VECTOR-BORNE AND ZOONOTIC DISEASES
Volume 10, Number 10, 2010
ª Mary Ann Liebert, Inc.
DOI: 10.1089=vbz.2009.0072
Temporal Variation in the Susceptibility
of Culex tritaeniorhynchus (Diptera: Culicidae)
to Japanese Encephalitis Virus in an Endemic Area
of Tamil Nadu, South India
Pauiraj Philip Samuel, Natarajan Arunachalam, Rathinasamy Rajendran,
Soosaimanickam Victor Jerold Leo, Krishnan Ayanar,
Ramakrishnan Balasubramaniam, and Brij Kishore Tyagi
Abstract
The study area, Cuddalore, is one of the endemic districts for Japanese encephalitis ( JE) in southern India and
there is a strong seasonality in JE case incidence, as well as JE virus ( JEV) infection in the principal vector Culex
(Culex) tritaeniorhynchus Giles. In a longitudinal 3-year study ( July 2003 to June 2006), we determined the
susceptibility of wild-caught female Cx. tritaeniorhynchus for JEV infection over several seasons from several
villages. The susceptibility varied in all four seasons with the lowest value (4.82 geometric mean [GM]) in hot
and wet seasons and highest (13.22 GM) in cool and wet seasons. Infection rate was significant between seasons
(7.08–11.85 GM) and years (4.82–13.22 GM). Although the vector was abundant throughout the year, with an
average per man-hour density ranging from 58 to 652, the JEV infection rates showed no correlation with vector
abundance during different seasons in the index villages. The temporal and spatial changes in the competency of
the vector appeared to influence the JEV infection rate in vector, which may at least partially explain the
seasonality in JEV human cases in the study area.
Key Words: Cx. tritaeniorhynchus—Japanese encephalitis virus—Susceptibility—Vector competence.
Introduction
J
apanese encephalitis virus ( JEV) is an important
pediatric public health problem in India, producing devastating epidemics in different parts of the country, particularly northeastern region of Assam and Gorakhpur areas
(Kanojia et al. 2003, Srivastava et al. 2003). Epidemics occur
annually and affect mainly lower socioeconomic rural communities (Reuben and Gajanana 1997, Kanojia et al. 2003).
The case fatality rate ranged from 40% to 60%, and about
30% of those who survive have sequellae, which cause great
financial burden to families (Kumar 1988, Solomon and
Vaughn 2002). In southern India in Tamil Nadu state, the
Cuddalore district is relatively dry, but an extensive epidemic occurred in 1981 and since then the disease has remained endemic with annual cases of encephalitis occurring
each year (Gajanana 1998). Entomological investigations
have shown that Culex (Culex) tritaeniorhynchus Giles,
Cx. (Cux.) vishnui Theobald, Cx. (Cux.) gelidus Theobald, and
Cx. (Cux.) fuscocephala Theobald constitute 93.6% of total
catch, of which the former species was the predominant and
principal vector of JEV (Reuben et al. 1994, Gajanana et al.
1997). In southern India, the largest number of JEV isolations
had been made from Cx. tritaeniorhynchus (Reuben et al. 1988
1994, Philip Samuel et al. 2000). JE case incidence showed a
strong seasonality, most of the cases being recorded during
the months of October and November. Virus infection in
vector mosquitoes also showed a very specific seasonal
pattern and the timing of appearance appears to be very
specific. Vector infection rate is an important parameter for
quantifying the transmission potential of specific vectors and
the risk of transmission to humans (Gajanana 1998). Therefore, we examined the seasonal variation of virus infection in
an endemic area, Cuddalore district, looking for any environmental or biological factor that may influence the pattern
of transmission. Vector competency of a species should be
Centre for Research in Medical Entomology, Indian Council of Medical Research, Madurai, Tamil Nadu, India.
1003
�1004
evaluated in different seasons and years to understand its
potential to act as a vector.
Materials and Methods
Study area
Our study area, the Cuddalore district of Tamil Nadu, is
endemic for JEV (latitude 11.75 N and longitude 79.75 E).
Most of the villages of this district are encircled mainly with
rice and sugarcane fields and inhabited by farmers and
agricultural laborers. In addition to cattle, the villagers
also rear pigs and fowl. A total of eight villages in four
blocks (villages=block), namely Nallur Block—S.S. Puram
and Kodikkalam, Mangalore Block—Avinangudi and
Pothiramangalam, Vridhachalam Block—Alichikudi and
Sathukudal, and Kammapuram Block—Ko. Adhanur and V.
Kumaramangalam, were selected for this study. Meteorological data showed that the maximum and minimum temperatures ranged from 328C to 398C and 208C to 288C,
respectively. The annual rainfall ranged from 0 to 254 mm
and relative humidity (RH) ranged between 85% and 92%
during the study period. Many of the villages receive irrigation water through the high-level channel from a reservoir, Wellington, where generally farmers raise two rice crops
in a year, beginning in June. The villages that are irrigated
through the low-level channel lie in the single cropping zone,
where a single long-term rice crop is grown, beginning in
September=October.
Viral assay
The virus stock used throughout the study was from a
single stock. Twenty percentage of mouse brain JEV suspension in 10�3 dilution of the Vellore strain (1958) of India
(P20778) passage level P14 in mice was used throughout the
study. This 20% JEV mouse brain suspension was serially
diluted 10-fold (10�3) with fowl blood and used for oral
feeding to Cx. tritaeniorhynchus. The titer of the 20% mouse
brain suspension was 106 tissue culture infection dose per
milliliter. Chickens used in this study were maintained in a
well-protected area free from natural infection. They were
periodically tested to find out the infection level.
Mosquito collection
For the susceptibility test in the laboratory, adult female
mosquitoes resting nearby cattle sheds and pigsties were
collected during dusk hours from the study villages. These
collections were repeated during different seasons, namely,
hot and wet season ( July–September), cool and wet season
(October–December), cool and dry season ( January–March),
and hot and dry season (April–June). All these mosquitoes were identified and sorted to species level and only Cx.
tritaeniorhynchus females were used for the infection experiment. Vector density was recorded as females per man hour
(PMH). For each season, 800 female mosquitoes (100 specimens from the eight index villages) were infected and tested.
Feeding experiments
Adults of Cx. tritaeniorhynchus females were held in Barraud cages at room temperature of 298C � 18C and 80% � 5%
RH throughout. Water-soaked raisins and cotton pledgets
PHILIP SAMUEL ET AL.
soaked in 1% glucose solution were provided as food. These
female mosquitoes were starved for 16–18 h before feeding on
JEV blood mixture sweetened with 1% sucrose from cotton
pledgets. Female fed on normal blood (uninfected fowl) were
kept as control. After feeding, we segregated the fully fed Cx.
tritaeniorhynchus mosquitoes. Viremic blood-fed mosquitoes
were carefully maintained in the laboratory for 12–14 days at
298C � 18C and 80% � 5% RH throughout and the watersoaked raisins were provided as food. Special precautions
were taken for holding infected mosquitoes in the specially
designed mosquito proof cages.
Screening of mosquitoes
Each female specimen was assayed individually for virus
content using enzyme-linked immunosorbant assay (ELISA).
All blood-fed female specimens were kept individually in
microcentrifuge tubes and were triturated in chilled 0.75%
bovine albumin phosphate saline (pH 7.4) containing antibiotics (1000 units of penicillin and 2 mg of streptomycin per
milliliter). Each mosquito suspension was subjected to two
cycles of freezing and thawing and centrifuged at 10,000 rpm
for 1 h, and the supernatant was used for screening by ELISA
on the same day. Monoclonal antibody, 6B4A-10 (reactive
against all the viruses in the JE=WN=SLE=MVE complex), was
used as capture antibody and the captured antigen from the
test sample was detected by detector monoclonal antibody
peroxidase conjugate, SLE MAB 6B6C-1 (Division of VectorBorne Infectious Diseases, CDC, Fort Collins, CO), reactive
against all flaviviruses. A mosquito sample is considered
positive for flavivirus antigen if its optical density is equal to
or greater than mean þ 4 standard deviations of optical density of uninfected laboratory mosquitoes (Gajanana et al. 1995,
1997).
Statistical analysis
The infection rate (IR) is expressed as the percentage of Cx.
tritaeniorhynchus females under examination in the feeding
series found to contain JEV (Philip Samuel et al. 1998).
IR ¼
Number of infected females
· 100
Total females tested
The experiments were conducted in a similar fashion in the
same place without any detectable variations. These experiments were conducted in different seasons in the same place,
using same strains present in those areas, during same period,
and using the same stock of the viral strain. Both chi-square
test and analysis of variance were carried out using SPSS-15.0
version (Tewari et al. 2008).
Results
The susceptibility of Cx. tritaeniorhynchus to JEV, based
on IRs, was lower in the hot and wet season during July–
September (2%–8%) and increased subsequently to 10.3%–21%
in the following cool and wet season during October–December.
Again the IR in the next season, cool and dry during
January–March, decreased to 4.8%–14% and showed an increase during the hot and dry (April–June) season (10.5%–
16.8%; Table 1). Susceptibility of Cx. tritaeniorhynchus to JEV
from different geographical locations of the study areas (eight
�SUSCEPTIBILITY STATUS OF Culex tritaeniorhynchus OF JEV
1005
Table 1. Seasonal Variation in the Infection Rates of Culex tritaeniorhynchus During the Study Period
Infection rate (%)
S. No.
1
2
3
4
Season (month)=year
(2003–2004)
(2004–2005)
(2005–2006)
GM
w2 (chi-square)
p-Value
Hot and wet ( July–Sep)
Cool and wet (Oct–Dec)
Cool and dry ( Jan–Mar)
Hot and dry (April–June)
GM
w2
p-Value
7.5
10.3
4.8
10.5
7.27
2.7
0.44
2.0
21.0
5.5
12.3
7.08
85.17
0.00001
8.0
11.4
14.0
16.8
11.85
43.46
0.00001
4.82
13.22
6.54
12.43
4.4
30.52
32.02
11.23
0.111
0.00001
0.00001
0.004
GM, geometric mean.
index villages) in almost all seasons in 3 years (2003–2006)
showed significant difference ( p < 0.05), except for one season, cool–dry 2006 ( p > 0.05). Infection rate between seasons
within different villages and years also showed significant
variation ( p < 0.05; Table 2).
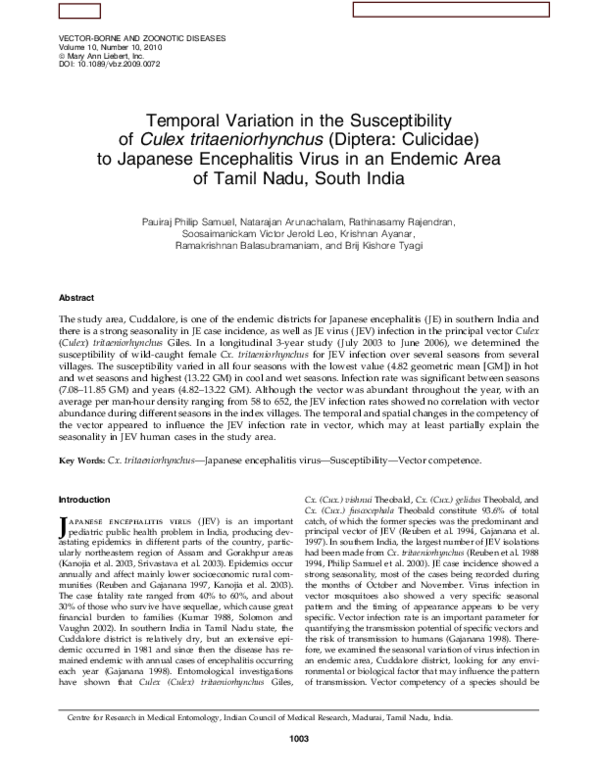
The vector density of Cx. tritaeniorhynchus in PMH was
recorded seasonwise during dusk collections from July–
September 2003 to April–June 2006 (Fig. 1). The IRs obtained
during the different seasons showed no correlation with the
abundance of the vector in the index villages, which ranged
from 58.61 to 652.2 PMH.
Pearson correlation coefficient was evaluated to assess the
relationship between the independent (maximum temperature, minimum temperature, and humidity) and dependent
variables (PMH density and IR). We have also checked for
normality of the variables using one-sample Kolmogorov–
Smirnov test and found that the data were normally distributed. As the data follow normal distribution, there is no need
for transformation. Multiple linear regressions between IR
and all the other meteorological data yielded a multiple correlation coefficient (r2 ¼ 0.20) showing poor relationship.
When the dependent variable was PMH density, a negative
correlation exists with maximum temperature (r ¼ �0.634,
p ¼ 0.027) and minimum temperature (r ¼ �0.728, p ¼ 0.007),
but we did not find any correlation when the dependent
variable was IR. The IR showed no correlation with PMH
density (r ¼ 0.012, p < 0.970), rainfall (r ¼ 0.147, p < 0.648),
humidity (r ¼ �0.065, p < 0.842), maximum temperature
(r ¼ 0.073, p < 0.822), and minimum temperature (r ¼ �0.25,
p < 0.433) (Table 3).
Discussion
In this study, we demonstrated that JEV can infect wildcaught Cx. tritaeniorhynchus females, but the rates vary
temporally and geographically. These findings on vector
competence help elucidate the transmission pattern of JEV in
India, which was similar to other studies using different
vectors=arboviruses (Hardy et al. 1979, Hayes et al. 1984,
Reisen et al. 1996). In previous vector competence studies in
India, most with JEV were limited to only one season and a
relatively small sample size with vectors, ranging from 2 to 7
females (Banerjee et al. 1978, 1984). In contrast, our investigation was over four consecutive seasons, included a much
larger sample size (100–800) of the principal JE vector, and
evaluated relatively small-scale spatial variations from different locations within a JE endemic district. The sample size
used in this study was comparable with similar studies conducted in other countries (Freier and Grimstad 1983, Reisen
et al. 1996).
Table 2. Comparison of Culex tritaeniorhynchus Susceptibility to Japanese Encephalitis Virus in Index
Villages (Between Villages–Within a Season and Between Seasons–Within a Village)
Infection rate (%)
Cool–wet Cool–dry Hot–dry Hot–wet Cool–wet Cool–dry Hot–dry
S. No. Villages=season=year
2004
2005
2005
2005
2005
2006
2006
w2 (chi-square)a
p-Value
1
S.S. Puram
2
Kodikkalam
3
Avinangudi
4
Pothiramangalam
5
Alichikudi
6
Sathukudal
7
Ko. Adhanur
8
Kumaramangalam
2
w (chi-square)b
p-Value
4
4
13
17
22
48
35
25
96.44
0.00001
8
13
26
8
0
0
0
0
92.92
0.00001
23
3
0
4
5
4
19
29
87.79
0.00001
6
15
4
8
4
3
13
8
19.01
0.01
24
18
1
7
4
13
17
7
43.44
0.00001
19
8
10
14
14
22
16
11
12.56
0.1c
15
28
11
10
20
18
15
19
14.16
0.02
33.51
41.4
36.06
25.48
51.42
125.67
22.43
37.8
0.00001
0.00001
0.00002
0.0003
0.00001
0.000001
0.001
0.000001
a
Comparison of infection rate between seasons (within a village).
Comparison of infection rate between villages (within a season).
Not significant.
b
c
�1006
PHILIP SAMUEL ET AL.
700
652.2
600
523.9
521.9
Average PMH
500
400
300
363.2
353.7
294.3
249.3
244.8
200
166.9
143.2
156.8
100
58.61
Ju
l-S
ep
'0
3
O
ct
-D
ec
'0
3
Ja
nM
ar
'0
4
Ap
r-J
un
'0
4
Ju
l-S
ep
'0
4
O
ct
-D
ec
'0
4
Ja
nM
ar
'0
5
Ap
r-J
un
'0
5
Ju
l-S
ep
'0
5
O
ct
-D
ec
'0
5
Ja
nM
ar
'0
6
Ap
r-J
un
'0
6
0
Season
FIG. 1.
Abundance of Culex tritaeniorhynchus in different seasons in index villages. PMH, per man hour.
Vector susceptibility in different seasons showed a higher
IR of 13.22 geometric mean during the cool and wet season
(October–December), which coincided with peak transmission
season of JE, and a lower IR of 4.82 geometric mean during
nontransmission periods ( January–March). This suggests that
variations in infection during different seasons are mainly
responsible for transmission of JEV to humans (Table 1). Thus,
temporal changes might greatly impact the efficiency of arboviral transmission in nature, which would have significant
epidemiological importance as suggested by Hardy et al.
(1979) and Hayes et al. (1984).
In our study, IRs with respect to JEV were similar. Banerjee
et al. (1978) have reported similar results with lower IRs in JE
vectors. This may be due to the low virus titer and quantity in
the blood meal (Rosen et al. 1985) or due to the presence of
several anatomical or physiological barriers (Hardy et al.
1983, Weaver et al. 1984). However, it is suggested that the
variations in the susceptibility may be due to age distribution
of the vector mosquitoes.
Climate variability has a direct influence on the epidemiology of vector-borne diseases (Hardy et al. 1990, Githeko
et al. 2000). However, IRs recorded in our study did not show
any correlation with the rainfall, temperature, and humidity
during different seasons.
Cx. tritaeniorhynchus populations, despite close proximity
to each other, varied in their susceptibility to their JEV in
different seasons and years. Variations in susceptibility to
different arthropod viruses among geographic strains of different populations, including laboratory populations of
mosquitoes, had been already recorded in several parts of the
world (Gubler and Rosen 1976, Gubler et al. 1979, Banerjee
et al. 1983, 1988, Rosen et al. 1985, Boromisa et al. 1987,
Table 3. Analysis of Climatic Variations Against Japanese Encephalitis Virus Infection Rates
Variables
PMH
Statistical test=variables
Pearson correlation
coefficient
Sig. (two-tailed)
Infection rate Pearson correlation
coefficient
Sig. (two-tailed)
Maximum
Pearson correlation
temperature
coefficient
Sig. (two-tailed)
Minimum
Pearson correlation
temperature
coefficient
Sig. (two-tailed)
Rainfall
Pearson correlation
coefficient
Sig. (two-tailed)
Humidity
Pearson correlation
coefficient
Sig. (two-tailed)
a
PMH
Infection rate Maximum temperature Minimum temperature Rainfall Humidity
1
0.012
�0.634a
�0.728b
0.149
�0.091
0.012
0.97
1
0.027
0.073
0.007
�0.25
0.643
0.147
0.778
�0.065
0.97
�0.634a
0.073
0.822
1
0.433
0.465
0.648
�0.349
0.842
0.424
0.027
�0.728b
0.822
�0.25
0.465
0.128
1
0.266
�0.003
0.17
0.182
0.007
0.149
0.433
0.147
0.128
�0.349
�0.003
0.992
1
0.572
�0.743b
0.643
�0.091
0.648
�0.065
0.266
0.424
0.992
0.182
�0.743b
0.006
1
0.778
0.842
0.17
0.572
0.006
Correlation is significant at the 0.05 level (two-tailed).
Correlation is significant at the 0.01 level (two-tailed).
PMH, per man hour.
b
�SUSCEPTIBILITY STATUS OF Culex tritaeniorhynchus OF JEV
Vazeille et al. 2001, Mousson et al. 2002, Paupy et al. 2003).
We have not examined variation in the population=strain of
Cx. tritaeniorhynchus in the study area. However, we observed
significant variation in the oral susceptibility in the different
study villages. This may not be due to geographical variations
as all the index villages are located in one district. This variation in this survey may be due to the spatial variation in
larval habitat quality or density of vectors, which will affect
the competency of the adults from each index village.
Virus infection in vector mosquitoes also shows a seasonal
pattern. The improved understanding of this seasonality will
enhance the understanding of host–pathogen interactions and
will improve the accuracy of public health surveillance and
forecasting systems for the control of communicable diseases
and enhancement of preventive health interventions (Fisman
2007). There is a future need to find out the pathways of virus
infection and also to quantitatively evaluate the viral particles
present in different organs of the vector mosquitoes. The temporal and spatial changes influenced the JEV infection in vector
mosquitoes and this would have played a role in the occurrence
of seasonality in JEV cases in the endemic study area.
Acknowledgments
The authors are grateful to the Director General, Indian
Council of Medical Research, for his support and encouragement in conducting this study. The authors express thanks
to the staff members of the Centre for Research in Medical
Entomology, Field Station, Vriddachalam, for their excellent
technical assistance in laboratory and field work; to S.C.
Tewari, for reviewing the manuscript; and to K. Venkatsubramani and A. Venkatesh, for DTP work. The authors are
thankful to the Department of Science and Technology,
Ministry of Science and Technology, Government of India,
New Delhi, for funding this project (SP=SO=C-47=2001).
Disclosure Statement
No competing financial interests exist.
References
Banerjee, K, Deshmukh, PK, Ilkal, MA, Dhanda, V. Transmission
of Japanese encephalitis virus by Culex bitaeniorhynchus Giles.
Indian J Med Res 1978; 67:889–893.
Banerjee, K, Deshmukh, PK, Ilkal, MA, Dhanda, V. Comparative
susceptibility of three species of mosquitoes to infection with
Japanese encephalitis virus. Indian J Med Res 1983; 78:603–
606.
Banerjee, K, Mishra, AC, Bhat, HR. Experimental transmission of
Japanese encephalitis virus by Culex vishnui Theobald. Indian J
Med Res 1984; 79:303–306.
Banerjee, K, Mourya, DT, Malunjkar, AS. Susceptibility and
transmissibility of different geographical strains of Aedes aegypti mosquitoes to Chickungunya virus. Indian J Med Res
1988; 87:134–138.
Boromisa, RD, Karamjit, SR, Grimstad, PR. Variation in the
vector competence of geographic strains of Aedes albopictus for
dengue 1 virus. J Am Mosq Control Assoc 1987; 3:378–386.
Fisman, DN. Seasonality of infectious diseases. Annu Rev Public
Health 2007; 28:127–143.
Freier, JE, Grimstad, PR. Transmission of dengue virus by orally
infected Aedes triseriatus. Am J Trop Med Hyg 1983; 32:1429–1434.
1007
Gajanana, A. Epidemiology and surveillance of Japanese encephalitis in Tamil Nadu. ICMR Bull 1998; 28:33–37.
Gajanana, A, Rajendran, R, Philip Samuel, P, Thenmozhi, V, et al.
Japanese encephalitis in South Arcot district, Tamil Nadu: a
three-year longitudinal study of vector abundance and infection frequency. J Med Entomol 1997; 34:651–659.
Gajanana, A, Rajendran, R, Thenmozhi, V, Philip Samuel, P,
et al. Comparative evaluation of bioassay and ELISA for detection
of Japanese encephalitis virus in field collected mosquitoes.
Southeast Asian J Trop Med Public Health 1995; 26:91–97.
Githeko, AK, Lindsay, SW, Confalonieri, UE, Patz, JA. Climate
change and vector-borne diseases a regional analysis. Bull
WHO 2000; 78:1136–1147.
Gubler, DJ, Nalim, S, Tav, R, Saipan, H, Sulianti Soroso, J.
Variations in susceptibility to oral infection with dengue
viruses among geographic strains of Ae. aegypti. Am J Trop
Med Hyg 1979; 28:1045–1052.
Gubler, DJ, Rosen, L. Variation among geographic strains of
Aedes albopictus in susceptibility to infection with Dengue
viruses. Am J Trop Med Hyg 1976; 25:318–325.
Hardy, JL, Houk, EJ, Kramer, LD, Reeves, WC. Intrinsic factors
affecting vector competence of mosquitoes for arboviruses.
Annu Rev Entomol 1983; 28:229–262.
Hardy, JL, Meyer, RP, Presser, SB, Milby, MM. Temporal variation in the susceptibility of a semi-isolated population of
Culex tarsalis to per oral infection with Western equineencephalomyelitis and St. Louis encephalitis viruses. Am J
Trop Med Hyg 1990; 42:500–511.
Hardy, JL, Reeves, WC, Bruen, JP, Presser, SB. Vector competence of Culex tarsalis and other mosquito species for Western
equine encephalomyelitis virus. Arctic Trop Arbovirus 1979;
10:157–171.
Hayes, CG, Baker, RH, Baqar, S, Ahmed, T. Genetic variation for
West Nile virus susceptibility in Culex tritaeniorhynchus. Am J
Trop Med Hyg 1984; 33:715–724.
Kanojia, PC, Shetty, PS, Geevarghese, G. A long-term study on
vector abundance & seasonal prevalence in relation to the
occurrence of Japanese encephalitis in Gorakhpur district,
Uttar Pradesh. Indian J Med Res 2003; 117:104–110.
Kumar, R. Japanese encephalitis in India. Indian Pediatr 1988;
25:354–360.
Mousson, L, Vazeille, NM, Chawprom, S, Prajakwong, S, et al.
Genetic structure of Aedes agypti populations in China Mai
(Thailand) and relation with dengue transmission. Trop Med
Int Health 2002; 7:865–872.
Paupy, C, Vazeille, NM, Reynes, JM, Rodhain, F, Failloux, AB.
Variation over space and time of Aedes aegypti in phnom penh
(Cambodia): Genetic structure and oral susceptibility to a
dengue virus. Genet Res 2003; 82:171–182.
Philip Samuel, P, Hiriyan, J, Gajanana, A. Japanese encephalitis
virus infection in mosquitoes and its epidemiological implications. ICMR Bull 2000; 30:37–43.
Philip Samuel, P, Hiriyan, J, Thenmozhi, V, Balasubramanian, A.
A system for studying vector competence of mosquitoes for
Japanese encephalitis virus. Indian J Malariol 1998; 35:146–150.
Reisen, WK, Hardy, JL, Presser, SB, Chiles, RE. Seasonal variations in the vector competence of Culex tarsalis (Diptera: Culicidae) from the Coachella Valley of California for Western
equine encephalomyelitis and St. Louis encephalitis vectors.
J Med Entomol 1996; 33:433–437.
Reuben, R, Gajanana, A. Japanese encephalitis in India. Indian
J Paediatr 1997; 64:243–251.
Reuben, R, Kaul, HN, Soman, RS. Mosquitoes of arboviral importance in India. Mosq Borne Dis Bull 1988; 5:48–54.
�1008
Reuben, R, Tewari, SC, Hiriyan, J, Akiyama, J. Illustrated keys to
species of Culex (Culex) associated with Japanese encephalitis in
Southeast Asia (Diptera: Culicidae). Mosq Syst 1994; 26:75–96.
Rosen, L, Roseboom, LE, Gubler, DJ, Lien, JC, Chaniotis, BN.
Comparative susceptibility of mosquito species and strain to
oral and parenteral infection with dengue and Japanese encephalitis viruses. Am J Trop Med Hyg 1985; 34:603–815.
Solomon, T, Vaughn, DW. Pathogenesis and clinical features of
Japanese encephalitis and West Nile virus infections. Curr
Trop Microbiol Immunol 2002; 267:171–194.
Srivastava, VK, Sinha, NK, Singh, A, Chandra, R. Japanese encephalitis situation in Gorakhpur division, UP. J Commun Dis
2003; 35:56–58.
Tewari, SC, Thenmozhi V, Arunachalam N, Philip Samuel P,
Tyagi BK. Desiccated vector mosquitoes used for the surveillance of Japanese encephalitis virus activity in endemic
southern India. Trop Med Int Health 2008; 13:286–290.
Vazeille, M, Mousson, L, Rakatoarivony, I, Villeret, R, et al.
Population genetic structure and competence as a vector for
PHILIP SAMUEL ET AL.
dengue type 2 virus of Aedes aegypti and Aedes albopictus from
Madagascar. Am J Trop Med Hyg 2001; 65:491–497.
Weaver, SC, Scherer, WF, Cupp, EW, Castello, DA. Barriers to
dissemination of Venezuelan encephalitis viruses in the middle American enzootic vector mosquito, Culex (Melanoconion)
taeniopus. Am J Trop Med Hyg 1984; 33:953–960.
Address correspondence to:
B.K. Tyagi
Centre for Research in Medical Entomology
Indian Council of Medical Research
4, Sarojini Street
Chinna Chokkikulam
Madurai
Tamil Nadu 625002
India
E-mail: crmeicmr@icmr.org.in
�
 Victorjerald Leo
Victorjerald Leo