Mucoepidermoid Carcinoma of the External
Auditory Canal: Case Report
Giuseppe Magliulo, MD, Massimo Fusconi, MD, and Gianna Pulice, MD
This study reports a case of mucoepidermoid carcinoma (MEC) of the external auditory
canal, which to date has only been described once in literature. Because the lesion is
extremely rare, it is particularly difficult to classify it into stages following normal diagnostic
parameters. This obviously limits the possibilities of treatment that consequently are either
empirical or based on those of squamous cell carcinoma. The problems in the diagnosis and
the possible methods of treatment of mucoepidermoid carcinoma are discussed.
(Am J Otolaryngol 2003;24:274-277. © 2003 Elsevier Inc. All rights reserved.)
Neoplastic lesions of the external auditory
canal (EAC) are quite rare. In fact they occur
in 1 or 2 cases in 5 million people and affect in
particular those between 50 and 60 years of
age.1-3
In the past the term ceruminoma comprehended benign and malignant tumors of the
EAC whether they were of epithelial or glandular origin.4 Recently, the Armed Forces Institute of Pathology (Bethesda, MD, 1991) and
the World Health Organization have reclassified the histological pathologies, forming a
new simplified version in substitution of the
old method. Squamous cell carcinomas followed by adenoidal cystic carcinomas and
basaliomas are respectively the most frequent
forms of tumor,5 whereas mucoepidermoid
tumors are extremely rare. From a thorough
review of the literature available, we found
that only 4 cases of this type of tumor have
been reported, and of these only 1 was situated in the EAC.6-9 The aim of this study is to
present a second case of mucoepidermoid carcinoma (MEC) of the EAC that are diagnosed
and treated surgically and to propose the possible methods of diagnosis and treatment.
From the Department of Otorhinolaryngology, Audiology and Phoniatrics, Giorgio Ferreri, La Sapienza University, Rome, Italy.
Address correspondence to: Massimo Fusconi, MD,
Via R. D’Aronco, 18 00163, Rome, Italy. E-mail:
massimo.fusconi@libero.it.
© 2003 Elsevier Inc. All rights reserved.
0196-0709/03/2404-0000$30.00/0
doi:10.1016/S1096-0709(03)00056-5
274
CASE REPORT
A 62-year-old woman was seen in March
2000 complaining of slight left-sided otalgia.
The patient stated that she had 2 small lumps
that she felt during palpation of the EAC and
that they had been present for about 6 years.
On otoscopy, they were seen to be bright red
in color, situated on the inferior wall of the
cartilaginous portion of the EAC, and less
than 8 mm in size. They caused her some
pain, which slightly increased on palpation. A
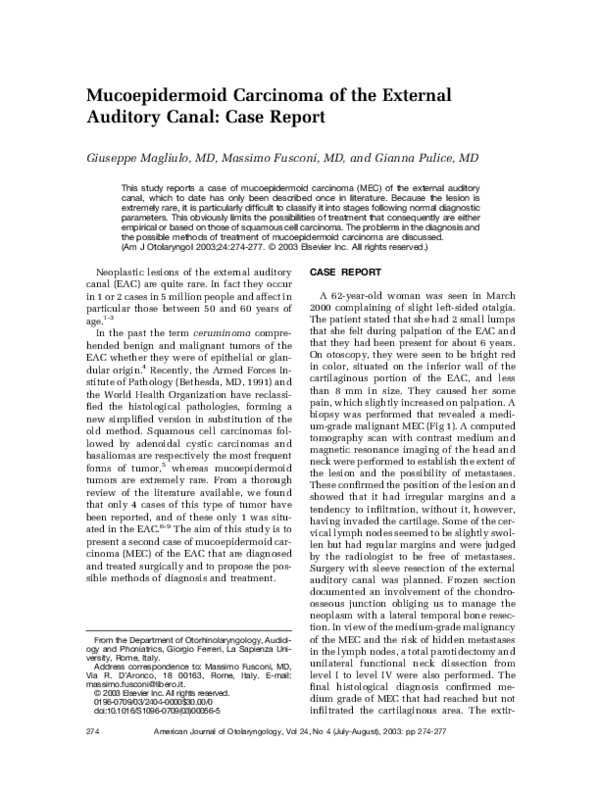
biopsy was performed that revealed a medium-grade malignant MEC (Fig 1). A computed
tomography scan with contrast medium and
magnetic resonance imaging of the head and
neck were performed to establish the extent of
the lesion and the possibility of metastases.
These confirmed the position of the lesion and
showed that it had irregular margins and a
tendency to infiltration, without it, however,
having invaded the cartilage. Some of the cervical lymph nodes seemed to be slightly swollen but had regular margins and were judged
by the radiologist to be free of metastases.
Surgery with sleeve resection of the external
auditory canal was planned. Frozen section
documented an involvement of the chondroosseous junction obliging us to manage the
neoplasm with a lateral temporal bone resection. In view of the medium-grade malignancy
of the MEC and the risk of hidden metastases
in the lymph nodes, a total parotidectomy and
unilateral functional neck dissection from
level I to level IV were also performed. The
final histological diagnosis confirmed medium grade of MEC that had reached but not
infiltrated the cartilaginous area. The extir-
American Journal of Otolaryngology, Vol 24, No 4 (July-August), 2003: pp 274-277
�MUCOEPIDERMOID CARCINOMA
Fig 1. Hematoxylin eosin staining (original magnification 25ⴛ). Both the epidermoid and mucous components are clearly shown.
pated parotid parenchyma was free of neoplastic infiltration, whereas one of the lymph
nodes from the functional neck dissection
(level I) showed signs of metastases. The patient has been seen repeatedly since surgery
and in the 2-year follow-up period has shown
no signs of relapse.
DISCUSSION
MECs are malignant tumors that frequently
originate in the mayor and minor salivary
glands (11% and 8%, respectively).10 They
may also occur in other glandular structures
in their normal anatomic sites such as the
anal, esophageal, tracheobronchial mucous
glands, and the biliary and ceruminous duct,
or they may arise in ectopic sites such as the
hypophysis, the mandible, and the neck.9
The ceruminous glands are known to be
situated in the deep dermis of the EAC. The
mechanism that provokes tumoral degeneration is not clearly understood, but Soh et al9
have advanced 4 etiopathogenetic hypotheses: those originating from the seromucous
glands because of metastatic or functional alterations of the mucosal epithelium, those
caused by chronic irritation that causes squamous metaplasia of the mucosa, seromucous
and minor salivary glands implanted in the
ear during embryogenesis, and finally those
caused by secondary invasion of a tumor located in an adjacent primary site. Each single
hypothesis is valid and reliable on its own but
the possibility that they may act together
275
should also be taken into consideration. Soh
et al’s9 interpretations of glandular tumors of
both the middle and external ear clearly also
applies to MECs. In the case of the latter, the
only possible means of diagnosis is histological. Under histological examination, MECs
appear to be composed of scattered solid and
cystic mucinous areas. In the solid parts, the
cells are arranged in nests, are tubular in
structure, and have different characteristics
very similar to those of mucous squamous
cells, whereas other cells have intermediate
histopathological characteristics. It is exactly
this percentage of the different cells that
makes it possible to establish a low-, medium-,
or high-grade malignancy. In low-grade tumors, there is a higher percentage of mucous
cells, and, in high-grade tumors of squamous
cells and in medium-grade tumors, there is an
equal percentage of glandular and epithelial
cells. The histological diagnosis of MECs is
often difficult and not always completely reliable. For example, low-grade MECs may be
confused with adenomas because they have a
low mitotic rate and very little atypia; thus,
the diagnosis of MEC may be established only
if intermediate and epithelioid cells are
present. High-grade MECs instead are very
similar to poorly differentiated squamous carcinoma except for the fact that the former has
intermediate and mucin-secreting cells, a difference that gives a useful indication in the
histological diagnosis. The clinical diagnosis
is based on classical otoscopy. MECs do not
particularly differ from other neoplasms
found in the external auditory canal. They
appear as solid reddish masses that are variable in shape (usually irregular) and may be
located in any part of the EAC. They are normally neither painful nor tender, but pain is
sometimes present as a result of concomitant
infection, compression (as in our case), or
infiltration of the nerves. Imaging techniques
serve to establish the extent of the lesion and
to assess possible metastatic involvement of
the lymph nodes. Their informations are essentially not specific. The images of highgrade malignant tumors both on computed
tomography scan and magnetic resonance imaging are identical to those of other malignant
neoformations in the EAC with irregular infiltrating margins. Moreover, low-grade malignant tumors with a regular surface and well-
�276
MAGLIULO, FUSCONI, AND PULICE
TABLE 1. Review of the Literature
TNM
Grade of
Malignancy
Authors
Site
Kinney and Wood (1987)
External auditory canal
n.p.
high
Landman and Farmer
(1991)
Posterior mid helix
T1N0M0
low
Shotton et Al. (1993)
Cheek involving ear
T4N0M0
n.p.
Soh et Al. (1996)
Middle ear
T4N1M0
n.p.
circumscribed margins are very similar in
appearance to benign lesions.11 The very fact
that MECs in the EAC are extremely rare
makes it highly difficult if not impossible to
establish a reliable system of classification
into stages. In fact, of the 4 cases of MECs in
the ear described in literature, only 1 reported
by Kinney and Wood6 involved the EAC (Table 1).
The lack of precise guidelines in the classification and treatment of this form of tumor
obliged us to adopt the same criteria for squamous cell carcinomas of the external auditory
canal. Several methods of classification do
exist; however, the one proposed by Pittsburgh University, that is a combination of the
clinical and imaging technique results before
surgery, has recently come to be considered
the most useful (Table 2). 12
Our case involved the chondro-osseous
junction and may be classified as a T2. Because the algorithm for high-grade squamous
TABLE 2.
T1
T2
T3
T4
N status
M status
Treatment
Follow-up
(months)
Ear canal resection
⫹ superficial
parotidectomy
resection
Excision by Mohs
surgical
technique
Superficial
parotidectomy ⫹
external
radiotherapy
Radiotherapy (not
specified
Outcome
18
Persistent
disease
8
Free from
disease
0
Dead
13
Dead
cell carcinomas indicates partial lateral temporal bone resection, the same form of surgery
also applies to this form of lesion. This modality is combined with functional neck dissection in those cases in which these are involved. The effective necessity of the latter
form of surgery is based on the results of the
preoperative imaging techniques, but these
unfortunately are somewhat unreliable and
give rise to doubt because they do not always
clearly manifest nodal involvement. At this
point, it should be kept in mind that metastases of the lymph nodes indicates a worse
prognosis and automatically puts the patients
into the category of advanced lesions. Furthermore, as Jesse et al13 already stressed, the first
form of surgical treatment of malignant neoplasms of the EAC must necessarily be radical
because subsequent surgery is virtually ineffective and only palliative. It is therefore particularly important to adopt a highly aggressive strategy at the very beginning. We
University of Pittsburgh Staging System for Squamous Cell Carcinoma of the Temporal Bone and Stage
Tumour limited to the external auditory canal without bony erosion or evidence of soft-tissue
extension
Tumour with limited external auditory canal erosion (not full thickness) or radiologic findings consistent
with limited (⬍0.5 cm) soft-tissue involvement
Tumour eroding the osseous external auditory canal (full thickness) with limited (⬍0.5 cm) soft tissue
involvement, or involving middle ear and/or mastoid or causing facial paralysis at presentation
Tumour eroding the cochlea, petrous apex, medial wall of middle ear, carotid canal, jugular foramen,
or dura, or with extensive (⬎0.5 cm) soft-tissue involvement
Involvement of lymph nodes is a poor prognostic finding and automatically places the patient in a
higher category (ie, stage III (T1, N1) or stage IV (T2,3,4, N1)
M1 immediately places a patient in the stage IV category
�MUCOEPIDERMOID CARCINOMA
performed functional neck dissection even
though the results of the imaging scans were
negative, basing our decision on the histological appearance of the lesion. The tumor in
question was a medium-grade MEC with a
high potential risk of metastasis. The final
histological examination proved our choice to
be right. Although it is not possible to draw
final conclusions, it would, however, seem
reasonable not to postpone lymph node dissection when the surgeon is faced with a clinically and histologically proved highly aggressive squamous cell or mucoepidermoid
tumour.
Alternative measures would only apply to
low-grade MECs. In these cases, lymph node
dissection could be delayed, but in the meantime the patient should be kept under close
surveillance. Because of the clinical features
of the MEC described in this study, we are not
in a position to be able to judge the validity of
postoperative radiotherapy. It would, however, seem logical to reserve this form of treatment for the particularly aggressive forms of
tumor.
REFERENCES
1. Arena S, Keen M: Carcinoma of the middle ear and
temporal bone. Am J Otol 9:351-356, 1988
277
2. Conley JJ: Cancer of the middle ear and temporal
bone. NY State J Med 9:1575-1579, 1974
3. Morton RP, Stell PM, Derrick PPO: Epidemiology of
cancer of the middle ear cleft. Cancer 53:1612-1621, 1984
4. Wetli CV, Pardo V, Millard M: Tumours of ceruminous glands. Cancer 29:1169-1178, 1972
5. Kuhel WI, Hume CR, Selesnick SH: Cancer of the
external auditory canal and temporal bone. Otolaryngol
Clin North Am 20:5829-5851, 1996
6. Kinney SE, Wood BG: Malignancies of the external
ear canal and temporal bone: surgical techniques and
results. Laryngoscope 97:158-164, 1987
7. Landman G, Farmer ER: Primary cutaneous mucoepidermoid carcinoma. J Cutan Pathol 18:56-59, 1991
8. Shotton JC, Sergeant RJ, Tanner NS, et al: Lateral
temporal bone resection for extensive pinnal malignancy.
Has anything changed in forty years? J Laryngol Otol
107:697-702, 1993
9. Soh KB, Tan HK, Sinniah R: Mucoepidermoid carcinoma of the middle ear-a case report. J Laryngol Otol
110:249-251, 1996
10. Gates GA: Current concepts in otolaryngology: Malignant neoplasms of the minor salivary glands. N Engl
J Med 306:718-722, 1982
11. Kim H, Han MH, Park SW, et al: Radiologicpathologic correlation of unusual lingual masses: Part
II: Benign and malignant tumors. Korean J Radiol 2:42-51,
2001
12. Arriaga M, Curtin H, Takahashi H, et al: Staging
proposal for external auditory meatus carcinoma based
on preoperative clinical examination and computer tomography findings. Ann Otol Rhinol Laryngol 90:714721, 1990
13. Jesse RH, Healey JE, Wiley DB: External auditory
canal, middle ear and mastoid. in Mac Lombey WS,
Fletcher GA, (eds): Cancer of the Head and Neck. Baltimore, MD , Williams & Wilkins, 1967
�
 Monica Garcia
Monica Garcia