type currents have been identified
in subpopulations of large and small sensory neurons, including
those associated with mechanoreceptors and nociceptors,
�lE JOURNAl CANAdiEN dES SCiENCES NEUROlOGiqUES
respectively138-141. in contrast, villiere and colleagues reported
that the proportion of neurons with A-type current is greatest in
C-fibres and least in Aα/β-fibres142. Under thorough
pharmacological and biophysical analysis, Gold and colleagues
characterized six voltage-gated potassium currents in rat dRG
neurons, three transient and three sustained, and found that there
is differential distribution among rat dRG neuron subpopulations138. Thus, it remains possible that most sensory cell
types have at least one transient and one sustained current.
Regardless of the sensory cell type, most studies agree sustained
potassium currents shape APs, while transient currents are
involved in the latency of firing, low firing frequency, spike
adaptation and that there may be an inverse relationship in the
proportion of these two broad classes of potassium current in any
given sensory cell137,139,141,143,144.
Three classes of KCa channels can be distinguished on the
basis of their biophysical and pharmacological properties104.
large conductance bKCa channels are voltage-gated and
sensitive to iberiotoxin, while small conductance (SKCa) and
intermediate conductance (iKCa) channels are voltage-insensitive
and can be blocked by apamin and clotrimazole, respectively.
modulation of KCa channels allows alterations in intracellular
calcium concentration to regulate membrane excitability,
whereby, the three KCa channels are thought to have distinct
functional roles. For instance, bKCa channels are involved in AP
repolarization and generation of the fast AhP (fast IAhP),
whereas, SKCa channels convey the IAhP that mediates slow
AhPs in small nociceptive dRG neurons104,145-147. in contrast,
the physiological role of iKCa in dRG neurons remains to be
determined. Although the functions of SKCa and bKCa channels
are well recognized in small diameter sensory neurons148,149, the
presence of SKCa channels in large diameter neurons150 suggests
that KCa channels have physiological importance in nonnociceptive neurons.
Hyperpolarization-activated cyclic nucleotide-gated cation
(HCN) channel subunits include four family members (hCN1-4)
that share substantial homology151,152. individual hCN subunits
assemble as homotetramers and, when expressed, homomers
differ in two main respects: 1) rates of activation are in the order
of hCN1>hCN2>hCN3>hCN4; and 2) hCN2 and 4 are
strongly modulated by adenosine 3’, 5’ –cyclic monophosphate
(cAmP) elevations which shifts the midpoint of activation in the
positive direction by 12 to 20 mv. heteromers may also form
functional hCN channels and have intermediate properties
which are related to subunit composition153,154.
The hCN channels give rise to hyperpolarization-activated,
non-selective cation current (Ih)155. The slow activation of Ih in
dRG neurons gives rise to a ‘voltage sag’ in response to
hyperpolarizing current commands155,156. Thus, the initial
voltage attained by injection of hyperpolarizing current
gradually abates during the course of the current command. Ih is
also involved in setting resting membrane potential, participating
in pacemaker activity and modulating synaptic activity157. hCN
channels 1 to 3, but likely not hCN4 (but see also reference
number158), are present in the somata and axons of dRG
neurons159-161. Further, hCN1 and fast Ih are predominately
found in larger dRG neurons, while slower Ih currents are more
variably expressed in small neurons160-162. last, knockout
mutations or block with Zd7288 are associated with suppression
Volume 39, No. 4 – July 2012
of sensory neuron hyperexcitability and pain-related behaviours
and, therefore, ih has attracted recent interest in pain research163.
Spinal projections
Once transduction has encoded information from various
stimuli in an organism’s environment, various levels of the
central nervous system (CNS) become involved in the
processing of this sensory information.
The initial stage for the central processing of pain occurs in
the dorsal horn of the spinal cord and involves specific spatial
terminations for primary afferents. For instance, the rostrocaudal and medio-lateral terminations of primary afferents
encode the location of their individual peripheral receptive
fields, thus, generating a somatotopic map of the body’s surface
onto the dorsal horn164. On the other hand, primary afferent
terminations in the dorso-ventral plane of the dorsal horn encode
different functional classes of sensory neurons. The dorsoventral plane of the dorsal horn is subdivided into six horizontal
laminae (li to lvi) where neurons of common morphological
features define each lamina165,166. The identities of primary
afferents that terminate and release glutamate within the
marginal layer (li), the substantia gelatinosa (lii), the nucleus
proprius (liii to liv) and lv have been determined. For
instance, large myelinated fibres, innervating low threshold
mechanoreceptors enter the cat spinal cord and send collaterals
into the dorsal horn as they ascend and, sometimes, descend the
dorsal column167-170. These collaterals terminate ipsilaterally in
laminae ventral to the outer lamina ii (liio) and include
extensive terminations in laminae iii and iv. Similar patterns of
termination occur in the rat dorsal horn171. in contrast, identified
C-fibres, including nociceptive and thermoreceptive fibres,
terminate ipsilaterally in laminae i, ii and v172,173. Further,
CGRP immunoreactivity revealed that peptidergic C-fibres,
many of which co-localize SP or SOm, terminate in laminae i,
iio and v, whereas, ib4 labelling and/or P2X3 immunoreactivity
has revealed that non-peptidergic C-fibres terminate dorsally
within inner lamina ii (liiid)29,174,175. Although both classes of
C-fibres transmit nociceptive information to the spinal cord, the
function of non-peptidergic C-fibres remains poorly
understood34. Nociceptive, high threshold mechanoreceptive
Aδ-fibres terminate ipsilaterally in laminae i and v, whereas
innocuous Aδ-fibres, innervating d-hairs, terminate ipsilaterally
in the deeper part of lamina ii and lamina iii176. Taken together,
the superficial layers of the dorsal horn (li and liio) receive
heavy nociceptive input, while deeper laminae, with the
exception of l5, receive non-nociceptive input.
Neuropathic pain
Neuropathic pain can be triggered by various insults
including direct nerve and spinal cord trauma; viral infections
including Herpes zoster and hiv; or metabolic diseases
including diabetes18. because the clinical presentation of
neuropathic pain is often independent of any obvious signs of
inflammation, it is sometimes described as ‘non-inflammatory
pain’.
in experimental animals, peripheral nerve damage, such as
nerve sectioning (axotomy) or chronic constriction, induce painrelated behaviours that are widely accepted as a model for
423
�ThE CANAdiAN JOURNAl OF NEUROlOGiCAl SCiENCES
human neuropathic pain. Such behaviours are associated with an
enduring increase in the excitability of primary afferent neurons
which, over a period of days or weeks, leads to the generation of
increased excitability and synaptic activity in second order
sensory neurons within the dorsal horn of the spinal cord. These
events correspond to the phenomenon of ‘central sensitization’
which is a major component of many persistant pain states3,177.
The generation of ectopic activity, thus, provides a theoretical
basis for the use of pre-emptive analgesia in surgery. however,
traditional analgesics, such as morphine, have limited use in the
treatment of neuropathic pain and, therefore, much effort has
been devoted to the understanding of how peripheral nerve
injury leads to increased excitability of the spinal dorsal horn.
Enduring increases in primary afferent activity as a trigger to
central sensitization
Experiments using various nerve injury animal models
suggest that the enduring increase in primary afferent activity
originates both from the neuroma178, that develops at the site of
nerve injury, and from sensory cell bodies in the dRG179,180.
dRG excitability increases two to seven weeks after
sectioning (axotomy) of the sciatic nerve26. Thus, the minimum
curent required to discharge an AP (rheobase) was reduced and
sustained depolarizing current evoked a higher frequency of AP
discharge. There were also increases in AP height and width.
voltage-clamp analysis supported these findings, as AP
generating mechanisms, such as TTX–R and/or TTX-S Na+
currents (INa), were increased102. in contrast, AP regulatory
mechanisms, such as steady state (delayed rectifier) K+ current
(IK) and hvA Ca2+-channel current (hvA-Iba) were
attenuated112. Further, alterations were most prevalent in the
small-sized dRG neurons which are, presumably, nociceptive Cand Aδ-fibres. however, with the onset of autotomy (self
mutilation), which is believed to be a behavioral manifestaion of
human neuropathic pain, changes became most substantial in the
large (Aβ) cell bodies26,102,112.
Other studies also reported changes in electrical properties of
dRG neurons after nerve injury that are consistent with
increased primary afferent activity. For instance, intracellular
recordings from neurons in intact dRG revealed that sacral 1
(S1) spinal nerve transection led to a significant reduction of the
rheobase in A- and C-cell types181. The reduction of rheobase in
A-cells was associated with a concomitant increase in apparent
input resistance near the resting membrane potential (RmP). by
contrast, the rheobase reduction in C-cells was associated with a
depolarizing shift of the RmP. in addition, nerve injury produced
significant action potential broadening in all cell types. in smallsized dRG neurons, axotomy reduced AP threshold, but was
without alterations to RmP or AP shape182. After CCi, isolated
small-, medium- and large-sized dRG neurons showed an
increased incidence of spontaneous AP activity which was
associated with a negative shift in AP threshold183. Similar
findings were reported after chronic compression of the dRG,
however, injury-induced changes were more apparent in largeand medium-sized neurons than in small neurons184. despite
differences in the experimental approach employed in these
studies, similarities do exist, including a reduction in firing
threshold or rheobase in nociceptive and, possibly, nonnociceptive sensory neurons. Further, distinct changes to AP and
424
AhP shape, as well as to passive membrane properties, suggest
alterations in the underlying availability of particular ion
channels may be asssociated with the sensory neuron subtype, as
well as the nature of the nerve injury.
Nerve injury-induced changes to the availability of sodium
channels. in contrast to the findings of Abdulla and Smith102
discussed above, Waxman and colleagues reported that axotomy
injury resulted in the down regulation of TTX-R sodium current
in small- and large-sized rat dRG neurons, leaving TTX-S
sodium currents to make a greater proportion of the total sodium
current in both cell populations185,186. Similar observations were
reported by Zhang and colleagues after an axotomy injury182.
Further, the reduction in TTX-R sodium currents was paralleled
by the emergence of a rapidly repriming TTX-S sodium current
in small dRG neurons after axotomy. Rapidly repriming TTX-S
current permits neuronal firing at higher than normal
frequencies186,187 and upregulation of its corresponding
transcript, Nav1.3, as well as protein product have been observed
in dRG neurons of adult rats after axotomy188-190, CCi191 and
SNl192. in contrast, transcripts encoding TTX-R sodium
currents are down regulated in small dRG neurons following
axotomy100,189. These alterations may, in part, be explained by a
loss of target derived neurotrophic factors after peripheral nerve
injuries. For instance, partial restoration of TTX-R currents,
along with upregulation of α-SNS transcript, was reported after
the administration of NGF to the proximal nerve stump193.
Further, intrathecal GdNF treatment prevented sensory
hypersensitivity after SNl injury and was associated with block
of A-fibre ectopic discharge and normalization of Nav1.3
expression in injured dRG194. in addition to the emergence of
rapidly-repriming TTX-S sodium currents, loss of target derived
GdNF is associated with a reduction in TTX-R currents in small
ib4-positive dRG neurons, whereas loss of NGF is associated
with a reduction in TTX-R currents in small peptidergic
neurons43. Taken together, it appears that nerve injury is
commonly associated with a reduction in TTX-R sodium
currents, allowing TTX-S currents to dominate as the major
generators of AP upstroke and, possibly, spontaneous ectopic AP
discharge in injured sensory neurons. however, Nav1.8
upregulation, along with the presence of functional TTX-R
sodium channels, have been associated with abberrant activity in
uninjured C-fibres and neuropathic pain behaviours after partial
nerve injury195. Therefore, the relevance of particular sodium
channel isoforms to neuropathic pain may depend on the extent
of nerve injury and, possibly, the degree of associated
inflammation. in broader terms, it is generally accepted that
increased Na+ channel function is associated with the onset and
maintenance of neuropathic pain and, in line with this, there has
been an impetus for the development of novel, state-dependent
ion channel modulators as potential therapeutic agents196.
Nerve injury-induced changes to the availability of potassium
channels. in large cutaneous afferent dRG neurons, a sustained
potassium current component, as well as the transient current, IA,
but not Id were reduced after axotomy197. Compared to
contralateral controls, mRNA expression for genes which
encode delayed rectifier (Kv1.1 and 1.2) and A-type (Kv1.4, 2.2,
4.2, and 4.3) voltage-gated potassium channels were reduced in
ipsilateral lumbar 4, 5 and 6 dRG one week following CCi198.
Unlike changes in IK,Ca after axotomy112, l5 SNl decreased IK,Ca
�lE JOURNAl CANAdiEN dES SCiENCES NEUROlOGiqUES
due to a direct effect on IK,Ca channels199. Though all IK,Ca
subtypes were decreased in small- and medium-sized dRG
neurons from the injured nerve, medium-sized dRG neurons
from the adjacent uninjured l4 nerve had increased iberiotoxin
sensitive (large conductance) and clotrimazole sensitive
(intermediate conductance) IK,Ca. in injured human peripheral
nerves, there was a decrease in human intermediate conductance
calcium-activated potassium channel 1 (hiK1)-like immunoreactivity predominately in large-, but also, in medium- and
small-sized dRG neurons when compared to controls200. like
sodium channels, these changes were associated with a loss of
target-derived neurotrophic support. Taken together, it appears
that nerve injury promotes a reduction in sustained and/or A-type
potassium currents which could account for broadening of APs,
as well as contributing to sensory neuron hyperexcitability
through a reduction in spike adaptation. Further, a reduction in
IK,Ca, whether directly or secondary to reductions in hvA
calcium currents (see below) serves as an additional ionic
mechanism for AP broadening and aberrant activity in sensory
neurons after peripheral nerve injury.
Nerve injury-induced changes to the availability of calcium
channels. After axotomy, the density of omega-conotoxin
GviA-sensitive (N-type) calcium current (ICa) is decreased and
is concurrent with increased inactivation in large-sized dRG
neurons associated with cutaneous afferents112,201. lvA or T-type
ICa is unaffected. by contrast, following CCi, T-type current
density is increased in small-sized rat dRG neurons, but was
without changes in voltage- and time-dependent parameters202.
Onset of diabetic neuropathy is also associated with increased Ttype, but not hvA, current density in ib4-positive, capsaicin
responsive medium-sized rat dRG neurons, as well as a
depolarizing shift in steady-state inactivation203.
Although the changes in ICa are variable and likely depend on
the nerve injury model and dRG cell type studied, alterations are
consistent with increased excitability. For instance, the reduction
in hvA or N-type ICa could underlie decreased calciumdependent potassium current after injury112 which, in turn, would
be expected to decrease AhP amplitude and shorten AhP
duration, ultimately, increasing firing frequency204. however, the
observed decrease in hvA ICa after peripheral nerve injury seems
inconsistent with the effectiveness of drugs, such as the
gabapentinoids205 and ziconotide113,206, which directly or
indirectly impede vGCC function. The likely explanation for
this paradox is that, whilst nerve injury may reduce hvA vGCC
expression on dRG cell bodies, expression in the central
terminals of primary afferents may be increased. This may in
turn lead to the increased release of neurotransmitters and other
mediators from primary afferents and the onset of central
sensitization. Thus, any consequence of vGCC blockade in
dRG neurons would be overcome by drug action at nerve
terminals. This possibility is illustrated by the actions of
morphine which can increase dRG excitability by an action on
Ca2+ channels207, yet opioids are known to produce analgesia,
impart, by blocking presynaptic Ca2+ channels and, thereby,
reducing neurotransmitter release from primary afferent
terminals208.
by contrast, a CCi induced increase in T-type current has
been correlated closely to more prominent afterdepolarizing
potentials (AdP), as well as a lowered rheobase for AP firing in
dRG neurons203. This has led to the identification of T-type
Volume 39, No. 4 – July 2012
calcium channels as a potential therapeutic target in pain
management196,209,210.
Nerve injury-induced changes to the availability of HCN
channels. Since the pacemaker current (Ih) acts to induce a
depolarization after a hyperpolarizing event, any upregulation
after nerve injury may contribute to enhanced neuronal
excitability neuropathic pain. Chronic compression of the dRG
(CCd) produces cutaneous hyperalgesia and enhanced
excitability of neuronal somata184,211. The CCd increased ih
current density and rate of activation, without changing its
reversal potential, voltage dependence of activation, or rate of
deactivation in medium-sized rat dRG neurons associated with
cutaneous afferents211. Further, SNl injury markedly increased
pacemaker currents in large diameter dRG neurons212.
Pharmacological blockade of Ih with Zd7288 decreased firing
frequency of ectopic discharges originating in injured Aβ- and
Aδ-fibres and was concurrent with the reversal of mechanical
allodynia. Changes may not be limited to the cell body, however,
and can involve the axonal accumulation of the hCN channels at
the site of sciatic nerve injury159. intriguingly, more recent
reports suggest hCN channels are important in both the
establishment and maintenance of neuropathic pain, where
specific hCN channel isoforms could play important roles213,214.
in addition to injury-induced changes in ion channel
availability, extrinsic mechanisms also contribute to the
generation of ectopic activity in sensory neurons. These include
sprouting of perivascular sympathetic neurons within the
dRG215-218. Although normal dRG neurons are insensitive to
noradrenaline, injury-induced upregulation of α-adrenoceptors218-220 and the formation of baskets of sympathetic axons
around dRG neurons215 enables excitation of neurons that may
contribute to ‘sympathetically maintained pain’ (complex
regional syndrome ii). Additionally, neurogenic inflammation,
involving the release of CGRP and SP from sensory nerve
endings17, may contribute to altered ongoing activity in sensory
neurons. lastly, there is evidence that ectopic excitatory
interactions may occur between neuronal cell bodies in the dRG
following nerve injury221.
Central sensitization
in 1983, Clifford Woolf’s study of injury induced changes to
the cutaneous receptive field properties of flexor motor neurons
in rat provided the first pieces of evidence for spinal cord
plasticity and central sensitization177. Essentially, repeated
noxious heat stimuli presented to the paw produced a sustained
increase in the excitability of α-motor neuron axons which was
characterized by: Aβ-fibre recruitment to the, normally,
nociceptor specific reflex; expanse of the receptive field which
was unresponsive to local anaesthetics applied to the site of
injury; and all of which could be mimicked by C-fibre strength
electrical stimulations of the sural nerve. Since these findings
were difficult to explain within the context of a peripherally
driven mechanism, a central process was implicated. it is now
appreciated that central sensitization is a form of nervous system
plasticity composed of increases in membrane excitability222,
synaptic facilitation223,224, loss of inhibition225, reversal of
inhibition (disinhibition)226 and enhancement of excitation227 of
central circuitry which promotes spontaneous pain, allodynia
and hyperalgesia after inflammation or lesions to the nervous
425
�ThE CANAdiAN JOURNAl OF NEUROlOGiCAl SCiENCES
system3. The net effect is the recruitment of previously
subthreshold inputs from low-threshold receptors and highthreshold receptors from outside a given receptive field to the
output of central nociceptive neurons. These inputs can be
experimentally revealed in the spinal cord after the
administration of synaptic blockers of inhibitory transmission,
such as GAbAA receptor antagonists, which enable Aβ-fibre
input into the superficial dorsal horn225 and pain-like responses
elicited by the movement of hairs228. This heightened pain
response is protective when maintained by peripheral
mechanisms responding to inflammatory cues which subside
over the course of healing. A major feature of neuropathic pain,
however, is that it is a manifestation of maladaptive plasticity in
the nervous system where changes to the nociceptive pathway
enabling central sensitization do not return to pre-injury status229.
Therefore, the somatosensory system is left in a persistent state
where it can no longer distinguish innocuous information from
nociceptive information.
in the context of neuropathic pain, the mechanisms
responsible for the establishment and maintenance of central
sensitization remain poorly understood. What seems clear is that
multiple mechanisms are involved after nerve injury to increase
excitability and reduce inhibition3. it has been shown that 13-25
days of sciatic nerve CCi produces changes in the synaptic
excitation of lii neurons, where there is a decrease in excitatory
synaptic drive to inhibitory, tonic cells and an increase in
excitatory synaptic drive to putative excitatory neurons227.
Further, these changes are concurrent with the onset of
mechanical allodynia and hyperalgesia. One of the early
consequences of CCi is the activation of spinal microglia and the
release of bdNF230. Since nervous system injury is associated
with elevated levels of bdNF231 and neuropathic pain-related
behaviours are attenuated by sequestering bdNF230, bdNF has
become a molecule of interest in nerve injury related central
sensitization. We recently found that spinal cord cultures
exposed to five to six days of bdNF produced a similar
‘electrophysiological signature’ to that seen with CCi232 and that
activated microglia enhanced overall dorsal horn excitability
through the release of bdNF233. microglia-derived bdNF has
also been shown to mediate nerve injury induced disinhibition
through causing the collapse of the transmembrane anion
gradient and compromising control over firing rate in li
neurons230,234. in addition to reducing inhibitory tone in the
dorsal horn, bdNF release has been associated with the
enhancement of N-methyl-d-aspartate (NmdA) receptor
mediated depolarizations in the rat spinal cord235, as well as the
enhancement of NmdA receptor mediated excitatory post
synaptic currents (epscs) in lii dorsal horn neurons224. it was
further demonstrated that ATP and its release from damaged cells
can activate microglia and, through P2X4 purinergic receptor
(P2X4R) stimulation, promotes the release of bdNF236.
One might, therefore, suggest that peripheral nerve injury and
the resultant chronic increase in primary afferent excitability
increases the release of ATP from primary afferent terminals.
This activates microglia, triggering the release of bdNF which
promotes an increase in superficial dorsal horn excitability
through a functional loss of inhibitory circuits and enhancement
of synaptic strength at excitatory synapses. bdNF is, however,
only one piece to a very complicated puzzle and several studies
426
have described contributions of other molecules, cell types and
processes to the establishment and maintenance of central
sensitization after nerve injury3,229,237.
Nerve injury
Ectopic discharge in primary afferents is secondary to direct
axonal damage and disruption of the myelin sheath that
surrounds many axons238. Cutting an axon, results in
degeneration of the distal segment as a consequence of
interruption in axonal flow and transport which deprives the
distal axon and nerve ending of its normal metabolic interaction
with the cell body239,240. Wallerian degeneration leads to loss of
the distal axonal segment and involves responses from glial
cells, immune cells, in addition to peripheral nerves. The
proximal portion of damaged primary afferents can undergo
phenotypic switch in response to retrograde loss of targetderived trophic factors. however, the electrical behaviour of
both injured and uninjured nerve fibres is altered in response to
injury195,241. in parallel, the chemical environment is changed
and several mediators are known to interact with sensory
neurons239. Alterations in sensory neuron phenotype and
electrical activity likely contribute to central sensitization and
neuropathic pain.
Nerve degeneration
Nerve degeneration is not limited to nerve transections, but
exists in other models of nerve injury242, as well as in disease
states and infections243,244. in the case of axotomy, the proximal
axonal segment and attached cell body becomes isolated from
the distal segment240. Cytoplasmic materials build up as the ends
of both segments become sealed, forming swollen retraction
bulbs. in a process known as Wallerian degeneration, the distal
axon swells and becomes a series of beaded fragments. Cellular
debris from the terminal and distal axon is then cleared by
phagocytic cells, such as macrophages. Although variable
among species, Wallerian degeneration in rodent models of
peripheral nerve injury occurs within a few days following
injury245-247. in contrast, the proximal segment is spared since it
is still physically and metabolically coupled to the surviving cell
body. during degeneration, retrograde signals produce changes
in the cell body and include swelling, eccentric positioning of the
nucleus and the breaking apart of rough endoplasmic reticulum
(chromatolysis)248. These changes are associated with the
production of protein required for nerve regeneration and cease
once connections are restored. if the cell body dies, the
degenerative process spreads to the remaining proximal
segment. Thus, nerve degeneration occurs over several days,
affects the entire neuron and involves several cell types.
Inflammation
injury to peripheral nerves results in a local inflammatory
response characterized by the activation of resident mast cells
and macrophages, supportive Schwann cells along the axon and
satellite cells in the dRG237,239,249. in addition, the inflammatory
response is augmented by the infiltration of circulating
phagocytes (macrophages and neutrophils), T-lymphocytes and
natural killer cells which contribute to the removal of cellular
debris, neutralization of pathogens, regeneration of axons and
�lE JOURNAl CANAdiEN dES SCiENCES NEUROlOGiqUES
formation of a neuroma237,250. Corresponding to these events, an
‘inflammatory soup’ of bradykinins, SP, hydrogen ions, NGF,
prostaglandins, histamine, ATP and proinflammatory cytokines
is produced18.
Several lines of evidence underline the importance of the
local inflammatory response in the generation of centralized
pain. For instance, cardinal signs of inflammation, such as the
presence of edema, correlate more strongly with nocifensive
behaviours than the extent of fibre loss after fixed-diameter
polyethylene cuff nerve injury242. Encasing the nerve stump after
sciatic nerve transection, in order to minimize contact with
infiltrating immune cells and inflammatory mediators, attenuates
pain-related behaviours, such as autotomy251. The local response
of early inflammatory cellular mediators, including the
degranulation of mast cells and the accumulation of neutrophils,
is important in the generation of hyperalgesia after partial nerve
injuries252,253. Cui and colleagues demonstrated a strong
correlation between degree of local macrophage/monocyte
infiltration among three nerve injury models and the presence of
mechanical allodynia254. lastly, peripheral nerve injuries such as
CCi are associated with an inflammatory response of higher
magnitiude than sciatic nerve transections254 and invoke
downregulation of GAbAergic functions in the superficial dorsal
horn while axotomy is ineffective255. Similarly, CCi produces
greater augmentation of excitatory synaptic transmission than
sciatic nerve axotomy256.
Several inflammatory mediators released from damaged
tissue alter the electrical properties of sensory neurons. For
instance, hydrogen ions and ATP act through the non-selective
cation channels TRPv1, ASiCs and P2X to depolarize sensory
neurons towards AP threshold257-259. In vivo administration of SP
to glabrous skin produces hyperalgesia and allodynia260,261.
Further, SP release depolarizes and excites small nociceptive
sensory neurons262,263 which express the neurokinin-1(NK1)
receptor264. Excitation of peptidergic fibres, not only leads to
neuropeptide release centrally, but antidromic propagation of
APs can also result in peripheral release and further exacerbate
inflammation (neurogenic inflammation)17,265. in support, NK-1
receptor antagonists applied either centrally266,267 or
peripherally268, attenuate or delay the onset of pain-related
behaviours in response to nerve injury.
The involvement of NGF in inflammatory pain is well
documented, however, NGF expression is upregulated in several
cell types, including dRG neurons269, Schwann cells237 and
satellite cells270 after nerve injury. Consistent with a role in nerve
injury and, perhaps, neuropathic pain, NGF antagonism, with
anti-serum application at the site of nerve injury, attenuated or
delayed the onset of hyperalgesia after CCi269,271. NGF release
can enhance excitability of primary afferents in several ways,
including an increase in TRPv1 activity272, sensitivity273 and
expression274. in addition to the maintenance of TTX-R sodium
currents (Nav1.8) through Trk receptors43, NGF signalling
through the p75 neurotrophin receptor275, can increase AP firing
and is concurrent with an enhancement of TTX-R sodium
current and a suppression of delayed rectifier-like potassium
current276.
Endogenous proteases, such as trypsin, activate tethered
ligand protease-activated receptors 2 (PAR-2), a novel class of
G-protein coupled receptors (GPCR), expressed on small-sized
Volume 39, No. 4 – July 2012
nociceptive dRG neurons277. PAR-2 activation reduces mcurrent which results in membrane depolarization and the
generation of APs278,279. in addition and similar to the activation
of metabotropic P2Y purinergic receptors280,281 and bradykinin-2
(b2) receptors282, PAR-2 activation sensitizes TRP channels
which are associated with hyperalgesia277,283. Consistent with
these observations, injection of PAR-2 agonists in vivo induces
pain-related behaviours66, whereas, antagonists produce
antinociceptive effects284.
The association of eicosanoids and their synthesizing
enzymes, cyclo-oxygenase- 1 (COX-1) and particularly the
inducible COX-2, with inflammation and pain is well
documented285,286. For instance, prostaglandin E2 (PGE2) or
prostaglandin i2 (PGi2; prostacyclin) administration induces
hyperalgesia287,288. Further, PGi2 and PGE2 enhance the
sensitivity of primary afferents to either mechanical or chemical
stimulation289-291. PGE2 and PGi2 receptors (EP and iP,
respectively) are expressed in sensory neurons292-294 and in vitro
application of PGE2 or PGi2 on dRG neurons lowers firing
threshold295 and increases AP firing upon current injection,
elevated potassium or bradykinin application296,297. Consistent
with hyperexcitability, PGE2 and a PGi2 analogue suppress a
sustained-type potassium current297 and, similar to serotonin,
prostaglandins upregulate TTX-R sodium currents298-301. in
addition, Ih is positively modulated by PGE2 in trigeminal
ganglion cells302. Through a receptor mediated mechanism of
action, PGE2 and PGi2 also sensitize TRPv1 channels,
producing hyperalgesia in mice303. last, it has also been
suggested that hyperalgesia induced by bradykinin,
norepinephrine and cytokines is secondary to the production of
prostaglandins304.
The actions of several major pro-inflammatory cytokines,
such as TNF-α and il-6, are also associated with pain
hypersensitivity and, perhaps, neuropathic pain305,306. however,
accumulating evidence implicates direct involvement of il-1β in
the enduring increase in sensory neuron excitability commonly
observed after peripheral nerve injury. For instance, mRNA307
and protein308,309 expression of the il-1β receptor, il-1Ri, in
sensory neurons implies that il-1β can directly affect primary
afferents. in agreement, changes in the electrical properties of
sensory neurons consistent with increased excitability occur
within minutes of il-1β application309,310, as well as the onset of
pain-related behaviours after intraplantar injections of il-1β309.
importantly, il-1β expression311, secretion312 and processing313
are upregulated for several days following peripheral nerve
injury and we have recently reported that such long-term (five to
six days) exposure to il-1β alters the excitability of dRG
neurons314. For instance, the effects of long-term il-1β exposure
in medium and small, ib4-positive dRG neurons parallel
changes observed after nerve injury, such as a reduction in
rheobase and increased repetitive discharge. Since changes in
injured sensory neurons may lead to central sensitization, il-1β
may be of particular importance in the establishment of
neuropathic pain.
At this point, another issue relevant to inflammation and
peripheral nerve should be mentioned. it is generally believed
that inflammation not only protects injured tissue from infection,
but that it may itself initiate the healing process315-317. For
example, it has recently been suggested that injury-induced
increase in interleukin-1β and TNF-α protein levels is required
427
�ThE CANAdiAN JOURNAl OF NEUROlOGiCAl SCiENCES
for functional nerve recovery311. This implies that attempts to
attenuate neuropathic pain by preventing the actions of
interleukin-1β and TNF-α, may lead to impaired restoration of
function in nerve injury situations.
Research (AhFmR) studentship and an AhFmR dr. lionel E.
mcleod health Research Scholarship.
REFERENCES
1.
Phenotypic switch
Although CGRP and SP expression appears to be
downregulated in injured sensory neurons318,319, respective
receptor antagonists applied either centrally266,267,320 or
peripherally268, attenuate or delay the onset of pain-related
behaviours in response to nerve injury. This apparent paradox
may be explained by phentoypic shifts and / or contributions
from uninjured sensory neurons after nerve injury. For instance,
some nerve injuries321 result in a phenotypic shift where large,
rather than small, sensory neurons begin to express322,323 and
become responsive to SP263. Another phenotypic switch pertains
to bdNF. Under normal circumstances, bdNF mRNA and
protein is expressed in nociceptive sensory neurons324, however,
bdNF becomes upregulated in large diameter dRG neurons and
is concurrent with increased anterograde transport to the dorsal
horn after sciatic axotomy325. it has, therefore, been suggested
that an injury induced shift in the phenotype of sensory neurons
may alter the efficacy of synaptic input into the spinal cord237.
2.
3.
4.
5.
6.
7.
8.
9.
CONCLUSIONS
There is now strong evidence linking the inflammatory milieu
after nerve injury to changes in the electrical activity of sensory
neurons and pain-related behaviours. The net effect is that
primary afferents send volleys of spontaneous, ectopic discharge
to the dorsal horn which can then trigger central sensitization.
The association between this enduring increase in primary
afferent activity after peripheral nerve injury and neuropathic
pain is now well established.
These findings do not contradict the description of
neuropathic pain as ‘non-inflammatory pain’ as the initial
inflammatory trigger normally subsides by the time the patient
presents. Although evidence is mounting to support the role of
interleukin-1β and other cytokines in the onset of neuropathic
pain, drugs which antagonize of prevent the actions of these
mediators may be of limited value in the clinic as the use of such
agents would be analogous to ‘closing the barn door after the
horse has bolted’. it is already well known that nonsteroidal antiinflammatory drugs are largely ineffective in the treatment of
neuropathic pain. however, it is possible that attenuation of the
actions of inflammatory mediators may impact the transition
from acute to chronic pain. Alternatively, the identification of
various types of voltage gated ion channels in the aetiology of
neuropathic pain may be more relevant to the development of
therapy, because their participation may outlast that of
inflammatory mediators.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
ACKNOWLEDGMENTS
The authors thank dr. Nataliya bukhanova-Schultz for help
with the figure.
22.
23.
GRANTS
Supported by Canadian institutes of health Research. PlS
was supported by an Alberta heritage Foundation for medical
428
24.
merskey h, bogduk N. Part iii: Pain terms, a current list with
definitions and notes on usage. in: merskey h, bogduk N,
editors. Classification of chronic pain: descriptions of chronic
pain syndromes and definitions of pain terms. Seattle: iASP
Press; 1994. p. 209-14.
Wang h, Woolf CJ. Pain TRPs. Neuron. 2005;46(1):9-12.
latremoliere A, Woolf CJ. Central sensitization: a generator of pain
hypersensitivity by central neural plasticity. J Pain. 2009;10(9):
895-926.
Cox JJ, Reimann F, Nicholas AK, et al. An SCN9A channelopathy
causes congenital inability to experience pain. Nature. 2006;444
(7121):894-8.
lee mC, mouraux A, iannetti Gd. Characterizing the cortical
activity through which pain emerges from nociception. J
Neurosci. 2009;29(24):7909-16.
Wall Pd. introduction to the fourth edition. in: Wall Pd, melzack
R, editors. Textbook of pain. london: harcourt Publishers
limited; 1999. p. 1-8.
Klit h, Finnerup Nb, Jensen TS. Central post-stroke pain: clinical
characteristics, pathophysiology, and management. lancet
Neurol. 2009;8(9):857-68.
Price dd. Psychological and neural mechanisms of the affective
dimension of pain. Science. 2000;288(5472):1769-72.
mcCaffery m, Pasero C. Assessment: underlying complexities,
misconceptions, and practical tools. in: mcCaffery m, Pasero C,
editors. Pain: clinical manual. 2 ed. St. louis: mosby; 1999. p.
35-102.
Rainville P, Carrier b, hofbauer RK, et al. dissociation of sensory
and affective dimensions of pain using hypnotic modulation.
Pain. 1999;82(2):159-71.
Rainville P, duncan Gh, Price dd, et al. Pain affect encoded in
human anterior cingulate but not somatosensory cortex. Science.
1997;277(5328):968-71.
mogil JS. Animal models of pain: progress and challenges. Nat Rev
Neurosci. 2009;10(4):283-94.
hummel m, lu P, Cummons TA, et al. The persistence of a longterm negative affective state following the induction of either
acute or chronic pain. Pain. 2008;140(3):436-45.
Sandkuhler J. models and mechanisms of hyperalgesia and
allodynia. Physiol Rev. 2009;89(2):707-58.
backonja mm, Stacey b. Neuropathic pain symptoms relative to
overall pain rating. J Pain. 2004;5(9):491-7.
mogil JS, Crager SE. What should we be measuring in behavioral
studies of chronic pain in animals? Pain. 2004;112(1-2):12-15.
Richardson Jd, vasko mR. Cellular mechanisms of neurogenic
inflammation. J Pharmacol Exp Ther. 2002;302(3):839-45.
irving GA. Contemporary assessment and management of
neuropathic pain. Neurology. 2005;64(12 Suppl 3):S21-7.
Aley KO, messing RO, mochly-Rosen d, et al. Chronic
hypersensitivity for inflammatory nociceptor sensitization
mediated by the epsilon isozyme of protein kinase C. J Neurosci.
2000; 20(12):4680-5.
honore P, Rogers Sd, Schwei mJ, et al. murine models of
inflammatory, neuropathic and cancer pain each generates a
unique set of neurochemical changes in the spinal cord and
sensory neurons. Neuroscience. 2000;98(3):585-98.
Perl ER. Function of dorsal root ganglion neurons: an overview. in:
Sheryl A. Scott, editor. Sensory neurons diversity, development,
and plasticity. New York: Oxford University Press; 1992. p.
3-23.
Gasser hS. The control of excitation in the nervous system. bull N
Y Acad med. 1937;13(6):324-48.
light AR, Perl ER. Unmyelinated afferent fibers are not only for
pain anymore. J Comp Neurol. 2003;461(2):137-9.
Olausson h, lamarre Y, backlund h, et al. Unmyelinated tactile
afferents signal touch and project to insular cortex. Nat
Neurosci. 2002;5(9):900-4.
�lE JOURNAl CANAdiEN dES SCiENCES NEUROlOGiqUES
25. harper AA, lawson SN. Conduction velocity is related to
morphological cell type in rat dorsal root ganglion neurones. J
Physiol. 1985;359:31-46.
26. Abdulla FA, Smith PA. Axotomy- and autotomy-induced changes
in the excitability of rat dorsal root ganglion neurons. J
Neurophysiol. 2001;85(2):630-43.
27. Aoki Y, Takahashi Y, Ohtori S, et al. distribution and
immunocytochemical characterization of dorsal root ganglion
neurons innervating the lumbar intervertebral disc in rats: a
review. life Sci. 2004;74(21):2627-42.
28. Silverman Jd, Kruger l. Selective neuronal glycoconjugate
expression in sensory and autonomic ganglia: relation of lectin
reactivity to peptide and enzyme markers. J Neurocytol. 1990;19
(5):789-801.
29. bradbury EJ, burnstock G, mcmahon Sb. The expression of P2X3
purinoreceptors in sensory neurons: effects of axotomy and
glial-derived neurotrophic factor. mol Cell Neurosci. 1998;12(45):256-68.
30. lee Y, Takami K, Kawai Y, et al. distribution of calcitonin generelated peptide in the rat peripheral nervous system with
reference to its coexistence with substance P. Neuroscience.
1985;15(4):1227-37.
31. lee Y, Kawai Y, Shiosaka S, et al. Coexistence of calcitonin generelated peptide and substance P-like peptide in single cells of the
trigeminal ganglion of the rat: immunohistochemical analysis.
brain Res. 1985;330(1):194-6.
32. hokfelt T, Elde R, Johansson O, et al. immunohistochemical
evidence for separate populations of somatostatin-containing
and substance P-containing primary afferent neurons in the rat.
Neuroscience. 1976;1(2):131-6.
33. Caterina mJ, Schumacher mA, Tominaga m, et al. The capsaicin
receptor: a heat-activated ion channel in the pain pathway.
Nature. 1997;389(6653):816-24.
34. Guo A, vulchanova l, Wang J, et al. immunocytochemical
localization of the vanilloid receptor 1 (vR1): relationship to
neuropeptides, the P2X3 purinoceptor and ib4 binding sites. Eur
J Neurosci. 1999;11(3):946-58.
35. Aoki Ym, Ohtori Sm, Takahashi Km, et al. Expression and coexpression of vR1, CGRP, and ib4-binding glycoprotein in
dorsal root ganglion neurons in rats: differences between the disc
afferents and the cutaneous afferents. Spine. 2005;30(13):
1496-500.
36. bennett dlh, michael GJ, Ramachandran N, et al. A distinct
subgroup of small dRG cells express GdNF receptor
components and GdNF is protective for these neurons after
nerve injury. J Neurosci. 1998;18(8):3059-72.
37. bennett dl, Averill S, Clary dO, et al. Postnatal changes in the
expression of the trkA high-affinity NGF receptor in primary
sensory neurons. Eur J Neurosci. 1996;8(10):2204-8.
38. Stephens hE, belliveau AC, Gupta JS, et al. The role of
neurotrophins in the maintenance of the spinal cord motor
neurons and the dorsal root ganglia proprioceptive sensory
neurons. int J dev Neurosci. 2005;23(7):613-20.
39. lindsay Rm. The role of neurotrophic factors in functional
maintenance of mature sensory neurons. in: Scott SA, editor.
Sensory neurons diversity, development, and plasticity. New
York; 1992. p. 404-20.
40. Averill S, mcmahon Sb, Clary dO, et al. immunocytochemical
localization of trkA receptors in chemically identified subgroups
of adult rat sensory neurons. Eur J Neurosci. 1995;7(7):1484-94.
41. molliver dC, Wright dE, leitner ml, et al. ib4-binding dRG
neurons switch from NGF to GdNF dependence in early
postnatal life. Neuron. 1997;19(4):849-61.
42. Airaksinen mS, Saarma m. The GdNF family: signalling,
biological functions and therapeutic value. Nat Rev Neurosci.
2002;3(5):383-94.
43. Fjell J, Cummins TR, dib-hajj Sd, et al. differential role of GdNF
and NGF in the maintenance of two TTX-resistant sodium
channels in adult dRG neurons. brain Res mol brain Res. 1999;
67(2):267-82.
44. Snider Wd, Wright dE. Neurotrophins cause a new sensation.
Neuron. 1996;16(2):229-32.
Volume 39, No. 4 – July 2012
45. luo W, Wickramasinghe SR, Savitt Jm, et al. A hierarchical NGF
signaling cascade controls Ret-dependent and Ret-independent
events during development of nonpeptidergic dRG neurons.
Neuron. 2007;54(5):739-54.
46. valdés-Sánchez Km, Pérez-villalba A, vega JA, et al. bdNF is
essentially required for the early postnatal survival of
nociceptors. dev biol. 2010;339(2):465-76.
47. mcmahon Sb, Armanini mP, ling lh, et al. Expression and
coexpression of Trk receptors in subpopulations of adult primary
sensory neurons projecting to identified peripheral targets.
Neuron. 1994;12(5):1161-71.
48. Wright dE, Snider Wd. Neurotrophin receptor mRNA expression
defines distinct populations of neurons in rat dorsal root ganglia.
J Comp Neurol. 1995;351(3):329-38.
49. Airaksinen mS, Koltzenburg m, lewin GR, et al. Specific subtypes
of cutaneous mechanoreceptors require neurotrophin-3
following peripheral target innervation. Neuron. 1996;16(2):
287-95.
50. lumpkin EA, Caterina mJ. mechanisms of sensory transduction in
the skin. Nature. 2007;445(7130):858-65.
51. voets T, droogmans G, Wissenbach U, et al. The principle of
temperature-dependent gating in cold- and heat-sensitive TRP
channels. Nature. 2004;430(7001):748-54.
52. dhaka A, viswanath v, Patapoutian A. TRP ion channels and
temperature sensation. Annu Rev Neurosci. 2006;29(1):135-61.
53. Ramsey iS, delling m, Clapham dE. An introduction to TRP
channels. Annu Rev Physiol. 2006;68:619-47.
54. Schepers RJ, Ringkamp m. Thermoreceptors and thermosensitive
afferents. Neurosci biobehav Rev. 2009;33(3):205-12.
55. Caterina mJ, Julius d. The vanilloid receptor: a molecular gateway
to the pain pathway. Annu Rev Neurosci. 2001;24:487-517.
56. bandell m, Story Gm, hwang SW, et al. Noxious cold ion channel
TRPA1 is activated by pungent compounds and bradykinin.
Neuron. 2004;41(6):849-57.
57. Peier Am, moqrich A, hergarden AC, et al. A TRP channel that
senses cold stimuli and menthol. Cell. 2002;108(5):705-15.
58. Kwan KY, Allchorne AJ, vollrath mA, et al. TRPA1 contributes to
cold, mechanical, and chemical nociception but is not essential
for hair-cell transduction. Neuron. 2006;50(2):277-89.
59. Suzuki m, mizuno A, Kodaira K, et al. impaired pressure sensation
in mice lacking TRPv4. J biol Chem. 2003;278(25):22664-8.
60. Alessandri-haber N, Joseph E, dina OA, et al. TRPv4 mediates
pain-related behavior induced by mild hypertonic stimuli in the
presence of inflammatory mediator. Pain. 2005;118(1-2):70-9.
61. Alloui A, Zimmermann K, mamet J, et al. TREK-1, a K+ channel
involved in polymodal pain perception. EmbO J. 2006;25(11):
2368-76.
62. maingret F, lauritzen i, Patel AJ, et al. TREK-1 is a heat-activated
background K(+) channel. EmbO J. 2000;19(11):2483-91.
63. Patel AJ, honore E, maingret F, et al. A mammalian two pore
domain mechano-gated S-like K+ channel. EmbO J. 1998;17
(15):4283-90.
64. lumpkin EA, bautista dm. Feeling the pressure in mammalian
somatosensation. Curr Opin Neurobiol. 2005;15(4):382-8.
65. morris CE, Juranka PF. Nav channel mechanosensitivity: activation
and inactivation accelerate reversibly with stretch. biophys J.
2007;93(3):822-33.
66. vergnolle N, bunnett NW, Sharkey KA, et al. Proteinase-activated
receptor-2 and hyperalgesia: a novel pain pathway. Nat med.
2001;7(7):821-6.
67. Kruger l, Perl ER, Sedivec mJ. Fine structure of myelinated
mechanical nociceptor endings in cat hairy skin. J Comp Neurol.
1981;198(1):137-54.
68. burgess PR, Perl ER. myelinated afferent fibres responding
specifically to noxious stimulation of the skin. J Physiol. 1967;
190(3):541-62.
69. bessou P, Perl ER. Response of cutaneous sensory units with
unmyelinated fibers to noxious stimuli. J Neurophysiol. 1969;32
(6):1025-43.
70. handwerker hO, Kilo S, Reeh PW. Unresponsive afferent nerve
fibres in the sural nerve of the rat. J Physiol. 1991;435:229-42.
71. michaelis m, habler hJ, Jaenig W. Silent afferents: a separate class
of primary afferents? Clin Exp Pharmacol Physiol. 1996;23(2):
99-105.
429
�ThE CANAdiAN JOURNAl OF NEUROlOGiCAl SCiENCES
72. munger bl, ide C. The structure and function of cutaneous sensory
receptors. Arch histol Cytol. 1988;51(1):1-34.
73. Suzuki m, Watanabe Y, Oyama Y, et al. localization of
mechanosensitive channel TRPv4 in mouse skin. Neurosci lett.
2003;353(3):189-92.
74. Alvarez FJ, Fyffe RE. Nociceptors for the 21st century. Curr Rev
Pain. 2000;4(6):451-8.
75. denda m, Nakatani m, ikeyama K, et al. Epidermal keratinocytes
as the forefront of the sensory system. Exp dermatol. 2007;16
(3):157-61.
76. González-martínez T, Germanà, P, monjil dF, et al. Absence of
meissner corpuscles in the digital pads of mice lacking
functional Trkb. brain Res. 2004;1002(1-2):120-8.
77. Johnson KO. The roles and functions of cutaneous
mechanoreceptors. Curr Opin Neurobiol. 2001;11(4):455-61.
78. brodal P. Peripheral parts of the somatosensory system. in: brodal
P, editor. The central nervous system structure and function. New
York: Oxford University Press; 2010. p. 165-89.
79. boulais N, misery l. merkel cells. J Am Acad dermatol. 2007;
57(1):147-65.
80. matsuda Y, Yoshida S, Yonezawa T. Tetrodotoxin sensitivity and Ca
component of action potentials of mouse dorsal root ganglion
cells cultured in vitro. brain Res. 1978;154(1):69-82.
81. Yoshida S, matsuda Y, Samejima A. Tetrodotoxin-resistant sodium
and calcium components of action potentials in dorsal root
ganglion cells of the adult mouse. J Neurophysiol. 1978;41(5):
1096-106.
82. Koerber hR, druzinsky RE, mendell lm. Properties of somata of
spinal dorsal root ganglion cells differ according to peripheral
receptor innervated. J Neurophysiol. 1988;60(5):1584-96.
83. harper AA, lawson SN. Electrical properties of rat dorsal root
ganglion neurones with different peripheral nerve conduction
velocities. J Physiol. 1985;359:47-63.
84. Gurtu S, Smith PA. Electrophysiological characteristics of hamster
dorsal root ganglion cells and their response to axotomy. J
Neurophysiol. 1988;59(2):408-23.
85. Nicholls JG, baylor dA. Specific modalities and receptive fields of
sensory neurons in CNS of the leech. J Neurophysiol. 1968;31
(5):740-56.
86. Rose Rd, Koerber hR, Sedivec mJ, et al. Somal action potential
duration differs in identified primary afferents. Neurosci lett.
1986;63(3):259-64.
87. Koerber hR, mendell lm. Functional heterogeneity of dorsal root
ganglion cells. in: Scott SA, editor. Sensory neurons diversity,
development, and plasticity. New York: Oxford University Press;
1992. p. 77-96.
88. djouhri l, bleazard l, lawson SN. Association of somatic action
potential shape with sensory receptive properties in guinea-pig
dorsal root ganglion neurones. J Physiol. 1998;513(Pt 3):857-72.
89. Fang X, djouhri l, mcmullan S, et al. intense isolectin-b4 binding
in rat dorsal root ganglion neurons distinguishes C-fiber
nociceptors with broad action potentials and high Nav1.9
expression. J Neurosci. 2006;26(27):7281-92.
90. Traub RJ, mendell lm. The spinal projection of individual
identified A-delta- and C-fibers. J Neurophysiol. 1988;59(1):
41-55.
91. Nowycky mC. voltage-gated ion channels in dorsal root ganglion
neurons. in: Scott SA, editor. Sensory neurons diversity,
development, and plasticity. New York: Oxford University Press;
1992. p. 97-115.
92. Catterall WA. From ionic currents to molecular mechanisms: the
structure and function of voltage-gated sodium channels.
Neuron. 2000;26(1):13-25.
93. beneski dA, Catterall WA. Covalent labeling of protein
components of the sodium channel with a photoactivable
derivative of scorpion toxin. PNAS. 1980;77(1):639-43.
94. Catterall WA, Goldin Al, Waxman SG. international Union of
Pharmacology. Xlvii. Nomenclature and structure-function
relationships of voltage-gated sodium channels. Pharmacol Rev.
2005;57(4):397-409.
95. Terlau h, heinemann Sh, Stühmer W, et al. mapping the site of
block by tetrodotoxin and saxitoxin of sodium channel ii. FEbS
lett. 1991;293(1-2):93-6.
430
96. Caffrey Jm, Eng dl, black JA, et al. Three types of sodium
channels in adult rat dorsal root ganglion neurons. brain Res.
1992;592(1-2):283-97.
97. Rizzo mA, Kocsis Jd, Waxman SG. Slow sodium conductances of
dorsal root ganglion neurons: intraneuronal homogeneity and
interneuronal heterogeneity. J Neurophysiol. 1994;72(6):
2796-815.
98. Akopian AN, Sivilotti l, Wood JN. A tetrodotoxin-resistant
voltage-gated sodium channel expressed by sensory neurons.
Nature. 1996;379(6562):257-62.
99. Sangameswaran l, delgado SG, Fish lm, et al. Structure and
function of a novel voltage-gated, tetrodotoxin-resistant sodium
channel specific to sensory neurons. J biol Chem. 1996;271(11):
5953-6.
100. dib-hajj Sd, Tyrrell l, black JA, et al. NaN, a novel voltage-gated
Na channel, is expressed preferentially in peripheral sensory
neurons and down-regulated after axotomy. PNAS. 1998;95(15):
8963-8.
101. Rush Am, Cummins TR, Waxman SG. multiple sodium channels
and their roles in electrogenesis within dorsal root ganglion
neurons. J Physiol. 2007;579(Pt 1):1-14.
102. Abdulla FA, Smith PA. Changes in Na(+) channel currents of rat
dorsal root ganglion neurons following axotomy and axotomyinduced autotomy. J Neurophysiol. 2002;88(5):2518-29.
103. Cummins TR, dib-hajj Sd, black JA, et al. A novel persistent
tetrodotoxin-resistant sodium current in SNS-null and wild-type
small primary sensory neurons. J Neurosci. 1999;19(24):43RC.
104. Gover Td, moreira Th, Weinreich d. Role of calcium in regulating
primary sensory neuronal excitability. in: Canning bJ, Spina d,
editors. Sensory nerves: handbook of experimental
pharmacology. berlin heidelberg: Springer; 2009. p. 563-87.
105. Catterall WA, Perez-Reyes E, Snutch TP, et al. international Union
of Pharmacology. Xlviii. Nomenclature and structure-function
relationships of voltage-gated calcium channels. Pharmacol Rev.
2005;57(4):411-25.
106. Catterall WA. Structure and regulation of voltage-gated Ca2+
channels. Annu Rev Cell dev biol. 2000;16(1):521-55.
107. Scroggs RS, Fox AP. Calcium current variation between acutely
isolated adult rat dorsal root ganglion neurons of different size. J
Physiol. 1992;445:639-58.
108. Fuchs A, Rigaud m, Sarantopoulos Cd, et al. Contribution of
calcium channel subtypes to the intracellular calcium signal in
sensory neurons: the effect of injury. Anesthesiology. 2007;107
(1):117-27.
109. Acosta CG, lopez hS. δ Opioid receptor modulation of several
voltage-dependent Ca2+ currents in rat sensory neurons. J
Neurosci. 1999;19(19):8337-48.
110. Schroeder JE, Fischbach PS, mcCleskey EW. T-type calcium
channels: heterogeneous expression in rat sensory neurons and
selective modulation by phorbol esters. J Neurosci. 1990;10(3):
947-51.
111. lu SG, Zhang X, Gold mS. intracellular calcium regulation among
subpopulations of rat dorsal root ganglion neurons. J Physiol.
2006;577(1):169-90.
112. Abdulla FA, Smith PA. Axotomy- and autotomy-induced changes
in Ca2+and K+ channel currents of rat dorsal root ganglion
neurons. J Neurophysiol. 2001;85(2):644-58.
113. Zamponi GW, lewis RJ, Todorovic Sm, et al. Role of voltagegated calcium channels in ascending pain pathways. brain Res
Rev. 2009;60(1):84-9.
114. Todorovic Sm, Jevtovic-Todorovic v. The role of T-type calcium
channels in peripheral and central pain processing. CNS Neurol
disord drug Targets. 2006;5(6):639-53.
115. Felix R, Gurnett CA, de Waard m, et al. dissection of functional
domains of the voltage-dependent Ca2+ channel α2δ subunit. J
Neurosci. 1997;17(18):6884-91.
116. Newton RA, bingham S, Case PC, et al. dorsal root ganglion
neurons show increased expression of the calcium channel
[alpha]2[delta]-1 subunit following partial sciatic nerve injury.
mol brain Res. 2001;95(1-2):1-8.
117. luo Zd, Chaplan SR, higuera ES, et al. Upregulation of dorsal root
ganglion [alpha]2[delta] calcium channel subunit and its
correlation with allodynia in spinal nerve-injured rats. J
Neurosci. 2001;21(6):1868-75.
�lE JOURNAl CANAdiEN dES SCiENCES NEUROlOGiqUES
118. boroujerdi A, Kim hK, lyu YS, et al. injury discharges regulate
calcium channel alpha-2-delta-1 subunit upregulation in the
dorsal horn that contributes to initiation of neuropathic pain.
Pain. 2008;139(2):358-66.
119. luo Zd, Calcutt NA, higuera ES, et al. injury type-specific
calcium channel α2δ-1 subunit up-regulation in rat neuropathic
pain models correlates with antiallodynic effects of gabapentin.
J Pharmacol Exp Ther. 2002;303(3):1199-205.
120. Field mJ, Cox PJ, Stott E, et al. identification of the α2-δ-1 subunit
of voltage-dependent calcium channels as a molecular target for
pain mediating the analgesic actions of pregabalin. PNAS. 2006;
103(46):17537-42.
121. marais E, Klugbauer N, hofmann F. Calcium channel α2δ
subunits−structure and gabapentin binding. mol Pharmacol.
2001;59(5):1243-8.
122. Stefani A, Spadoni F, bernardi G. Gabapentin inhibits calcium
currents in isolated rat brain neurons. Neuropharmacology.
1998;37(1):83-91.
123. Gee NS, brown JP, dissanayake vUK, et al. The novel
anticonvulsant drug, gabapentin (Neurontin), binds to the
subunit of a calcium channel. J biol Chem. 1996;271(10):
5768-76.
124. Gutman GA, Chandy KG, Grissmer S, et al. international Union of
Pharmacology. liii. Nomenclature and molecular relationships
of voltage-gated potassium channels. Pharmacol Rev. 2005;57
(4):473-508.
125. Ocaña m, Cendán Cm, Cobos EJ, et al. Potassium channels and
pain: present realities and future opportunities. Eur J Pharmacol.
2004;500(1-3):203-19.
126. bayliss dA, barrett Pq. Emerging roles for two-pore-domain
potassium channels and their potential therapeutic impact.
Trends Pharmacol Sci. 2008;29(11):566-75.
127. lesage F, lazdunski m. molecular and functional properties of
two-pore-domain potassium channels. Am J Physiol Renal
Physiol. 2000;279(5):F793-801.
128. hibino h, inanobe A, Furutani K, et al. inwardly rectifying
potassium channels: their structure, function, and physiological
roles. Physiol Rev. 2010;90(1):291-366.
129. Pischalnikova A, Sokolova O. The domain and conformational
organization in potassium voltage-gated ion channels. J
Neuroimmune Pharmacol. 2009;4(1):71-82.
130. Ghatta S, Nimmagadda d, Xu X, et al. large-conductance,
calcium-activated potassium channels: structural and functional
implications. Pharmacol Ther. 2006;110(1):103-16.
131. Kostyuk PG, veselovsky NS, Fedulova SA, et al. ionic currents in
the somatic membrane of rat dorsal root ganglion neurons-iii.
Potassium currents. Neuroscience. 1981;6(12):2439-44.
132. Kameyama m. ionic currents in cultured dorsal root ganglion cells
from adult guinea pigs. J membr biol. 1983;72(3):195-203.
133. Kasai h, Kameyama m, Yamaguchi K, et al. Single transient K
channels in mammalian sensory neurons. biophys J. 1986;49(6):
1243-7.
134. Penner R, Petersen m, Pierau FK, et al. dendrotoxin: a selective
blocker of a non-inactivating potassium current in guinea-pig
dorsal root ganglion neurones. Pflugers Arch. 1986;407(4):
365-9.
135. Stansfeld CE, marsh SJ, halliwell Jv, et al. 4-Aminopyridine and
dendrotoxin induce repetitive firing in rat visceral sensory
neurones by blocking a slowly inactivating outward current.
Neurosci lett. 1986;64(3):299-304.
136. Stansfeld C, Feltz A. dendrotoxin-sensitive K+ channels in dorsal
root ganglion cells. Neurosci lett. 1988;93(1):49-55.
137. mcFarlane S, Cooper E. Kinetics and voltage dependence of A-type
currents on neonatal rat sensory neurons. J Neurophysiol. 1991;
66(4):1380-91.
138. Gold mS, Shuster mJ, levine Jd. Characterization of six voltagegated K+ currents in adult rat sensory neurons. J Neurophysiol.
1996;75(6):2629-46.
139. Yoshida S, matsumoto S. Effects of α-dendrotoxin on K+ currents
and action potentials in tetrodotoxin-resistant adult rat trigeminal
ganglion neurons. J Pharmacol Exp Ther. 2005;314(1):437-45.
140. Everill b, Rizzo mA, Kocsis Jd. morphologically identified
cutaneous afferent dRG neurons express three different
Volume 39, No. 4 – July 2012
potassium currents in varying proportions. J Neurophysiol.
1998;79(4):1814-24.
141. vydyanathan A, Wu ZZ, Chen SR, et al. A-type voltage-gated K+
currents influence firing properties of isolectin b4-positive but
not isolectin b4-negative primary sensory neurons. J
Neurophysiol. 2005;93(6):3401-9.
142. villiere v, mclachlan Em. Electrophysiological properties of
neurons in intact rat dorsal root ganglia classified by conduction
velocity and action potential duration. J Neurophysiol. 1996;76
(3):1924-41.
143. Connor JA, Stevens CF. voltage clamp studies of a transient
outward membrane current in gastropod neural somata. J
Physiol. 1971;213(1):21-30.
144. Catacuzzeno l, Fioretti b, Pietrobon d, et al. The differential
expression of low-threshold K+ currents generates distinct firing
patterns in different subtypes of adult mouse trigeminal ganglion
neurones. J Physiol. 2008;586(Pt 21):5101-18.
145. Gold mS, Shuster mJ, levine Jd. Role of a Ca(2+)-dependent slow
afterhyperpolarization in prostaglandin E2-induced sensitization
of cultured rat sensory neurons. Neurosci lett. 1996;205(3):
161-4.
146. Scholz A, Gruss m, vogel W. Properties and functions of calciumactivated K+ channels in small neurones of rat dorsal root
ganglion studied in a thin slice preparation. J Physiol. 1998;513
(Pt 1):55-69.
147. Zhang Xl, mok lP, Katz EJ, et al. bKCa currents are enriched in
a subpopulation of adult rat cutaneous nociceptive dorsal root
ganglion neurons. Eur J Neurosci. 2010;31(3):450-62.
148. Christian EP, Togo J, Naper KE. Guinea pig visceral C-fiber
neurons are diverse with respect to the K+ currents involved in
action-potential repolarization. J Neurophysiol. 1994;71(2):
561-74.
149. morita K, Katayama Y. Calcium-dependent slow outward current in
visceral primary afferent neurones of the rabbit. Pflugers Arch.
1989;414(2):171-7.
150. bahia PK, Suzuki R, benton dC, et al. A functional role for smallconductance calcium-activated potassium channels in sensory
pathways including nociceptive processes. J Neurosci. 2005;25
(14):3489-98.
151. Kaupp Ub, Seifert R. molecular diversity of pacemaker ion
channels. Annu Rev Physiol. 2001;63:235-57.
152. Santoro b, liu dT, Yao h, et al. identification of a gene encoding
a hyperpolarization-activated pacemaker channel of brain. Cell.
1998;93(5):717-29.
153. Ulens C, Tytgat J. Functional heteromerization of hCN1 and hCN2
pacemaker channels. J biol Chem. 2001;276(9):6069-72.
154. Orio P, madrid R, de la Peña E, et al. Characteristics and
physiological role of hyperpolarization activated currents in
mouse cold thermoreceptors. J Physiol. 2009;587(9):1961-76.
155. mayer ml, Westbrook Gl. A voltage-clamp analysis of inward
(anomalous) rectification in mouse spinal sensory ganglion
neurones. J Physiol. 1983;340:19-45.
156. Scroggs RS, Todorovic Sm, Anderson EG, et al. variation in ih,
iiR, and ilEAK between acutely isolated adult rat dorsal root
ganglion neurons of different size. J Neurophysiol. 1994;71(1):
271-9.
157. Pape hC. queer current and pacemaker: the hyperpolarizationactivated cation current in neurons. Annu Rev Physiol. 1996;58:
299-327.
158. Cho hj, Staikopoulos v, ivanusic J, et al. hyperpolarizationactivated cyclic-nucleotide gated 4 (hCN4) protein is expressed
in a subset of rat dorsal root and trigeminal ganglion neurons.
Cell Tissue Res. 2009;338(2):171-7.
159. Jiang Yq, Xing GG, Wang Sl, et al. Axonal accumulation of
hyperpolarization-activated cyclic nucleotide-gated cation
channels contributes to mechanical allodynia after peripheral
nerve injury in rat. Pain. 2008;137(3):495-506.
160. Tu h, deng l, Sun q, et al. hyperpolarization-activated, cyclic
nucleotide-gated cation channels: roles in the differential
electrophysiological properties of rat primary afferent neurons. J
Neurosci Res. 2004;76(5):713-22.
431
�ThE CANAdiAN JOURNAl OF NEUROlOGiCAl SCiENCES
161. Kouranova Ev, Strassle bW, Ring Rh, et al. hyperpolarizationactivated cyclic nucleotide-gated channel mRNA and protein
expression in large versus small diameter dorsal root ganglion
neurons: correlation with hyperpolarization-activated current
gating. Neuroscience. 2008;153(4):1008-19.
162. momin A, Cadiou h, mason A, et al. Role of the hyperpolarizationactivated current ih in somatosensory neurons. J Physiol. 2008;
586(Pt 24):5911-29.
163. viana F, belmonte C. Funny currents are becoming serious players
in nociceptor's sensitization. J Physiol. 2008;586(Pt 24):5841-2.
164. doubell TP, mannion JR, Woolf CJ. The dorsal horn: statedependent sensory processing, plasticity and the generation of
pain. in: Wall Pd, melzack R, editors. Textbook of pain.
london: harcourt Publishers limited; 1999. p. 165-81.
165. Rexed b. A cytoarchitectonic atlas of the spinal cord in the cat. J
Comp Neurol. 1954;100(2):297-379.
166. Rexed b. The cytoarchitectonic organization of the spinal cord in
the cat. J Comp Neurol. 1952;96(3):414-95.
167. brown AG, Rose PK, Snow PJ. The morphology of hair follicle
afferent fibre collaterals in the spinal cord of the cat. J Physiol.
1977;272(3):779-97.
168. brown AG, Rose PK, Snow PJ. morphology and organization of
axon collaterals from afferent fibres of slowly adapting type i
units in cat spinal cord. J Physiol. 1978;277:15-27.
169. brown AG, Fyffe RE, Noble R. Projections from Pacinian
corpuscles and rapidly adapting mechanoreceptors of glabrous
skin to the cat's spinal cord. J Physiol. 1980;307:385-400.
170. brown AG, Fyffe RE, Rose PK, et al. Spinal cord collaterals from
axons of type ii slowly adapting units in the cat. J Physiol. 1981;
316:469-80.
171. Woolf CJ. Central terminations of cutaneous mechanoreceptive
afferents in the rat lumbar spinal cord. J Comp Neurol. 1987;
261(1):105-19.
172. light AR, Trevino dl, Perl ER. morphological features of
functionally defined neurons in the marginal zone and substantia
gelatinosa of the spinal dorsal horn. J Comp Neurol. 1979;186
(2):151-71.
173. Sugiura Y, Terui N, hosoya Y. difference in distribution of central
terminals between visceral and somatic unmyelinated (C)
primary afferent fibers. J Neurophysiol. 1989;62(4):834-40.
174. Traub RJ, Solodkin A, Ruda mA. Calcitonin gene-related peptide
immunoreactivity in the cat lumbosacral spinal cord and the
effects of multiple dorsal rhizotomies. J Comp Neurol. 1989;287
(2):225-37.
175. Ribeiro-da-Silva A, Cuello AC. Organization of peptidergic neurons
in the dorsal horn of the spinal cord: anatomical and functional
correlates. Prog brain Res. 1995;104:41-59.
176. light AR, Perl ER. Spinal termination of functionally identified
primary afferent neurons with slowly conducting myelinated
fibers. J Comp Neurol. 1979;186(2):133-50.
177. Woolf CJ. Evidence for a central component of post-injury pain
hypersensitivity. Nature. 1983;306(5944):686-8.
178. Govrin-lippmann R, devor m. Ongoing activity in severed nerves:
source and variation with time. brain Res. 1978;159(2):406-10.
179. Wall Pd, devor m. Sensory afferent impulses originate from dorsal
root ganglia as well as from the periphery in normal and nerve
injured rats. Pain. 1983;17(4):321-39.
180. Kajander KC, Wakisaka S, bennett GJ. Spontaneous discharge
originates in the dorsal root ganglion at the onset of a painful
peripheral neuropathy in the rat. Neurosci lett. 1992;138(2):
225-8.
181. Kim Yi, Na hS, Kim Sh, et al. Cell type-specific changes of the
membrane properties of peripherally-axotomized dorsal root
ganglion neurons in a rat model of neuropathic pain.
Neuroscience. 1998;86(1):301-9.
182. Zhang Jm, donnelly dF, Song XJ, et al. Axotomy increases the
excitability of dorsal root ganglion cells with unmyelinated
axons. J Neurophysiol. 1997;78(5):2790-4.
183. Study RE, Kral mG. Spontaneous action potential activity in
isolated dorsal root ganglion neurons from rats with a painful
neuropathy. Pain. 1996;65(2-3):235-42.
432
184. ma C, lamotte Rh. Enhanced excitability of dissociated primary
sensory neurons after chronic compression of the dorsal root
ganglion in the rat. Pain. 2005;113(1-2):106-12.
185. Everill b, Cummins TR, Waxman SG, et al. Sodium currents of
large (Aβ-type) adult cutaneous afferent dorsal root ganglion
neurons display rapid recovery from inactivation before and after
axotomy. Neuroscience. 2001;106(1):161-9.
186. Cummins TR, Waxman SG. downregulation of tetrodotoxinresistant sodium currents and upregulation of a rapidly repriming
tetrodotoxin-sensitive sodium current in small spinal sensory
neurons after nerve injury. J Neurosci. 1997;17(10):3503-14.
187. Cummins TR, Aglieco F, Renganathan m, et al. Nav1.3 sodium
channels: rapid repriming and slow closed-state inactivation
display quantitative differences after expression in a mammalian
cell line and in spinal sensory neurons. J Neurosci. 2001;21(16):
5952-61.
188. Waxman SG, Kocsis Jd, black JA. Type iii sodium channel mRNA
is expressed in embryonic but not adult spinal sensory neurons,
and is reexpressed following axotomy. J Neurophysiol. 1994;72
(1):466-70.
189. dib-hajj S, black JA, Felts P, et al. down-regulation of transcripts
for Na channel α-SNS in spinal sensory neurons following
axotomy. PNAS. 1996;93(25):14950-4.
190. black JA, Cummins TR, Plumpton C, et al. Upregulation of a silent
sodium channel after peripheral, but not central, nerve injury in
dRG neurons. J Neurophysiol. 1999;82(5):2776-85.
191. dib-hajj Sd, Fjell J, Cummins TR, et al. Plasticity of sodium
channel expression in dRG neurons in the chronic constriction
injury model of neuropathic pain. Pain. 1999;83(3):591-600.
192. Kim Ch, Oh Y, Chung Jm, et al. The changes in expression of three
subtypes of TTX sensitive sodium channels in sensory neurons
after spinal nerve ligation. brain Res mol brain Res. 2001;95(12):153-61.
193. dib-hajj Sd, black JA, Cummins TR, et al. Rescue of alpha -SNS
sodium channel expression in small dorsal root ganglion neurons
after axotomy by nerve growth factor in vivo. J Neurophysiol.
1998;79(5):2668-76.
194. boucher TJ, Okuse K, bennett dl, et al. Potent analgesic effects of
GdNF in neuropathic pain states. Science. 2000;290(5489):
124-7.
195. Gold mS, Weinreich d, Kim CS, et al. Redistribution of Na(v)1.8
in uninjured axons enables neuropathic pain. J Neurosci. 2003;
23(1):158-66.
196. hildebrand mE, Smith Pl, bladen C, et al. A novel slowinactivation-specific ion channel modulator attenuates
neuropathic pain. Pain. 2011;152(4):833-43.
197. Everill b, Kocsis Jd. Reduction in potassium currents in identified
cutaneous afferent dorsal root ganglion neurons after axotomy. J
Neurophysiol. 1999;82(2):700-8.
198. Kim dS, Choi JO, Rim hd, et al. downregulation of voltage-gated
potassium channel [alpha] gene expression in dorsal root ganglia
following chronic constriction injury of the rat sciatic nerve. mol
brain Res. 2002;105(1-2):146-52.
199. Sarantopoulos Cd, mcCallum Jb, Rigaud m, et al. Opposing
effects of spinal nerve ligation on calcium-activated potassium
currents in axotomized and adjacent mammalian primary
afferent neurons. brain Res. 2007;1132(1):84-99.
200. boettger mK, Till S, Chen mX, et al. Calcium-activated potassium
channel SK1- and iK1-like immunoreactivity in injured human
sensory neurones and its regulation by neurotrophic factors.
brain. 2002;125(2):252-63.
201. baccei ml, Kocsis Jd. voltage-gated calcium currents in
axotomized adult rat cutaneous afferent neurons. J Neurophysiol.
2000;83(4):2227-38.
202. Jagodic mm, Pathirathna S, Joksovic Pm, et al. Upregulation of the
T-type calcium current in small rat sensory neurons after chronic
constrictive injury of the sciatic nerve. J Neurophysiol. 2008;
99(6):3151-6.
203. Jagodic mm, Pathirathna S, Nelson mT, et al. Cell-specific
alterations of T-type calcium current in painful diabetic
neuropathy enhance excitability of sensory neurons. J Neurosci.
2007;27(12):3305-16.
�lE JOURNAl CANAdiEN dES SCiENCES NEUROlOGiqUES
204. Titmus mJ, Faber dS. Axotomy-induced alterations in the
electrophysiological characteristics of neurons. Prog Neurobiol.
1990;35(1):1-51.
205. Charles P. mechanisms of analgesia by gabapentin and pregabalin
− calcium channel α2-δ[Cavα2-δ] ligands. Pain. 2009;142(12):13-16.
206. Schmidtko A, lötsch J, Freynhagen R, et al. Ziconotide for
treatment of severe chronic pain. lancet. 2010;375(9725):
1569-77.
207. Abdulla FA, Smith PA. Axotomy reduces the effect of analgesic
opioids yet increases the effect of nociceptin on dorsal root
ganglion neurons. J Neurosci. 1998;18(23):9685-94.
208. hori Y, Endo K, Takahashi T. Presynaptic inhibitory action of
enkephalin on excitatory transmission in superficial dorsal horn
of rat spinal cord. J Physiol. 1992;450(1):673-85.
209. Choe W, messinger Rb, leach E, et al. TTA-P2 is a potent and
selective blocker of T-type calcium channels in rat sensory
neurons and a novel antinociceptive agent. mol Pharmacol.
2011;80(5):900-10.
210. Todorovic Sm, Jevtovic-Todorovic v. T-type voltage-gated calcium
channels as targets for the development of novel pain therapies.
br J Pharmacol. 2011;163(3):484-95.
211. Yao h, donnelly dF, ma C, et al. Upregulation of the
hyperpolarization-activated cation current after chronic
compression of the dorsal root ganglion. J Neurosci. 2003;23(6):
2069-74.
212. Chaplan SR, Guo hq, lee dh, et al. Neuronal hyperpolarizationactivated pacemaker channels drive neuropathic pain. J
Neurosci. 2003;23(4):1169-78.
213. Emery EC, Young GT, berrocoso Em, et al. hCN2 ion channels
play a central role in inflammatory and neuropathic pain.
Science. 2011;333(6048):1462-6.
214. Takasu K, Ono h, Tanabe m. Spinal hyperpolarization-activated
cyclic nucleotide-gated cation channels at primary afferent
terminals contribute to chronic pain. Pain. 2010;151(1):87-96.
215. mclachlan Em, Janig W, devor m, et al. Peripheral nerve injury
triggers noradrenergic sprouting within dorsal root ganglia.
Nature. 1993;363(6429):543-6.
216. devor m, Janig W, michaelis m. modulation of activity in dorsal
root ganglion neurons by sympathetic activation in nerve-injured
rats. J Neurophysiol. 1994;71(1):38-47.
217. Sato J, Perl ER. Adrenergic excitation of cutaneous pain receptors
induced by peripheral nerve injury. Science. 1991;251(5001):
1608-10.
218. Petersen m, Zhang J, Zhang Jm, et al. Abnormal spontaneous
activity and responses to norepinephrine in dissociated dorsal
root ganglion cells after chronic nerve constriction. Pain. 1996;
67(2-3):391-7.
219. birder lA, Perl ER. Expression of α2-adrenergic receptors in rat
primary afferent neurones after peripheral nerve injury or
inflammation. J Physiol. 1999;515(2):533-42.
220. Abdulla FA, Smith PA. Ectopic alpha2-adrenoceptors couple to Ntype Ca2+ channels in axotomized rat sensory neurons. J
Neurosci. 1997;17(5):1633-41.
221. Amir R, devor m. Functional cross-excitation between afferent Aand C-neurons in dorsal root ganglia. Neuroscience. 1999;95(1):
189-95.
222. dalal A, Tata m, Allegre G, et al. Spontaneous activity of rat dorsal
horn cells in spinal segments of sciatic projection following
transection of sciatic nerve or of corresponding dorsal roots.
Neuroscience. 1999;94(1):217-28.
223. Woolf CJ, Thompson SW. The induction and maintenance of
central sensitization is dependent on N-methyl-d-aspartic acid
receptor activation; implications for the treatment of post-injury
pain hypersensitivity states. Pain. 1991;44(3):293-9.
224. Garraway Sm, Petruska JC, mendell lm. bdNF sensitizes the
response of lamina ii neurons to high threshold primary afferent
inputs. Eur J Neurosci. 2003;18(9):2467-76.
225. baba h, Ji RR, Kohno T, et al. Removal of GAbAergic inhibition
facilitates polysynaptic A fiber-mediated excitatory transmission
to the superficial spinal dorsal horn. mol Cell Neurosci. 2003;
24(3):818-30.
Volume 39, No. 4 – July 2012
226. Coull JA, boudreau d, bachand K, et al. Trans-synaptic shift in
anion gradient in spinal lamina i neurons as a mechanism of
neuropathic pain. Nature. 2003;424(6951):938-42.
227. balasubramanyan S, Stemkowski Pl, Stebbing mJ, et al. Sciatic
chronic constriction injury produces cell-type-specific changes
in the electrophysiological properties of rat substantia gelatinosa
neurons. J Neurophysiol. 2006;96(2):579-90.
228. Sivilotti l, Woolf CJ. The contribution of GAbAA and glycine
receptors to central sensitization: disinhibition and touch-evoked
allodynia in the spinal cord. J Neurophysiol. 1994;72(1):169-79.
229. Costigan m, Scholz J, Woolf CJ. Neuropathic pain: a maladaptive
response of the nervous system to damage. Annu Rev Neurosci.
2009;32:1-32.
230. Coull JA, beggs S, boudreau d, et al. bdNF from microglia causes
the shift in neuronal anion gradient underlying neuropathic pain.
Nature. 2005;438(7070):1017-21.
231. dougherty Kd, dreyfus CF, black ib. brain-derived neurotrophic
factor in astrocytes, oligodendrocytes, and microglia/
macrophages after spinal cord injury. Neurobiol dis. 2000;7(6 Pt
b):574-85.
232. lu vb, ballanyi K, Colmers WF, et al. Neuron type-specific effects
of brain-derived neurotrophic factor in rat superficial dorsal horn
and their relevance to 'central sensitization'. J Physiol. 2007;584
(Pt 2):543-63.
233. lu vb, biggs JE, Stebbing mJ, et al. brain-derived neurotrophic
factor drives the changes in excitatory synaptic transmission in
the rat superficial dorsal horn that follow sciatic nerve injury. J
Physiol. 2009;587(Pt 5):1013-32.
234. Prescott SA, Sejnowski TJ, de Koninck Y. Reduction of anion
reversal potential subverts the inhibitory control of firing rate in
spinal lamina i neurons: towards a biophysical basis for
neuropathic pain. mol Pain. 2006;2:32.
235. Kerr bJ, bradbury EJ, bennett dl, et al. brain-derived
neurotrophic factor modulates nociceptive sensory inputs and
NmdA-evoked responses in the rat spinal cord. J Neurosci.
1999;19(12):5138-48.
236. Ulmann l, hatcher JP, hughes JP, et al. Up-regulation of P2X4
receptors in spinal microglia after peripheral nerve injury
mediates bdNF release and neuropathic pain. J Neurosci. 2008;
28(44):11263-8.
237. Scholz J, Woolf CJ. The neuropathic pain triad: neurons, immune
cells and glia. Nat Neurosci. 2007;10(11):1361-8.
238. devor m. Ectopic discharge in A beta afferents as a source of
neuropathic pain. Exp brain Res. 2009;196(1):115-28.
239. Gaudet A, Popovich P, Ramer m. Wallerian degeneration: gaining
perspective on inflammatory events after peripheral nerve injury.
J Neuroinflammation. 2011;8(1):110.
240. Kelley J. Reactions of neurons to injury. in: Kandel ER, Schwartz
Jh, editors. Principles of neural science. New York: Elsevier
Science Publishings Co., inc. 1985. p. 187-95.
241. ma C, Shu Y, Zheng Z, et al. Similar electrophysiological changes
in axotomized and neighboring intact dorsal root ganglion
neurons. J Neurophysiol. 2003;89(3):1588-602.
242. mosconi T, Kruger l. Fixed-diameter polyethylene cuffs applied to
the rat sciatic nerve induce a painful neuropathy: ultrastructural
morphometric analysis of axonal alterations. Pain. 1996;64(1):
37-57.
243. Jones GJ, barsby Nl, Cohen EA, et al. hiv-1 vpr causes neuronal
apoptosis and in vivo neurodegeneration. J Neurosci. 2007;27
(14):3703-11.
244. Acharjee S, Noorbakhsh F, Stemkowski Pl, et al. hiv-1 viral
protein R causes peripheral nervous system injury associated
with in vivo neuropathic pain. FASEb J. 2010;24(11):4343-53.
245. Tsao JW, George Eb, Griffin JW. Temperature modulation reveals
three distinct stages of Wallerian degeneration. J Neurosci. 1999;
19(12):4718-26.
246. luttges mW, Kelly PT, Gerren RA. degenerative changes in mouse
sciatic nerves: electrophoretic and electrophysiologic
characterizations. Exp Neurol. 1976;50(3):706-33.
247. Perrin FE, lacroix S, Aviles-Trigueros m, et al. involvement of
monocyte chemoattractant protein-1, macrophage inflammatory
protein-1alpha and interleukin-1beta in Wallerian degeneration.
brain. 2005;128(Pt 4):854-66.
433
�ThE CANAdiAN JOURNAl OF NEUROlOGiCAl SCiENCES
248. Wells mR, vaidya U. morphological alterations in dorsal root
ganglion neurons after peripheral axon injury: association with
changes in metabolism. Exp Neurol. 1989;104(1):32-8.
249. Sorkin lS, Schafers m. immune cells in peripheral nerve. in:
deleo JA, Sorkin lS, Watkins lR, editors. immune and glia
regulation of pain. Seattle: iASP Press; 2007. p. 3-19.
250. Xie WR, deng h, li h, et al. Robust increase of cutaneous
sensitivity, cytokine production and sympathetic sprouting in
rats with localized inflammatory irritation of the spinal ganglia.
Neuroscience. 2006;142(3):809-22.
251. Okuda T, ishida O, Fujimoto Y, et al. The autotomy relief effect of
a silicone tube covering the proximal nerve stump. J Orthop Res.
2006;24(7):1427-37.
252. Zuo Y, Perkins Nm, Tracey dJ, et al. inflammation and
hyperalgesia induced by nerve injury in the rat: a key role of
mast cells. Pain. 2003;105(3):467-79.
253. Perkins Nm, Tracey dJ. hyperalgesia due to nerve injury: role of
neutrophils. Neuroscience. 2000;101(3):745-57.
254. Cui JG, holmin S, mathiesen T, et al. Possible role of inflammatory
mediators in tactile hypersensitivity in rat models of
mononeuropathy. Pain. 2000;88(3):239-48.
255. moore KA, Kohno T, Karchewski lA, et al. Partial peripheral nerve
injury promotes a selective loss of GAbAergic inhibition in the
superficial dorsal horn of the spinal cord. J Neurosci. 2002;22
(15):6724-31.
256. Chen Y, balasubramanyan S, lai AY, et al. Effects of sciatic nerve
axotomy on excitatory synaptic transmission in rat substantia
gelatinosa. J Neurophysiol. 2009;102(6):3203-15.
257. Tominaga m, Caterina mJ, malmberg Ab, et al. The cloned
capsaicin receptor integrates multiple pain-producing stimuli.
Neuron. 1998;21(3):531-43.
258. Chen CC, Akopian AN, Sivilotti l, et al. A P2X purinoceptor
expressed by a subset of sensory neurons. Nature. 1995;377
(6548):428-31.
259. Chen CC, England S, Akopian AN, et al. A sensory neuron-specific,
proton-gated ion channel. PNAS. 1998;95(17):10240-5.
260. Nakamura-Craig m, Gill bK. Effect of neurokinin A, substance P
and calcitonin gene related peptide in peripheral hyperalgesia in
the rat paw. Neurosci lett. 1991;124(1):49-51.
261. Carlton Sm, Zhou S, Coggeshall RE. localization and activation of
substance P receptors in unmyelinated axons of rat glabrous skin.
brain Res. 1996;734(1-2):103-8.
262. dray A, Pinnock Rd. Effects of substance P on adult rat sensory
ganglion neurones in vitro. Neurosci lett. 1982;33(1):61-6.
263. Abdulla FA, Stebbing mJ, Smith PA. Effects of substance P on
excitability and ionic currents of normal and axotomized rat
dorsal root ganglion neurons. Eur J Neurosci. 2001;13(3):
545-52.
264. li hS, Zhao Zq. Small sensory neurons in the rat dorsal root
ganglia express functional NK-1 tachykinin receptor. Eur J
Neurosci. 1998;10(4):1292-9.
265. Yonehara N, Yoshimura m. influence of painful chronic neuropathy
on neurogenic inflammation. Pain. 2001;92(1-2):259-65.
266. Cahill Cm, Coderre TJ. Attenuation of hyperalgesia in a rat model
of neuropathic pain after intrathecal pre- or post-treatment with
a neurokinin-1 antagonist. Pain. 2002;95(3):277-85.
267. lee SE, Kim Jh. involvement of substance P and calcitonin generelated peptide in development and maintenance of neuropathic
pain from spinal nerve injury model of rat. Neurosci Res. 2007;
58(3):245-9.
268. Jang Jh, Nam TS, Paik KS, et al. involvement of peripherally
released substance P and calcitonin gene-related peptide in
mediating mechanical hyperalgesia in a traumatic neuropathy
model of the rat. Neurosci lett. 2004;360(3):129-32.
269. herzberg U, Eliav E, dorsey Jm, et al. NGF involvement in pain
induced by chronic constriction injury of the rat sciatic nerve.
Neuroreport. 1997;8(7):1613-18.
270. Zhou XF, deng YS, Chie E, et al. Satellite-cell-derived nerve
growth factor and neurotrophin-3 are involved in noradrenergic
sprouting in the dorsal root ganglia following peripheral nerve
injury in the rat. Eur J Neurosci. 1999;11(5):1711-22.
434
271. Ro lS, Chen ST, Tang lm, et al. Effect of NGF and anti-NGF on
neuropathic pain in rats following chronic constriction injury of
the sciatic nerve. Pain. 1999;79(2-3):265-74.
272. Chuang hh, Prescott Ed, Kong h, et al. bradykinin and nerve
growth factor release the capsaicin receptor from Ptdins(4,5)P2mediated inhibition. Nature. 2001;411(6840):957-62.
273. Shu X, mendell lm. Acute sensitization by NGF of the response of
small-diameter sensory neurons to capsaicin. J Neurophysiol.
2001;86(6):2931-8.
274. Ji RR, Samad TA, Jin SX, et al. p38 mAPK activation by NGF in
primary sensory neurons after inflammation increases TRPv1
levels and maintains heat hyperalgesia. Neuron. 2002;36(1):
57-68.
275. Zhang Yh, Nicol Gd. NGF-mediated sensitization of the
excitability of rat sensory neurons is prevented by a blocking
antibody to the p75 neurotrophin receptor. Neurosci lett. 2004;
366(2):187-92.
276. Zhang Yh, vasko mR, Nicol Gd. Ceramide, a putative second
messenger for nerve growth factor, modulates the TTX-resistant
Na+ current and delayed rectifier K+ current in rat sensory
neurons. J Physiol. 2002;544(2):385-402.
277. Amadesi S, Nie J, vergnolle N, et al. Protease-activated receptor 2
sensitizes the capsaicin receptor transient receptor potential
vanilloid receptor 1 to induce hyperalgesia. J Neurosci. 2004;24
(18):4300-12.
278. linley JE, Rose K, Patil m, et al. inhibition of m current in sensory
neurons by exogenous proteases: a signaling pathway mediating
inflammatory nociception. J Neurosci. 2008;28(44):11240-9.
279. Alier KA, Endicott JA, Stemkowski Pl, et al. intrathecal
administration of proteinase-activated receptor-2 agonists
produces hyperalgesia by exciting the cell bodies of primary
sensory neurons. J Pharmacol Exp Ther. 2008;324(1):224-33.
280. Kress m, Guenther S. Role of [Ca2+]i in the ATP-induced heat
sensitization process of rat nociceptive neurons. J Neurophysiol.
1999;81(6):2612-19.
281. Tominaga m, Wada m, masu m. Potentiation of capsaicin receptor
activity by metabotropic ATP receptors as a possible mechanism
for ATP-evoked pain and hyperalgesia. PNAS. 2001;98(12):
6951-6.
282. Cesare P, mcNaughton P. A novel heat-activated current in
nociceptive neurons and its sensitization by bradykinin. PNAS.
1996;93(26):15435-9.
283. dai Y, Wang S, Tominaga m, et al. Sensitization of TRPA1 by PAR2
contributes to the sensation of inflammatory pain. J Clin invest.
2007;117(7):1979-87.
284. Cenac N, Andrews CN, holzhausen m, et al. Role for protease
activity in visceral pain in irritable bowel syndrome. J Clin
invest. 2007;117(3):636-47.
285. Salmon JA, higgs GA. Prostaglandins and leukotrienes as
inflammatory mediators. br med bull. 1987;43(2):285-96.
286. Kiefer W, dannhardt G. COX-2 inhibition and pain management: a
review summary. Expert Rev Clin immunol. 2005;1(3):431-42.
287. Ferreira Sh, Nakamura m, de Abreu Castro mS. The hyperalgesic
effects of prostacyclin and prostaglandin E2. Prostaglandins.
1978;16(1):31-7.
288. higgs EA, moncada S, vane JR. inflammatory effects of
prostacyclin (PGi2) and 6-oxo-PGF1[alpha] in the rat paw.
Prostaglandins. 1978;16(2):153-62.
289. Schepelmann K, linger K, Schaible hG, et al. inflammatory
mediators and nociception in the joint: Excitation and
sensitization of slowly conducting afferent fibers of cat's knee by
prostaglandin i2. Neuroscience. 1992;50(1):237-47.
290. birrell GJ, mcqueen dS, iggo A, et al. PGi2-induced activation
and sensitization of articular mechanonociceptors. Neurosci lett.
1991;124(1):5-8.
291. devor m, White dm, Goetzl EJ, et al. Eicosanoids, but not
tachykinins, excite C-fiber endings in rat sciatic nerve-end
neuromas. Neuroreport. 1992;3(1):21-4.
292. Oida h, Namba T, Sugimoto Y, et al. in situ hybridization studies of
prostacyclin receptor mRNA expression in various mouse
organs. br J Pharmacol. 1995;116(7):2828-37.
�lE JOURNAl CANAdiEN dES SCiENCES NEUROlOGiqUES
293. Sugimoto Y, Shigemoto R, Namba T, et al. distribution of the
messenger RNA for the prostaglandin e receptor subtype ep3 in
the mouse nervous system. Neuroscience. 1994;62(3):919-28.
294. matsumura K, Watanabe Y, Onoe h, et al. Prostacyclin receptor in
the brain and central terminals of the primary sensory neurons:
an autoradiographic study using a stable prostacyclin analogue
[3h]iloprost. Neuroscience. 1995;65(2):493-503.
295. Schaible hG, Schmidt RF. Excitation and sensitization of fine
articular afferents from cat's knee joint by prostaglandin E2. J
Physiol. 1988;403:91-104.
296. Nicol Gd, Cui m. Enhancement by prostaglandin E2 of bradykinin
activation of embryonic rat sensory neurones. J Physiol. 1994;
480(Pt 3):485-92.
297. Nicol Gd, vasko mR, Evans AR. Prostaglandins suppress an
outward potassium current in embryonic rat sensory neurons. J
Neurophysiol. 1997;77(1):167-76.
298. devor m, Govrin-lippmann R, Angelides K. Na+ channel
immunolocalization in peripheral mammalian axons and
changes following nerve injury and neuroma formation. J
Neurosci. 1993;13(5):1976-92.
299. Gold mS, Reichling db, Shuster mJ, et al. hyperalgesic agents
increase a tetrodotoxin-resistant Na+ current in nociceptors.
PNAS. 1996;93(3):1108-12.
300. Gold mS, levine Jd. dAmGO inhibits prostaglandin E2-induced
potentiation of a TTX-resistant Na+ current in rat sensory
neurons in vitro. Neurosci lett. 1996;212(2):83-6.
301. Khasar SG, Gold mS, levine Jd. A tetrodotoxin-resistant sodium
current mediates inflammatory pain in the rat. Neurosci lett.
1998;256(1):17-20.
302. ingram Sl, Williams JT. modulation of the hyperpolarizationactivated current (ih) by cyclic nucleotides in guinea-pig
primary afferent neurons. J Physiol. 1996;492 (Pt 1):97-106.
303. moriyama T, higashi T, Togashi K, et al. Sensitization of TRPv1
by EP1 and iP reveals peripheral nociceptive mechanism of
prostaglandins. mol Pain. 2005;1(1):3.
304. Taiwo YO, levine Jd. Characterization of the arachidonic acid
metabolites mediating bradykinin and noradrenaline
hyperalgesia. brain Res. 1988;458(2):402-6.
305. Sommer C, Kress m. Recent findings on how proinflammatory
cytokines cause pain: peripheral mechanisms in inflammatory
and neuropathic hyperalgesia. Neurosci lett. 2004;361(1-3):
184-7.
306. leung l, Cahill Cm. TNF-alpha and neuropathic pain--a review. J
Neuroinflammation. 2010;7:27.
307. Copray JC, mantingh i, brouwer N, et al. Expression of interleukin1 beta in rat dorsal root ganglia. J Neuroimmunol. 2001;118
(2):203-11.
308. liu l, Yang Tm, liedtke W, et al. Chronic il-1beta signaling
potentiates voltage-dependent sodium currents in trigeminal
nociceptive neurons. J Neurophysiol. 2006;95(3):1478-90.
309. binshtok Am, Wang h, Zimmermann K, et al. Nociceptors are
interleukin-1beta sensors. J Neurosci. 2008;28(52):14062-73.
310. Takeda m, Tanimoto T, Kadoi J, et al. Enhanced excitability of
nociceptive trigeminal ganglion neurons by satellite glial
cytokine following peripheral inflammation. Pain. 2007;129(12):155-66.
Volume 39, No. 4 – July 2012
311. Nadeau S, Filali m, Zhang J, et al. Functional recovery after
peripheral nerve injury is dependent on the pro-inflammatory
cytokines il-1β and TNF: implications for neuropathic pain. J
Neurosci. 2011;31(35):12533-42.
312. Rotshenker S, Aamar S, barak v. interleukin-1 activity in lesioned
peripheral nerve. J Neuroimmunol. 1992;39(1-2):75-80.
313. Kawasaki Y, Xu ZZ, Wang X, et al. distinct roles of matrix
metalloproteases in the early- and late-phase development of
neuropathic pain. Nat med. 2008;14(3):331-6.
314. Stemkowski Pl, Smith PA. long-term il-1β exposure causes
subpopulation dependent alterations in rat dorsal root ganglion
neuron excitability. J Neurophysiol. 2012;107:1586-97.
315. Temporin K, Tanaka h, Kuroda Y, et al. interleukin-1 beta promotes
sensory nerve regeneration after sciatic nerve injury. Neurosci
lett. 2008;440(2):130-3.
316. Temporin K, Tanaka h, Kuroda Y, et al. il-1[beta] promotes neurite
outgrowth by deactivating RhoA via p38 mAPK pathway.
biochem biophys Res Commun. 2008;365(2):375-80.
317. horie h, Sakai i, Akahori Y, et al. il-1 beta enhances neurite
regeneration from transected-nerve terminals of adult rat dRG.
Neuroreport. 1997;8(8):1955-9.
318. Sommer C, myers RR. Neurotransmitters in the spinal cord dorsal
horn in a model of painful neuropathy and in nerve crush. Acta
Neuropathol. 1995;90(5):478-85.
319. marchand JE, Wurm Wh, Kato T, et al. Altered tachykinin
expression by dorsal root ganglion neurons in a rat model of
neuropathic pain. Pain. 1994;58(2):219-31.
320. bennett Ad, Chastain Km, hulsebosch CE. Alleviation of
mechanical and thermal allodynia by CGRP(8-37) in a rodent
model of chronic central pain. Pain. 2000;86(1-2):163-75.
321. baranowski AP, Priestley Jv, mcmahon S. Substance P in
cutaneous primary sensory neurons--a comparison of models of
nerve injury that allow varying degrees of regeneration.
Neuroscience. 1993;55(4):1025-36.
322. Noguchi K, dubner R, de leon m, et al. Axotomy induces
preprotachykinin gene expression in a subpopulation of dorsal
root ganglion neurons. J Neurosci Res. 1994;37(5):596-603.
323. Noguchi K, Kawai Y, Fukuoka T, et al. Substance P induced by
peripheral nerve injury in primary afferent sensory neurons and
its effect on dorsal column nucleus neurons. J Neurosci. 1995;15
(11):7633-43.
324. michael GJ, Averill S, Nitkunan A, et al. Nerve growth factor
treatment increases brain-derived neurotrophic factor selectively
in TrkA-expressing dorsal root ganglion cells and in their central
terminations within the spinal cord. J Neurosci. 1997;17(21):
8476-90.
325. Tonra JR, Curtis R, Wong v, et al. Axotomy upregulates the
anterograde transport and expression of brain-derived
neurotrophic factor by sensory neurons. J Neurosci. 1998;18
(11):4374-83.
435
�
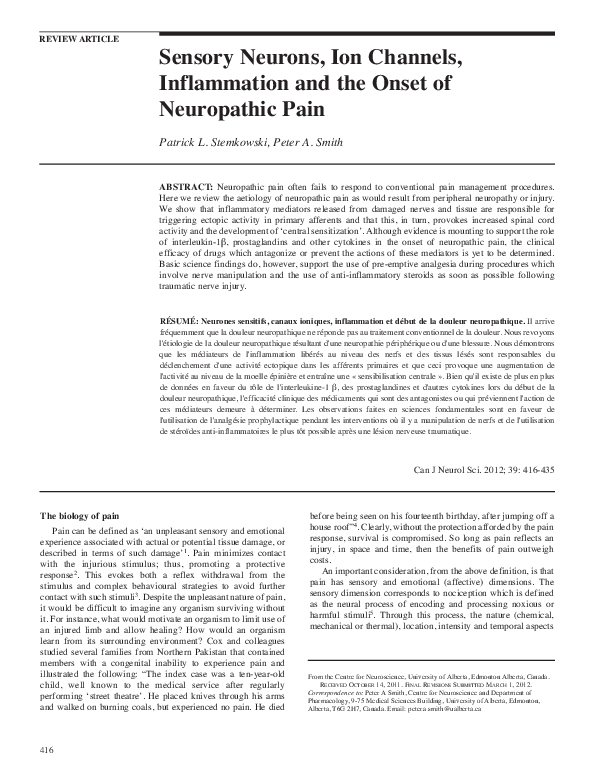
 peter smith
peter smith